-
PDF
- Split View
-
Views
-
Cite
Cite
Akira Toga, Kentaro Fukuda, Masahiro Ozaki, Takeshi Fujii, Yoshiro Yonezawa, Reinstrumentation for progressive hyper-kyphotic deformity after implant removal despite obtaining physiological alignment by posterior corrective surgery for adolescent idiopathic scoliosis with flat back: a case report, Journal of Surgical Case Reports, Volume 2023, Issue 10, October 2023, rjad547, https://doi.org/10.1093/jscr/rjad547
Close - Share Icon Share
Abstract
This case report describes a 13-year-old female patient with adolescent idiopathic scoliosis (AIS) and flat back who experienced progressive kyphotic deformity after implant removal despite obtaining physiological alignment postoperatively. The patient underwent multiple surgeries, and a late-developing infection complicated her treatment course. Despite hard bracing to prevent kyphotic change, the kyphosis progressed to 74° within a year after implant removal, leading to a decrease in patient height and back pain. Revision surgery was eventually necessary. Possible factors for the kyphotic progression include injury to paraspinal back muscles due to multiple surgeries or insufficient bony fusion from late-developing infection. This case highlights the importance of thorough evaluation and follow-up for optimal patient outcomes after implant removal in AIS patients, particularly those with flat back.
Introduction
Adolescent idiopathic scoliosis (AIS) is a spinal deformity characterized by lateral curvature and rotation of the spine, affecting a significant number of adolescents worldwide [1]. For patients with progressive deformities where conservative treatment proves ineffective, the primary treatment option is posterior spinal fusion with instrumentation, which has demonstrated generally favorable outcomes [2]. However, a subset of patients may experience complications, including loss of correction after implant removal [3–7]. This report highlights a rare case of progressive hyper-kyphotic deformity in an AIS patient with flat back following implant removal, delving into potential causes and clinical implications. Additionally, we examine management strategies and derive valuable insights from this case to inform future clinical practice.
Case report
A 13-year-old girl was diagnosed with AIS classified as Lenke type 1A- since her standing radiographs demonstrated the main thoracic (MT) curve of 62° from T6 to L2, the thoracic kyphosis (TK) angle of 7° (Figs 1A and 2A). Posterior corrective surgery was performed at the T5-L2 level to prevent the progression of deformity. The MT curve was corrected to 17°, indicating a correction rate of 72.6%. The TK improved to 27° and acquired physiological kyphosis. At the 1-year follow-up, both the coronal and sagittal alignments were maintained, and the patient restarted sports activities without any impairment (Figs 1B and 2B). However, the patient returned to our hospital complaining of wound swelling 1 month later. Laboratory data showed a mild inflammatory reaction, but magnetic resonance imaging showed subcutaneous fluid accumulation, and its culture revealed Methicillin-susceptible Staphylococcus aureus. Although the infection subsided with debridement surgery and antibiotics, it recurred 3 months later. Inevitably, implant removal surgery was performed after confirming bony fusion by computed tomography (CT) scan. Following this, there was almost no loss of the coronal alignment; however, the sagittal alignment progressively deteriorated (Figs 1B, C). Even though hard bracing was introduced to prevent the progression of kyphotic change, the TK progressed to 74° in a year (Fig. 2C). As a result, the height of the patient decreased by 2.5 cm. The patient complained of back pain in the supine position and the radiograph revealed rigid thoracic hyper-kyphosis that was not corrected by fulcrum bending (Fig. 2D). Therefore, revision surgery was performed 15 months after implant removal. Solid bony fusion was confirmed from T5 to L2. However, slight intraspinal mobility was observed at T7/8 and T10/11, even though the preoperative CT scan showed no clear evidence of pseudarthrosis (Fig. 3A). Pedicle screws were placed from T2 to L3 using an O-arm navigation system due to the significant changes in anatomical structure. Schwab Grade 2 osteotomies were performed again with the removal of fusion masses at multiple levels including at T7/8 and T10/11and the kyphosis was corrected using the cantilever technique (Fig. 3B). At the 14 month follow-up, there was no evidence of recurrence or residual infection, and the MT and TK were corrected and maintained at 5° and 23°, respectively (Figs 4A, B).
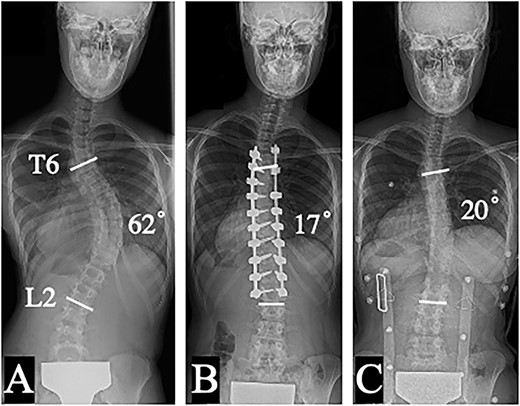
Posteroanterior plain radiographs in a standing position: preoperative (A), and 1 year after posterior corrective surgery from T5 to L2 (B); 1 year after implant removal (C).
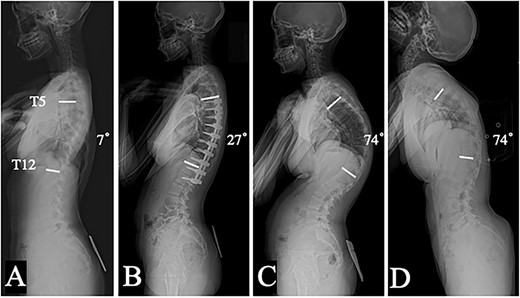
Lateral plain radiographs in a standing position: preoperative (A), and 1 year after posterior corrective surgery from T5 to L2 (B); 1 year (C) after implant removal; dorsal flexion in the supine position before revision surgery (D).
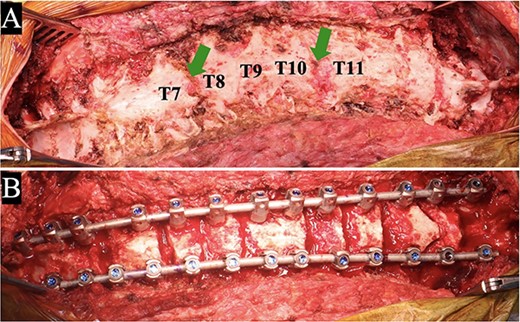
Intraoperative findings of revision surgery: solid bony fusion was confirmed except at T7/8 and T10/11 levels (arrows) (A); after correction with multilevel osteotomies (B).
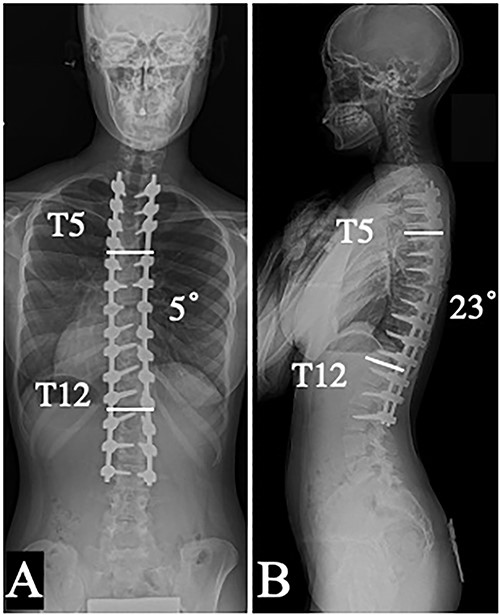
Coronal (A) and sagittal (B) plain radiographs in a standing position taken 14 months after the revision surgery.
Discussion
Several studies have described implant removal resulting in loss of coronal and/or sagittal correction [3–7]. Potter et al. [3] conducted a study on 21 AIS patients after implant removal, revealing a 10° correction loss in the coronal plane, while no significant changes were observed in the sagittal plane. In contrast, Tauchi et al. [4] indicated that implant removal affected the sagittal plane rather than the coronal plane since the MT curve increased by over 10° in 3.8% of cases, while the TK increased in 18.9% of cases. Rathjen et al. [5] also revealed the outcomes of implant removal in 43 patients with idiopathic scoliosis and reported that two patients (5%) experienced >10° of coronal plane progression in their MT, while 24 patients (56%) showed an increase of >10° in TK. Five patients (12%) with>20° (range, 22°–27°) of progression of TK after implant removal had greater TK before surgery. In our case, TK increased significantly from 27° to 74° within 1 year after implant removal. This case emphasizes the severity in progression of kyphotic deformity following implant removal, even though postoperative physiological alignment was achieved. Our case is also unique in that the patient had a flat back before surgery, as opposed to having greater TK.
Furthermore, there is concern that implant removal may require revision surgery due to severe curve progression. Kotani et al. [8] reported that MT curve increased from 29° to 57° within 15 months after implant removal following posterior spinal fusion, necessitating reinstrumentation. To the best of our knowledge, this is the first report of TK deterioration into symptomatic hyper-kyphosis, requiring reinstrumentation after implant removal despite achieving physiological alignment through corrective surgery for AIS with flat back.
The exact cause of this course remains unclear; however, possible factors include injury to paraspinal muscles from multiple surgeries or insufficient bony fusion due to late-developing infection. Repeated surgeries, as in this case, can lead to damage and atrophy of the paraspinal muscles, which can compromise their ability to provide adequate spinal stabilization and support [9]. This muscle dysfunction may contribute to the progression of the kyphotic deformity, especially in the absence of adequate spinal instrumentation following implant removal. As for the late-developing infection, it can interfere with the bone healing process and may cause osteolysis or septic loosening of the fusion mass, ultimately resulting in pseudarthrosis and instability [10, 11]. Alpert et al. [12] reported that patients who underwent implant removal for infection had more curve progression than those without infection. These factors, combined or individually, could have played a role in the observed kyphotic progression in this patient.
In conclusion, our case report presents a unique situation in which kyphotic deformity deteriorated after implant removal despite obtaining physiological alignment by posterior corrective surgery for AIS with flat back. This case serves as an important reminder of the potential complications that can arise after implant removal and emphasizes the need for thorough evaluation and follow-up to ensure optimal patient outcomes.
Author contributions
Conception and design: Kentaro Fukuda. Acquisition of data: Akira Toga, Kentaro Fukuda. Interpretation of data: Akira Toga, Yoshiro Yonezawa, Takeshi Fujii, Kentaro Fukuda. Study supervision: Masahiro Ozaki, Yoshiro Yonezawa, Takeshi Fujii, Kentaro Fukuda. Drafting the manuscript: Akira Toga, Masahiro Ozaki, Kentaro Fukuda. Critically revising the manuscript: Masahiro Ozaki, Yoshiro Yonezawa, Takeshi Fujii, Kentaro Fukuda. The final version of the manuscript was approved by all the authors.
Conflict of interest statement
The authors declare that there are no relevant conflicts of interest.
Funding
None declared.
Ethical approval
This study was approved by Saiseikai Yokohama-shi Tobu Hospital Ethics Committee (approval number, 202110096).
Informed consent
Informed consent was obtained by a participant in this study.
Data availability
The data supporting this study's findings can be provided by the corresponding author upon request.



