-
PDF
- Split View
-
Views
-
Cite
Cite
Yoshiaki Tomizuka, Soya Nagao, Koji Tanimoto, Kana Okugawa, Hiroko Shiraishi, Genki Iwama, Tomonori Kinoshita, Makoto Suruga, Hyunho Lee, Kazuyoshi Nakanishi, Bony mallet toe of the hallux treated with screws: a case report, Journal of Surgical Case Reports, Volume 2023, Issue 10, October 2023, rjad596, https://doi.org/10.1093/jscr/rjad596
Close - Share Icon Share
Abstract
Traumatic avulsion fracture of the distal phalanx of the hallux, known as the bony mallet toe of the hallux, is rare, and there is no consensus regarding its treatment. Few reports of treatment methods exist, such as nonsurgical treatment using a splint, Kirschner wires, and suture anchors, but there are no reports of screw fixation. We describe the case of a 54-year-old man with a bony mallet toe of the hallux treated with screws and augmented with strong sutures. The interphalangeal joint of the hallux was fixed with a Kirschner wire for 4 weeks after surgery, and weight bearing was allowed on the hallux 5 weeks postoperatively. A total of 20 months after the surgery, the patient had no symptoms or complications. Because of screw fixation and augmentation with strong sutures, fixation strength increased. We showed the feasibility of this new technique for treating an uncommon bony mallet toe of the hallux.
Introduction
Bony mallet toe of the hallux is uncommon, and few cases have been reported [1–7]. The treatment of mallet toe of the hallux remains controversial. Conservative treatment with rigid-soled sandals and a dorsal thermoplastic extension splint has achieved satisfactory results; however, it is difficult to immobilize the injured toe, and stabilization is necessary for 8–10 weeks [1, 2]. Several surgical treatments have been developed for this condition. Because the mechanism of injury is similar to that of a mallet finger, three reports have described closed reduction and percutaneous pinning techniques [3–5]. Two reports mentioned open reduction and fixation with Kirschner wire or suture anchors [6, 7]. This article reports an open reduction and screw fixation technique using sutures.
Case report
A 54-year-old man injured his right great toe while walking and wearing sandals. He complained of tenderness, swelling, and pain during motion. He could bear weight but could not actively extend the interphalangeal (IP) joint of the hallux. He was referred to our outpatient clinic 3 days after the injury. Physical examination revealed swelling, tenderness, and motion pain, and the patient could not extend the IP joint of the hallux. Plain lateral radiography and computed tomography revealed a displaced avulsion fracture of the dorsal base of the distal phalanx (Fig. 1). Surgery was performed under general anesthesia after informed consent was obtained on posttraumatic day 11. A Y-shaped incision was made at the center of the dorsal IP joint, and the displaced bony fragment was attached to the extensor hallucis longus (EHL). The IP joint was temporarily fixed with a 1.6 mm Kirschner wire, and the fragment was repositioned and fixed with two 1.5 mm cortical screws (APTUS® Hand, Medartis, Basel, Switzerland). A 4-0 FiberWire® (Arthrex, Naples, FL, USA) was fastened as an augmentation proximally to the EHL tendon and distally to the periosteum of the distal phalanx in a figure eight (Fig. 2). Postoperatively, the ankle was externally fixed in dorsiflexion from the leg to the toe, and heel loading was permitted. A total of 4 weeks after surgery, the Kirschner wire was removed to allow active motion of the IP joint of the hallux, and weight bearing was allowed on the hallux 5 weeks postoperatively. Plain radiographs taken 3 months after surgery confirmed bone healing (Fig. 3). A total of 20 months postoperatively, the patient acquired normal function, and the range of motion of the affected IP joint ranged from −3° to 30°, with no difference from the unaffected side (Fig. 4). Skin necrosis or nail deformities were not observed.

Plain radiographs (A) anterior–posterior view and (B) lateral view show an avulsion fracture of the dorsal base of the distal phalanx. Plain computed tomography (C) sagittal slice and (D) axial slice reveals an avulsion fracture of the dorsal base of the distal phalanx similar to the plain radiograph. Additionally, the fracture length line of the fragment was 5 mm.
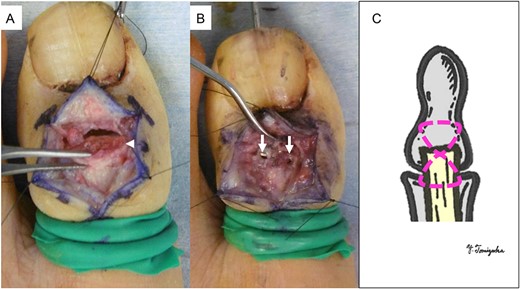
Operative findings (A) showed a bone fragment attached to the EHL (arrowhead) and (B) fixed with two screws (arrows). (C) Suture augmentation technique with FiberWire® (dotted line) proximally sutured to the EHL and distally sutured to the periosteum.

Postoperative plain radiographs (A) anterior–posterior view and (B) lateral view show the fragment fixed with two screws and temporarily fixed IP joint with Kirschner wire. Plain radiograph 3 months after surgery (C) anterior–posterior view and (D) lateral view indicates the bone union.
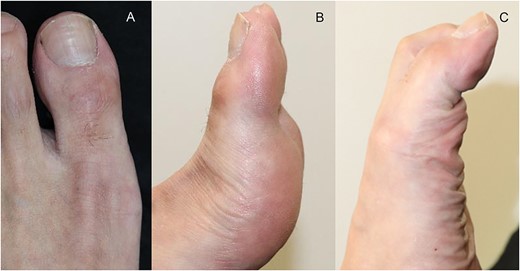
Physical findings 20 months after surgery (A) show EHL relief. Active motion shows IP joint range from (B) –3 to (C) 30°.
Discussion
Bony mallet toe of the hallux is uncommon, and only a few reports are available [1–7]. Because of its rarity, a standard treatment policy has not yet been established; however, each author has described satisfactory results using their procedure. In the two reports by Rapoff and Hennessy, nonoperative treatment of the mallet toe of the hallux used rigid sole sandals and a dorsal thermoplastic extension splint [1, 2]. Bone union was achieved, and satisfactory results were obtained; however, the IP joint was fixed for 8 and 10 weeks, respectively. Since then, several authors have reported satisfactory surgical treatment results. Nakamura et al. treated a patient with closed reduction and temporary IP joint fixation using Kirschner wire for 5 weeks [3]. Wada and Yui performed an extension block and temporary IP joint fixation with Kirschner wire for 4 weeks, similar to the Ishiguro method for bony mallet fingers [4]. Kawashima et al. described a percutaneous pinning technique [5]. Initially, an extension block wire was inserted into the proximal phalanx, and another Kirschner wire was placed through the dorsal fragment to the distal phalanx. Finally, the IP joint was temporarily fixed with a Kirschner wire for 6 weeks. Their procedure is frequently performed on the bony mallet finger, and they mentioned that this technique allows anatomical reduction and reduces the possibility of skin problems that may occur with the open surgical technique. Martin et al. considered closed reduction and fixation with Kirschner wires insufficient; thus, they performed open reduction, fixed the fragment with Kirschner wires, and immobilized the IP joint with a splint for 5 weeks [6]. Hong and Tan treated two cases with open reduction and a suture anchor without IP joint immobilization [7]. This technique is recommended because it causes less damage to the cartilage surface and allows early joint mobilization. In our patient, screw fixation was performed to achieve compression force. To our knowledge, the minimum screw diameter of the existing footplate system is 2.0 mm. Typically, to fix a bone fragment, the fracture line length of the fragment must be more than three times the screw diameter. In our case, it was 5 mm; therefore, we recognized that a 2.0 mm screw was unsuitable. Thus, the 1.5 mm screws used for hand surgery were useful, and to prevent rotation of the fragment, we placed two screws. If the fracture line length of the fragment was sufficient, two screws were placed. However, the 1.5 mm screw might have a weak fixation; therefore, we added augmentation with strong sutures. Wild et al. reported that suture augmentation improved the median load-to-failure force by 48% compared with the control group in olecranon fractures that used plate fixation [8]. Martin et al. performed open reduction, fixed the fragment with a Kirschner wire, and immobilized the IP joint for 5 weeks [6]. We performed fixation using two screws, augmented the fragment with a strong suture, and temporarily fixed the IP joint for 4 weeks. This might be unnecessary, or it could shorten the duration of the IP joint fixation because of the stronger fixation in our case. This issue warrants further investigation.
In conclusion, we described a new fixation method for the bony mallet toe of the hallux. When performing fixation with screws, we expected a compression force on the bone fragment. Furthermore, augmentation with FiberWire® increased fixation strength. Our technique can help foot and ankle surgeons who treat uncommon bony mallet toe of the hallux.
Conflict of interest statement
None declared.
Funding
None declared.
Data availability
Not applicable.



