-
PDF
- Split View
-
Views
-
Cite
Cite
Nimetula Limani, Shqipe Misimi, Andrej Nikolovski, Large biloma as the initial presentation of gallbladder perforation: a case report and literature review, Journal of Surgical Case Reports, Volume 2023, Issue 12, December 2023, rjad669, https://doi.org/10.1093/jscr/rjad669
Close - Share Icon Share
Abstract
Biloma is an encapsulated intra or extra-hepatic collection of bile after biliary tree trauma. Post-procedural and traumatic biliary damage are the most common etiologic causes. Gallbladder perforation due to acute cholecystitis rarely presents with biloma occurrence. We present a case of large extrahepatic biloma formation as a consequence of a perforated gallbladder.
Introduction
Biloma is a medical term used to describe the occurrence of an encapsulated collection of bile either inside or outside the biliary system. Its occurrence is described to be related to acute cholecystitis, iatrogenic injury (endoscopic or laparoscopic procedures), and abdominal trauma. The reported overall incidence of biloma is 0.3–2% [1]. Gallbladder perforation due to acute cholecystitis presents with an incidence of 2–11% [2]. Still, the initial presentation of gallbladder perforation with biloma occurrence is extremely rare. We report a case of a 70-year-old female patient with a large biloma as the initial presentation of calculous acute cholecystitis following gallbladder perforation. Written informed consent was obtained from the patient regarding this case report.
Case report
A 70-year-old female patient was transferred to our emergency department from another hospital with abdominal pain and vomiting in the past 2 weeks. The patient presented with clinical signs of acute abdomen. Physical examination showed diffuse abdominal tenderness. Abnormal laboratory findings comprehended Leucocyte count of 12.01 (3.5–10.0 × 109 g/L), Thrombocyte count of 456 (150.0–300.0 × 109 g/L), Neutrophil count of 9.7 (1.2–8.0 × 109 g/L), serum direct bilirubin value of 11.10 (0.0–8.6 mmol/L), and C-reactive protein value of 258 (0.0–5.0 mg/L). An abdominal computerized tomography (CT) scan revealed a large collection of fluid in the right hemiabdomen (Figs 1 and 2) and free gallstones in the abdominal cavity (Fig. 3).
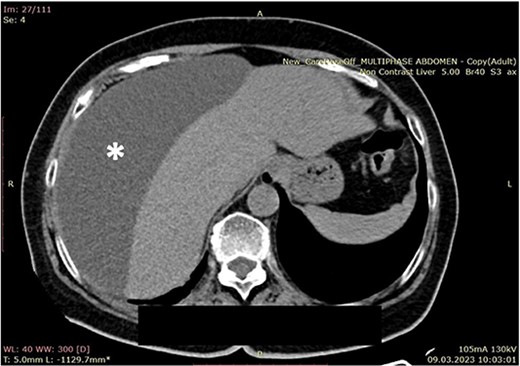
Computerized abdominal tomography (axial scan) showing a large biloma in the right subphrenic region (asterisk).

Computerized abdominal tomography (coronal scan) showing a large biloma (asterisk).
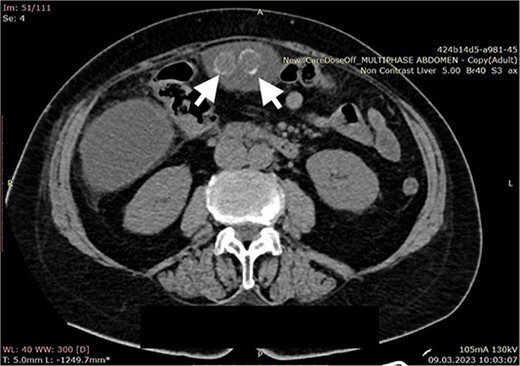
Computerized abdominal tomography (axial scan) showing two free gallstones in the intraabdominal cavity (arrows).
Indication for surgery was established. A median laparotomy was performed. The intraoperative finding correlated with biloma presence. Three liters of bile were evacuated from the abdomen, two free gallstones were found and removed (Fig. 4). A retrograde cholecystectomy followed. Two perforation sites at the fundus of the gallbladder were noted.
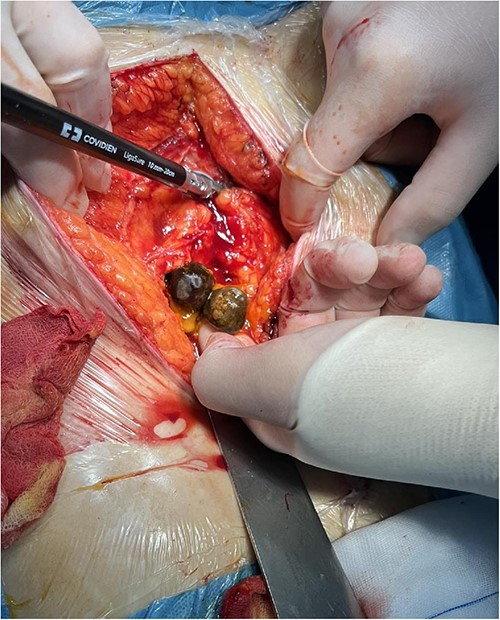
Intraoperative finding (free gallstones in the abdominal cavity).
The patient was given Metronidazole 3 × 500 intraoperatively and continued in the next 5 days. Hospital recovery was uneventful with 7 days duration of stay. After discharge, follow-up continued for 6 months; in the first month as an outpatient check-up and in the later period via telephone contact call. During this period, the patient did not exhibit any adverse event or laboratory irregularity and the only complaint was related to mild pain at the laparotomy site.
Discussion
In 1979, Gould et al. introduced the term “Biloma” when they encountered the phenomenon of extrahepatic collection of bile for the first time due to blunt abdominal trauma [3]. In 1983, Kuligowska et al. redefined it as “intrahepatic or extrahepatic collection outside the biliary tree with a fine demarcated capsule” [4]. In most cases, bilomas occur as a complication due to iatrogenic trauma following biliary surgery or intervention such as laparoscopic cholecystectomy, endoscopic retrograde cholangiopancreatography (ERCP), percutaneous catheter drainage, and blunt abdominal trauma. Pathophysiologically bilomas occur due to discontinuity of the biliary tree. However, the encapsulation is thought to be formed from one of the following mechanisms depending on the rate of the leakage. Slow bile leak causes inflammation to the surrounding tissue resulting in stimulation of the fibrosis formation as a protective mechanism. Rapid bile leaks lead to peritonitis primarily resulting in adhesions aiding encapsulation [5].
The site of perforation itself may influence the clinical presentation. Niemeier’s classification of gallbladder perforation was modified by Anderson and Nazem. They describe four types of perforation whereas type 2 results in biloma formation [6].
Spontaneous biloma due to gallbladder perforation (Type 2) is rarely reported. Literature review with the use of keywords “biloma” and “gallbladder perforation” resulted in the following cases shown in Table 1. Reported cases of intrabilliary (intrahepatic) perforation (Type 4) were excluded from the research since intrahepatic biloma formation did not occur in this case.
Literature review of reported cases with biloma presence as initial presentation in gallbladder perforation.
| Reference number . | Author . | Year . | Diagnostic tools . | Treatment . |
|---|---|---|---|---|
| [7] | Kalfadis et al. | 2011 | US, CT | Drainage under US |
| [8] | Tsai et al. | 2010 | US, CT | ERCP with endoscopic nasobiliary drainage |
| [9] | Ahn et al. | 2005 | CT, MRCP | Drainage under US |
| [10] | Krishnanand et al. | 2020 | US, CT | Laparoscopic cholecystectomy |
| [11] | O’Donnell | 2023 | CT | Not reported |
| [12] | Ji et al. | 2017 | CT, MR | Laparotomy, cholecystectomy |
| [13] | Ahmedou et al. | 2018 | US, CT | Percutaneous drainage + delayed cholecystectomy |
| This report | Limani et al. | 2023 | CT | Laparotomy, cholecystectomy |
| Reference number . | Author . | Year . | Diagnostic tools . | Treatment . |
|---|---|---|---|---|
| [7] | Kalfadis et al. | 2011 | US, CT | Drainage under US |
| [8] | Tsai et al. | 2010 | US, CT | ERCP with endoscopic nasobiliary drainage |
| [9] | Ahn et al. | 2005 | CT, MRCP | Drainage under US |
| [10] | Krishnanand et al. | 2020 | US, CT | Laparoscopic cholecystectomy |
| [11] | O’Donnell | 2023 | CT | Not reported |
| [12] | Ji et al. | 2017 | CT, MR | Laparotomy, cholecystectomy |
| [13] | Ahmedou et al. | 2018 | US, CT | Percutaneous drainage + delayed cholecystectomy |
| This report | Limani et al. | 2023 | CT | Laparotomy, cholecystectomy |
Literature review of reported cases with biloma presence as initial presentation in gallbladder perforation.
| Reference number . | Author . | Year . | Diagnostic tools . | Treatment . |
|---|---|---|---|---|
| [7] | Kalfadis et al. | 2011 | US, CT | Drainage under US |
| [8] | Tsai et al. | 2010 | US, CT | ERCP with endoscopic nasobiliary drainage |
| [9] | Ahn et al. | 2005 | CT, MRCP | Drainage under US |
| [10] | Krishnanand et al. | 2020 | US, CT | Laparoscopic cholecystectomy |
| [11] | O’Donnell | 2023 | CT | Not reported |
| [12] | Ji et al. | 2017 | CT, MR | Laparotomy, cholecystectomy |
| [13] | Ahmedou et al. | 2018 | US, CT | Percutaneous drainage + delayed cholecystectomy |
| This report | Limani et al. | 2023 | CT | Laparotomy, cholecystectomy |
| Reference number . | Author . | Year . | Diagnostic tools . | Treatment . |
|---|---|---|---|---|
| [7] | Kalfadis et al. | 2011 | US, CT | Drainage under US |
| [8] | Tsai et al. | 2010 | US, CT | ERCP with endoscopic nasobiliary drainage |
| [9] | Ahn et al. | 2005 | CT, MRCP | Drainage under US |
| [10] | Krishnanand et al. | 2020 | US, CT | Laparoscopic cholecystectomy |
| [11] | O’Donnell | 2023 | CT | Not reported |
| [12] | Ji et al. | 2017 | CT, MR | Laparotomy, cholecystectomy |
| [13] | Ahmedou et al. | 2018 | US, CT | Percutaneous drainage + delayed cholecystectomy |
| This report | Limani et al. | 2023 | CT | Laparotomy, cholecystectomy |
Clinical manifestation varies from asymptomatic to abdominal fullness, dull right upper quadrant, pain, nausea, vomiting, and sepsis. The diagnostic process typically starts with non-invasive methods, beginning with an abdominal ultrasound (US) examination that can reveal the presence of cysts, anechoic collections, or septated loculi, which may suggest an infection. To confirm the diagnosis, it is usually necessary to perform aspiration of the observed collections. While CT scans are an option, they have limitations in terms of specificity and may not effectively rule out other potential conditions like hematomas, seromas, or pseudocysts. The preferred diagnostic approach remains hepatobiliary cholescintigraphy using a Technetium-99m (Tc-99m) iminodiacetic acid chelate complex as a tracer. This test can detect both active leaks and sealed leaks, helping to guide appropriate treatment. However, it may have limitations when it comes to pinpointing the exact site of the leak due to a limited display of anatomical details. These limitations can be overcome by combining the cholescintigraphy with hybrid single-photon emission computed tomography (SPECT/CT) or magnetic resonance cholangiopancreatography (MRCP), both of which offer a more detailed view of the origin of the leak and can accurately identify connections between the biloma and the biliary system, with an accuracy rate ranging from 79 to 85%. In more invasive cases, procedures like ERCP can also be employed to both identify and treat bilomas. It is crucial to distinguish bilomas from other conditions such as pseudocysts, seromas, abscesses, or hematomas [12, 14, 15].
The management of bilomas depends on clinical, laboratory, and radiological findings. Options include percutaneous or endoscopic drainage, surgical drainage, or close monitoring, determined by factors like bile leak status, biloma size and location, infection, and patient condition. Small, asymptomatic collections may resolve spontaneously. However, Lee et al. demonstrated that bilomas larger than 4 cm rarely reabsorbed on their own and are not predictable [16]. Radiologically guided percutaneous drainage is often effective, with surgical intervention rarely needed. Ongoing bile leaks may require surgery or endoscopic stents. Surgical management is reserved for cases where percutaneous drainage fails or for complex, ongoing bile leaks, typically in specialized centers. Though limited evidence exists, percutaneous drainage generally offers a good prognosis for biloma patients [17, 18].
In this case, the timely diagnosis of a large biloma by the use of a CT scan resulted in satisfactory surgical treatment and outcome.
Conflict of interest statement
The authors declare no conflict of interest.
Funding
None declared.



