-
PDF
- Split View
-
Views
-
Cite
Cite
Sally Tan, Yesha Maniar, Tulio B S Pacheco, Georgios Spentzouris, Anuj Malhotra, Venkata Kella, Unique multidisciplinary approach in a patient with small bowel obstruction and chronic mesenteric ischemia, Journal of Surgical Case Reports, Volume 2023, Issue 10, October 2023, rjad577, https://doi.org/10.1093/jscr/rjad577
Close - Share Icon Share
Abstract
Management of small bowel obstruction (SBO) in patients with symptomatic chronic mesenteric ischemia is a phenomenon that has not been previously described in the literature. This is an index case report describing the utilization of a multidisciplinary approach in a patient that suffered from SBO from cecal perforation with history of chronic mesenteric ischemia attributed to superior mesenteric artery (SMA) and celiac trunk stenosis. The patient was a 70-year-old female with recent diagnosis of ischemic colitis and chronic mesenteric ischemia, found to have high-grade SBO with transition point in the right lower quadrant. Computerized tomography angiogram showed occluded SMA, and severe celiac artery stenosis. Interventional radiology revascularized the celiac trunk with stent placement prior to right hemicolectomy for management of her high-grade SBO. Prospective research should ascertain whether revascularization indeed leads to improved post-operative outcomes.
Introduction
Chronic mesenteric ischemia (CMI) most commonly arises from progressive atherosclerosis leading to stenosis of the celiac artery, superior mesenteric artery (SMA), or inferior mesenteric artery (IMA) [1]. CMI usually remains asymptomatic unless arterial flow is decreased by 60–75% due to collateral circulation between the vasculature of the small intestines [2]. Once symptomatic, patients frequently report post-prandial abdominal pain, weight loss, and fear of consuming food due to pain.
CMI is most common in female adults 50–70 years old with atherosclerotic disease [3, 4]. Management strategies for CMI include both medical and surgical interventions, with an emphasis on restoring vascular supply [2]. Asymptomatic patients are treated conservatively with smoking cessation and antiplatelet therapy [4]. Symptomatic CMI is an indication for revascularization either via open surgery or endovascular intervention.
We present a case of a patient who suffered from CMI, and small bowel obstruction (SBO) secondary to cecal perforation. A unique multidisciplinary approach between interventional radiology and general surgery was utilized to improve vascular flow for her surgical approach.
Case report
A 70-year-old female with a past medical history of recent ischemic colitis, hypertension, diabetes, transient ischemic attack, and chronic smoking (eight cigarettes per day) presented to the emergency department with worsening right lower quadrant pain, nausea, and vomiting. The patient reported that her symptoms had started 1 year ago, and she had experienced significant weight loss of 50 pounds during this time. She denied any symptoms of diarrhea, or hematochezia during the past year.
One month prior to presentation, she was hospitalized at an outside institution and managed conservatively for ischemic colitis with pneumatosis intestinalis. She was discharged on oral antibiotics. Two weeks later, she underwent mesenteric angiogram, which demonstrated occlusion of the SMA and 80% stenosis of the celiac artery. There were multiple unsuccessful attempts to cannulate the SMA. After failed revascularization, she was being evaluated for other surgical options.
In the emergency department on presentation to our hospital, her vital signs were unremarkable and laboratory results were notable for a white blood cell count of 13 600 with left shift to 86% neutrophils. She underwent a computed tomography (CT) angiogram, which revealed an occluded SMA, severe celiac artery stenosis (nearly 90%), and a patent IMA (Fig. 1). A high-grade SBO was noted, possibly secondary to stricture, with transition point in the right lower quadrant (Fig. 2).
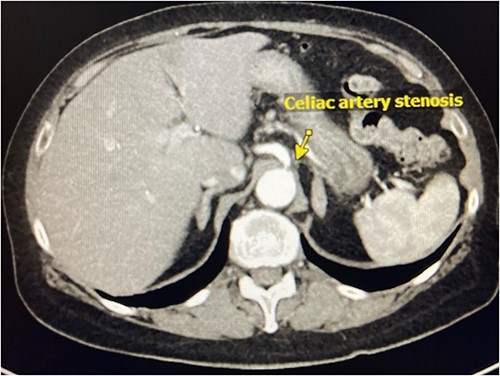
CT Angiography demonstrating celiac artery stenosis close to its origin.
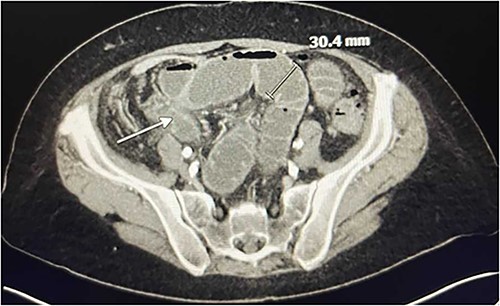
CT Angiography showing SBO with transition point in the right lower quadrant. A loop of thickened ileum measures 30.4 mm. The white arrow points to a stricture.
Initially, the patient underwent conservative management for the SBO. A nasogastric tube was placed, she received fluid resuscitation and antibiotic therapy. Given the findings of a possible stricture on her initial CT angiogram, she underwent CT enterography. Imaging demonstrated resolved obstruction, stricture and wall thickening in the terminal ileum and cecum, and severe aortoiliac atherosclerotic disease.
The patient’s symptoms were not resolving with conservative therapy and an operative intervention was deemed necessary to alleviate her symptoms, ultimately addressing the presence of the stricture. However, due to her atherosclerotic disease in the celiac artery and SMA, there was the possibility of ischemia if an ileocecal resection were to be performed.
Prior to operative intervention, the general surgery team consulted interventional radiology (IR) for management of her celiac artery and SMA stenosis and revascularization. Since a previous attempt to recanalize the SMA had failed, IR revascularized the celiac artery and a 5 mm by 18 mm balloon expandable bare metal stent was successfully placed. After stent placement, digital subtraction angiography demonstrated brisk flow through the celiac trunk (Fig. 3).
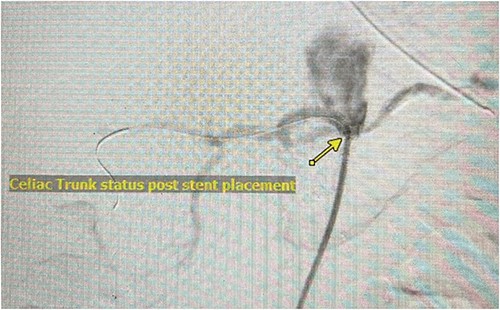
Angiography demonstrating flow through celiac trunk status post stent placement.
After the IR intervention, the patient underwent a robotic right hemicolectomy with enterolysis. Intraoperative findings revealed a cecal perforation, abscess and dense inflammatory tissue around the cecum, appendix, and terminal ileal mesentery (Fig. 4). Multiple loops of the small bowel were tethered to the abscess, which was most likely the cause of her SBO. There was no stricture noted. After the anastomosis had been performed, fluorescent angiography demonstrated adequate flow to the anastomosis.

Gross specimen showing thickened terminal ileum with cecal perforation.
The patient’s post-operative course was uncomplicated. She was discharged home on the second post-operative day once she was able to tolerate a diet and her bowel function returned.
Her pathology results showed mucosal ulceration and focal transmural necrosis with perforation in the cecum, with viable resection margins. The appendix and terminal ileum were uninvolved, with no significant histopathological changes, and five pericolic lymph nodes were found to have no significant pathological changes.
A month after the celiac stent placement, the patient had a follow-up visit with the interventional radiologist and vascular surgeon. An arterial ultrasound demonstrated flow in the celiac artery, SMA, and IMA. The patient continues to take aspirin and Plavix as part of her treatment.
Discussion
This case describes the management of a SBO requiring operative intervention in a patient with CMI. As demonstrated by this case, symptomatic CMI can result in a poor quality of life. They often present with weight loss, post-prandial abdominal pain, and food fear. The Society of Vascular Surgery strongly recommends endovascular revascularization to abate these symptoms. The primary target for revascularization is the SMA, with the celiac axis and interior mesenteric artery being secondary targets [2]. Open surgery is reserved for patients that fail endovascular management or present with lesions not amenable to endovascular intervention. We were able to pursue endovascular management for our patient, achieving revascularization of the celiac axis after a prior attempt at recanalization of the SMA had failed.
Generally, collateral circulation between the celiac artery and SMA allows for adequate blood supply even if there is significant atherosclerosis in one of these arteries [5]. With celiac artery stenosis, the collateral vessels most commonly are the pancreaticoduodenal arteries and the dorsal pancreatic artery [6]. However, in our case the patient had both SMA occlusion and celiac artery stenosis. Lack of collateral pathways led to her chronic symptoms and could possibly cause ischemia after resection and anastomosis.
Revascularization of mesenteric blood flow immediately prior to small bowel resection in the setting of SBO is a technique that has not been described previously in the literature. This novel approach to surgical treatment for cecal perforation in a patient with chronic mesenteric ischemia shows the importance of a multidisciplinary approach.
Conclusion
SBO in the setting of chronic mesenteric ischemia is a rare occurrence and there is no clear clinical guideline on how to treat these cases. Further studies on the incidence of such cases are warranted as celiac axis stenosis is seen in up to 25% of patients [7]. It will be important to ascertain whether revascularization indeed leads to improved post-operative outcomes.
Conflict of interest statement
The authors declare that they have no conflict of interest.
Funding
None declared.
Data availability
There is no data available. This is a case report.



