-
PDF
- Split View
-
Views
-
Cite
Cite
Mohammed Amir Rais, Yahia Naouri, Ahmed K Awad, A rare case of left parapharyngeal space large schwannoma of unknown origin, Journal of Surgical Case Reports, Volume 2023, Issue 1, January 2023, rjac578, https://doi.org/10.1093/jscr/rjac578
Close - Share Icon Share
Abstract
Schwannoma, also called neurilemmoma, is a rare neurogenic tumor exclusively benign that develops from a variety of glial nerve cells called Schwann cells. We present a 26-year-old female patient who was admitted with a history of dysphagia, headache and swelling going from the lower limit of the ear to the floor of the neck on the left side, which has been slowly progressing for 5 years. Upon local clinical examination, a well-defined mass was revealed, 6 × 5 cm in size, non-painful spontaneously, painful on direct palpation of the left neck. Computed tomography scan has shown a well-circumscribed large mass with heterogenous areas of enhancement in the left parapharyngeal space displacing the submandibular gland superiorly and the carotid sheath anterolaterally and compressing the oropharyngeal airway. Excision of the tumor was done by a combined route without post-operative complications noted. Histopathological examination revealed a benign schwannoma without the identification of the nerve of origin.
INTRODUCTION
Schwannoma, also called neurilemmoma, is a rare neurogenic tumor exclusively benign that develops from a variety of glial nerve cells called Schwann cells [1]. The function of these cells is to insulate the myelin sheath—the white tissue covering around axons to speed up the transmission of nerve impulses—from the axons of the peripheral nervous system and help in impulse propagation [2, 3]. Head and neck schwannoma can develop in several areas such as the cervical region, the jugular foramen and the hypoglossal canal with the parapharyngeal space being the most common location of this tumor by 31% [4]. Although parapharyngeal space schwannoma is usually of a salivary or neurogenic origin, schwannomas’ etiology is still unknown with slowly progressive growth [4]. Patients usually are diagnosed clinically with dysphagia and chronic nasal obstruction [5].
Schwannomas can be divided into central or peripheral lesions, so differential diagnosis must be established with other tumors clinically similar such as neuromas, neurofibromas, granular cell myoblastoma, fibromas [6]. Radiological examinations, especially computed tomography (CT) or magnetic resonance imaging (MRI), are extremely important in its primary diagnosis, providing valuable information, showing a homogeneous, very well delimited and solid lesion with shooting pain on direct palpation [7]. Generally, the treatment consists of a total surgical excision of the benign tumor, followed by a postoperative histopathological examination to establish the final diagnosis and confirm the absence of malignancy [8]. The parapharyngeal space schwannoma is usually of a salivary or neurogenic origin, and common among young population [9].
CASE PRESENTATION
A 26-year-old female patient was admitted with a history of dysphagia and swelling going from the lower limit of the ear to the floor of the neck on the left side, which has been slowly progressively increasing for 5 years. The patient has no illness or medical history; she reports that the swelling has been progressively increasing and starts causing dysphagia and pain on palpation. After first consultation with an ENT doctor, a CT scan was requested, upon which the doctor referred her to us in the maxillofacial surgery department. General and systemic examination was normal. Local clinical examination revealed a well-defined solitary mass of size 6 × 5 cm, non-painful spontaneously, painful on direct palpation of the left neck. Swelling was large below the angle of the mandible extra-orally on the left side. No cervical lymphadenopathy was found, and the overlying mucosa was normal in color and appearance.
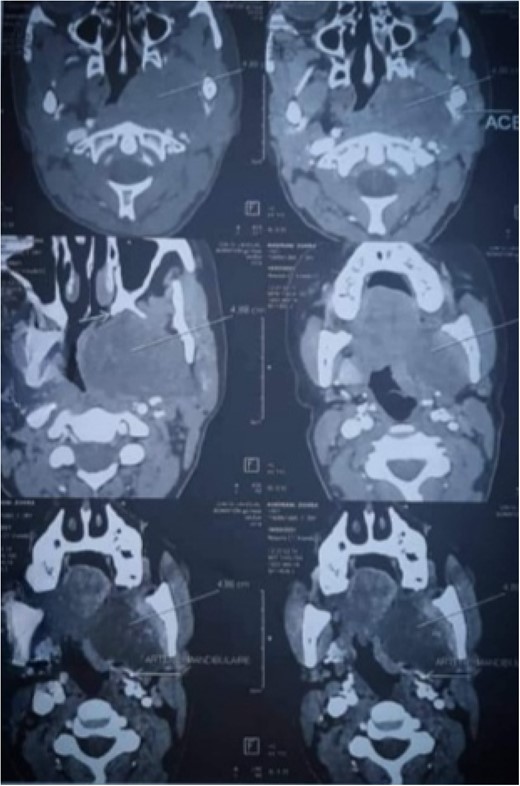
CT-scan has shown well-circumscribed, large-mass heterogenous areas of enhancement with size 6 × 44× 5 cm in the left parapharyngeal space displacing submandibular gland superiorly, carotid sheath anterolateral compressing the oropharyngeal airway (Fig. 1) Routine blood investigations were within the normal limit; hence, surgical removal under general anesthesia decision was done.
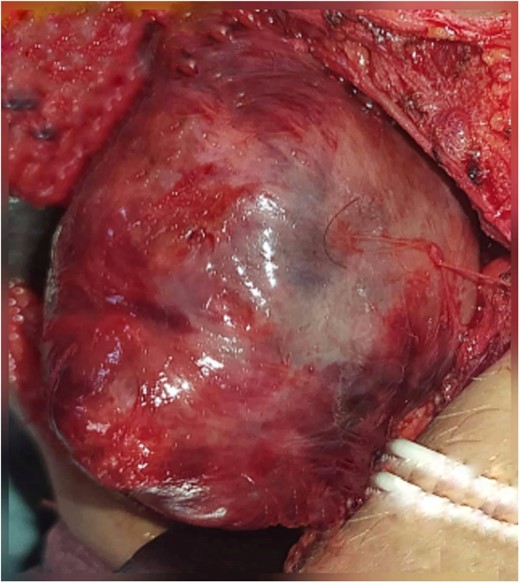
Excision of the tumor was principally done by a combined route. The first incision is a 10-cm external incision made below the arch of the left mandible from the mastoid tip to the neck middle; after flap elevation, the tumor was exposed but enucleation attempts were not successful due to its large volume, which forced us to make a second endo-buccal incision that was 5 cm in size and performed on the anterior tonsil pillar (Palatoglossal arch); this access was used to enucleate the rest of the tumor and thus its total detachment. The tumor was a well-circumscribed, homogeneous and lobulated firm red mass (Fig. 2). The wound was closed in layers with drain in situ.
No post-operative complication was noted. Patient was discharged on the second day and came back on the fourth day for drain removal. New CT-scan revealed a successful surgery intervention (Fig. 3). Post-operative antibiotic injection of cefotaxime and injection of metronidazole was given for 5 days, and analgesic treatment with paracetamol 1 g every 6 h in the presence of pain was recommended. Histopathological examination revealed a benign schwannoma. Suture removal of the both incisions performed on the 10th post-operative day (Fig. 4), with a strict oral hygiene recommended to the patient. Up to the last consultation, July 2022, no side effects or complications have been reported.


DISCUSSION
Schwannomas are benign and rare tumors of the peripheral nerves, derived from the nerve supporting Schwann cells [3]. Approximately 25–40% of schwannomas occur in the head and neck. With the oropharyngeal site being rare, the most common site is the parapharyngeal space of the neck [2]. The parapharyngeal space is shaped like an inverted pyramid, extending from the skull base superiorly to the greater cornu of the hyoid bone inferiorly [9]. The parapharyngeal space should be considered in two compartments: pre- and post-styloid compartments [9]. Histologically, schwannomas are distinct from the nerve itself and are well circumscribed and encapsulated with discrete patterns known as Antoni Type A and Type B being possibly observed [5]. Clinically, schwannomas produce few clinical symptoms and the main symptoms are usually due to the presence of a slow-growing mass, causing dysphagia, pain on palpation [1]. Schwannoma like other rare tumors can present with vague symptoms like headache and nausea [6] and rarely presenting ulceration; hence, its clinical diagnosis is difficult, and its definitive diagnosis is established by the histopathological study of the lesion [1].
Schwannoma can occur at any age with a predominance in early ages; it can also seen equally in both sexes [3]. CT scan and often an MRI are mandatory to determine its size and exact position in relation to the local nerves and vessels [4]. Prognosis is excellent as the treatment of schwannomas consists of surgical removal of the tumor by enucleation, with preservation of the neighboring structures. Furthermore, it is often possible to preserve the nerve of origin with rare recurrence if enucleation performed efficiently [10]. In this case, its slow progression was confirmed, often going unnoticed; for this patient, dysphagia and swelling were the main reasons for consultation, and the surgical removal was done completely, but with the need of a second endo-buccal incision justified by the important volume, the post-operative period was not associated with any neurological deficit or other complications. In our case, we do not know its exact origin.
CONCLUSION
Although parapharyngeal space schwannoma is the most common, it is not only rare but also difficult to diagnose from the vague nature of presentation. Most of the patients are asymptomatic and only experience dysphagia if swelling is large enough to have pressure manifestations. CT or MRI should be performed before the mainstay line of treatment, which is the radical removal of the tumor with its capsule.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The case report was performed following the declaration of Helsinki and according to the international guidelines and ethics.
CONSENT TO PUBLISH
Written consent was taken from the patient and uploaded as a supplementary file for review by editor in chief.
DATA AVAILABILITY
All data generated or analysed during this study are included in this published article and its supplementary information files.
HUMAN AND ANIMAL RIGHTS
Patient has consent to report his case, and no animals were used at our study, and our manuscript respected and conducting to ensure all human rights.



