-
PDF
- Split View
-
Views
-
Cite
Cite
Yassine Saadi, Alae Neqrachi, Moncif Boufettal, Rida-Allah Bassir, Mohamed Kharmaz, Mohamed Saleh Berrada, Surgical treatment of Hahn–Steinthal fracture using Herbert screws, Journal of Surgical Case Reports, Volume 2023, Issue 12, December 2023, rjad673, https://doi.org/10.1093/jscr/rjad673
Close - Share Icon Share
Abstract
Hahn–Steinthal fractures are rare and often neglected. Their initial management should be early, given the relatively high complication rate. We report eight cases of type I capitellum fractures treated by Herbert screw fixation. Between 2019 and 2022, we selected eight patients (six men and two women) with a mean age of 25 years (18–40 years). The mean follow-up was 2 years (1–3 years). Clinical results were assessed using the Mayo Clinic Elbow Performance Score (MEPS). The mean arc of mobilitý was 135° (105°–150°) for flexion/extension and 161° (150°–175°) for pronosupination. The mean MEPS was 90.6 points, with seven excellent results and one good result. The aim of this study was to highlight the good results of Herbert screw fixation technique in the management of Hahn–Steinthal fractures.
Introduction
Hahn–Steinthal fracture is defined as type fracture of the capitellum based on Bryan and Morrey classification modified by McKee [1, 2]. They account for 1% of all elbow fractures and 6% of humerus fractures. Often missed, their diagnosis is based on a good quality lateral X-ray of the elbow. Their initial management should be early, given the relatively high complication rate. Treatment options include: excision of small unfixable fragments, closed reduction, open reduction with different fixations, and prosthetic replacement. The purpose of this study was to evaluate the clinical outcomes of type I capitellum fractures treated by Herbert screws placed in an anterior -to- posterior technique.
Methods
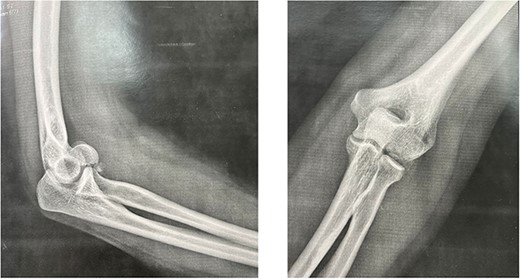
This is a prospective, monocentric study of adult patients undergoing surgical treatment for isolated capitellar fracture. Between 2019 and 2022, we received eight patients (six men and two women) with a mean age of 25 years (18–40 years) who had type I fracture of the capitellum. The dominant arm was affected in six patients (Table 1). All our patient had a fall on an outstretched hand. All fractures were close and isolated without any vascular or neurological damage. Standard AP (anteroposterior), lateral X-rays (Fig. 1) as well as a computed tomography (CT) scan with 3D reconstruction were done for all the patients (Fig. 2). Therefore, fractures with trochlea involvement were excluded.
| . | Age . | Sex . | Site . | Follow up (months) . | Operation delay (hours) . | Postoperative range of motion (Arc°) Pro/Supi . | Postoperative pain . | Postoperative MEPI* score . | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 18 | M | D | 12 | 4 | 150 | 175 | None | 100 |
| 2 | 20 | M | D | 13 | 6 | 130 | 180 | None | 100 |
| 3 | 20 | M | D | 35 | 10 | 140 | 155 | None | 95 |
| 4 | 23 | M | D | 20 | 15 | 145 | 145 | None | 80 |
| 5 | 25 | M | D | 24 | 8 | 135 | 160 | None | 85 |
| 6 | 26 | M | ND | 32 | 7 | 125 | 155 | None | 90 |
| 7 | 35 | F | ND | 29 | 10 | 120 | 165 | None | 95 |
| 8 | 40 | F | D | 40 | 72 | 105 | 150 | Mild | 80 |
| . | Age . | Sex . | Site . | Follow up (months) . | Operation delay (hours) . | Postoperative range of motion (Arc°) Pro/Supi . | Postoperative pain . | Postoperative MEPI* score . | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 18 | M | D | 12 | 4 | 150 | 175 | None | 100 |
| 2 | 20 | M | D | 13 | 6 | 130 | 180 | None | 100 |
| 3 | 20 | M | D | 35 | 10 | 140 | 155 | None | 95 |
| 4 | 23 | M | D | 20 | 15 | 145 | 145 | None | 80 |
| 5 | 25 | M | D | 24 | 8 | 135 | 160 | None | 85 |
| 6 | 26 | M | ND | 32 | 7 | 125 | 155 | None | 90 |
| 7 | 35 | F | ND | 29 | 10 | 120 | 165 | None | 95 |
| 8 | 40 | F | D | 40 | 72 | 105 | 150 | Mild | 80 |
*MEPI: Mayo Elbow Performance Index.
D: dominant; ND: non dominant; Ext/Flex: extension / flexion; Pro /supi: pronation /supination
| . | Age . | Sex . | Site . | Follow up (months) . | Operation delay (hours) . | Postoperative range of motion (Arc°) Pro/Supi . | Postoperative pain . | Postoperative MEPI* score . | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 18 | M | D | 12 | 4 | 150 | 175 | None | 100 |
| 2 | 20 | M | D | 13 | 6 | 130 | 180 | None | 100 |
| 3 | 20 | M | D | 35 | 10 | 140 | 155 | None | 95 |
| 4 | 23 | M | D | 20 | 15 | 145 | 145 | None | 80 |
| 5 | 25 | M | D | 24 | 8 | 135 | 160 | None | 85 |
| 6 | 26 | M | ND | 32 | 7 | 125 | 155 | None | 90 |
| 7 | 35 | F | ND | 29 | 10 | 120 | 165 | None | 95 |
| 8 | 40 | F | D | 40 | 72 | 105 | 150 | Mild | 80 |
| . | Age . | Sex . | Site . | Follow up (months) . | Operation delay (hours) . | Postoperative range of motion (Arc°) Pro/Supi . | Postoperative pain . | Postoperative MEPI* score . | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 18 | M | D | 12 | 4 | 150 | 175 | None | 100 |
| 2 | 20 | M | D | 13 | 6 | 130 | 180 | None | 100 |
| 3 | 20 | M | D | 35 | 10 | 140 | 155 | None | 95 |
| 4 | 23 | M | D | 20 | 15 | 145 | 145 | None | 80 |
| 5 | 25 | M | D | 24 | 8 | 135 | 160 | None | 85 |
| 6 | 26 | M | ND | 32 | 7 | 125 | 155 | None | 90 |
| 7 | 35 | F | ND | 29 | 10 | 120 | 165 | None | 95 |
| 8 | 40 | F | D | 40 | 72 | 105 | 150 | Mild | 80 |
*MEPI: Mayo Elbow Performance Index.
D: dominant; ND: non dominant; Ext/Flex: extension / flexion; Pro /supi: pronation /supination

The mean operative delay was 16 hours (4–72). One of the patients had a 3 days delay, because the diagnosis was initially missed and had to come back, for persistent pain.
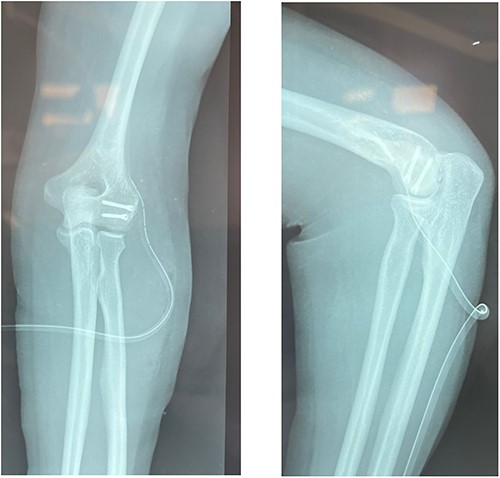
In a supine position, under regional anesthesia and with an upper limb tourniquet, the fracture was approached through a lateral Kocher approach. After exposing the capitulum, the fracture site was cleared of any hematoma or loose pieces of bone. Inspection of the joint found no intraarticular extension of the fracture. Temporary fixation was obtained by using two guide wires for the cannulated headless screws and checked with image intensification. The position of the wire should be as perpendicular as possible to the fracture line. After anterior to posterior drilling, Herbert screws were inserted. A last check for fracture stability under visual inspection (Fig. 3) as well as under image intensification was done (Fig. 4).

The tourniquet was deflated, and the skin was closed and a compressive dressing was placed after the hemostasis was revised. The procedure lasted for about 90 minutes and there were no complications. A brachio palmar splint was kept in place for 2 weeks before initiating passive rehabilitation. Muscle-strengthening exercises began at week 8 and continued until week 12. Patients were allowed to participate in simple sports activities from the sixth postoperative month.
Follow-up was done at 2 weeks, 1 month, and then monthly for another 6 months.
Clinical results were assessed using the Mayo Clinic Elbow Performance Score (MEPS) (Table 2) [3]. Osteoarthritic progression was assessed according to the Bröberg and Morrey classification (Table 3) [3].
| Mayo Elbow Performance Score . | |||
|---|---|---|---|
| Pain (45 pts) | None (45 pts) Mild (15pts) | Moderate (30 pts) Severe (0) | /45 |
| Range of motion (20 pts) | >100° (20 pts) Arc <50° (5 pts) | 50° to 100° (15 pts) | /20 |
| Stability (10 pts) | Stable (10 pts) Instable (laxity >10°) (0 pt) | Moderate instability (5 pts) | /10 |
| Daily function (25 pts) | Hand-mouth = feeding (5 pts) Dressing (5 pts) | Head hand = Combing hair (5 pts) Hygiene (5 pts) Shoeing (5 pts) | /25 |
| Index | Interpretation | ||
| >90 75–89 60–74 <60 | Excellent Good Fair Poor | ||
| Mayo Elbow Performance Score . | |||
|---|---|---|---|
| Pain (45 pts) | None (45 pts) Mild (15pts) | Moderate (30 pts) Severe (0) | /45 |
| Range of motion (20 pts) | >100° (20 pts) Arc <50° (5 pts) | 50° to 100° (15 pts) | /20 |
| Stability (10 pts) | Stable (10 pts) Instable (laxity >10°) (0 pt) | Moderate instability (5 pts) | /10 |
| Daily function (25 pts) | Hand-mouth = feeding (5 pts) Dressing (5 pts) | Head hand = Combing hair (5 pts) Hygiene (5 pts) Shoeing (5 pts) | /25 |
| Index | Interpretation | ||
| >90 75–89 60–74 <60 | Excellent Good Fair Poor | ||
| Mayo Elbow Performance Score . | |||
|---|---|---|---|
| Pain (45 pts) | None (45 pts) Mild (15pts) | Moderate (30 pts) Severe (0) | /45 |
| Range of motion (20 pts) | >100° (20 pts) Arc <50° (5 pts) | 50° to 100° (15 pts) | /20 |
| Stability (10 pts) | Stable (10 pts) Instable (laxity >10°) (0 pt) | Moderate instability (5 pts) | /10 |
| Daily function (25 pts) | Hand-mouth = feeding (5 pts) Dressing (5 pts) | Head hand = Combing hair (5 pts) Hygiene (5 pts) Shoeing (5 pts) | /25 |
| Index | Interpretation | ||
| >90 75–89 60–74 <60 | Excellent Good Fair Poor | ||
| Mayo Elbow Performance Score . | |||
|---|---|---|---|
| Pain (45 pts) | None (45 pts) Mild (15pts) | Moderate (30 pts) Severe (0) | /45 |
| Range of motion (20 pts) | >100° (20 pts) Arc <50° (5 pts) | 50° to 100° (15 pts) | /20 |
| Stability (10 pts) | Stable (10 pts) Instable (laxity >10°) (0 pt) | Moderate instability (5 pts) | /10 |
| Daily function (25 pts) | Hand-mouth = feeding (5 pts) Dressing (5 pts) | Head hand = Combing hair (5 pts) Hygiene (5 pts) Shoeing (5 pts) | /25 |
| Index | Interpretation | ||
| >90 75–89 60–74 <60 | Excellent Good Fair Poor | ||
| Grade 0: normal joint space Grade 1: narrowing <50% ± osteophytes Grade 2: narrowing >50% + osteophytes Grade 3: complete narrowing + osteophytes |
| Grade 0: normal joint space Grade 1: narrowing <50% ± osteophytes Grade 2: narrowing >50% + osteophytes Grade 3: complete narrowing + osteophytes |
| Grade 0: normal joint space Grade 1: narrowing <50% ± osteophytes Grade 2: narrowing >50% + osteophytes Grade 3: complete narrowing + osteophytes |
| Grade 0: normal joint space Grade 1: narrowing <50% ± osteophytes Grade 2: narrowing >50% + osteophytes Grade 3: complete narrowing + osteophytes |
Results
The mean follow-up was 2 years (1–3 years). The mean arc of mobilitý in flexion/extension and pronation/supination was 135° (105°–150°) and 161° (150°–175°), respectively. The mean MEPS was 90.6 points, with seven excellent results and one good result. Radiological signs of consolidation were partial at 5 weeks and complete at 2 months. No cases of pseudarthrosis, avascular necrosis, infection, instability, or arthrosis were noted in our series. On last follow up, all patients returned to previous levels of functioning and had no residual pain.
Discussion
The Hahn–Steinthal fracture or type I capitellum fracture is a rare articular fracture of the lower end of the humerus with a frontal line. They are not well studied, and the literature reports only small series [4]. The vast majority of published cases, as in our case, concern adults and adolescents older than 12 years [5]. Most authors suggest an indirect injury mechanism involving a fall onto the hand with the elbow in extension [6], classically responsible for a supra-condylar fracture. However, in the adolescent, the center of rotation of the capitellum is located around 15 mm anterior to the humeral shaft, making it vulnerable to compressive forces transmitted by the radial head during the fall. This would explain the frequent association with a radial head fracture [7]. Diagnosis is primarily radiological. An AP view is often not very suggestive. Good-quality lateral views are the key to diagnosis [2, 4, 5]. CT with elbow reconstruction better defines the medial extension of the fracture line, and helps rule out any progression to the trochlea [8]. In the specific case of Hahn–Steinthal fractures, several therapeutic methods have been described: reduction by external maneuvers, resection of the fragment, open reduction with osteosynthesis, and prosthetic replacement. All these methods have been well described, with no known studies directly comparing their clinical outcomes [9]. Orthopedic reduction has been performed in few patients, but has the disadvantage of long immobilization and poor functional results [10–12]. This is explained by the difficulty to maintain anatomic and stable reduction to restore the articular congruity. Many authors recommend resection of the avulsed fragment in Hahn–Steinthal fractures [13–15] as it is a simple procedure with no risks of osteonecrosis or non-union. But subsequently it exposes the patient to joint stiffness and elbow instability. This technique should be therefore limited to small unfixable fragments.
These reflections had led many surgeons to adopt an open reduction with different fixation techniques: bone suture [16], Kirschner wires [17], fibrin glue [18], bioabsorbable rods [19], or metallic screws [17, 20, 21]. The choice depends on: complexity of fracture, implants availability, and the surgeon’s habits. Regardless of the type of fixation we believe that the most important thing is to achieve an accurate anatomic reduction and a stable fixation avoiding dissection of the posterolateral column of the humerus so as not to compromise the vascular supply of the humeral condyle leading to high risk of osteonecrosis [22].
Like most authors, we have performed an open reduction and internal fixation using Herbert screws, used from posterior to anterior. Some authors prefer poster to anterior insertion to prevent further violation of the anterior articular cartilage [23].
The buried nature of Herbert screws preserves the integrity of the articular surface and prevents joint impingement, while maintaining an effective compression effect, allowing therefore patients to start functional exercise early after surgery.
Compared with other treatments described in the literature, we reported no cases of stiffness or osteoarthritis, and no need for material removal.
Conclusion
We recommend open reduction and internal fixation with Herbert screws for the treatment of Hahn–Steinthal fractures. Using an anterior to posterior insertion, this procedure leads to minimal articular damage and rigid fixation, as well as early mobilization. It also offers excellent clinical outcomes, including minimal to no residual pain, and a return to previous levels of functioning.
Conflict of interest statement
None declared.
Funding
None declared.



