-
PDF
- Split View
-
Views
-
Cite
Cite
Michael Basin, Alexandra Dimmer, Shogik Abramyan, Sanjit O Tewari, Amie Lucia, Percutaneous extraction of metallic foreign body from pyogenic liver abscess, Journal of Surgical Case Reports, Volume 2022, Issue 8, August 2022, rjac349, https://doi.org/10.1093/jscr/rjac349
Close - Share Icon Share
Abstract
We report a case of a 35-year-old male who developed a pyogenic liver abscess (PLA) secondary to a foreign body that migrated from the transverse colon into the liver. The mainstay of treatment of PLA requires removal of the foreign body, most frequently performed surgically. Few case reports exist of percutaneous removal. As our patient was hemodynamically stable at time of presentation, he underwent successful percutaneous transhepatic removal of the foreign body, avoiding any need for surgical operation.
INTRODUCTION
Pyogenic liver abscesses (PLA) are the most common type of intra-abdominal abscess, with an annual incidence around 2.3 cases per 100 000 [1]. The typical pathophysiology of PLA involves perforation and peritonitis, biliary infection, and surgical or penetrating abdominal wounds. Prior literature commonly describes hepatic abscesses following foreign body ingestion, most commonly with a fishbone [2]. Surgical drainage and foreign body removal remain the mainstay of treatment of hepatic abscesses, with treatment failure rates of 90.5% without foreign body removal [2].
This case describes an ingested paperclip that perforated the transverse colon and migrated into the liver, causing a PLA. The patient underwent successful percutaneous transhepatic foreign body removal.
CASE REPORT
The patient is a 35-year-old incarcerated male with a pertinent history of obesity (BMI 36), depression, psychosis and multiple previous foreign body self-insertions requiring removal by esophagogastroduodenoscopy (EGD) and bronchoscopy.
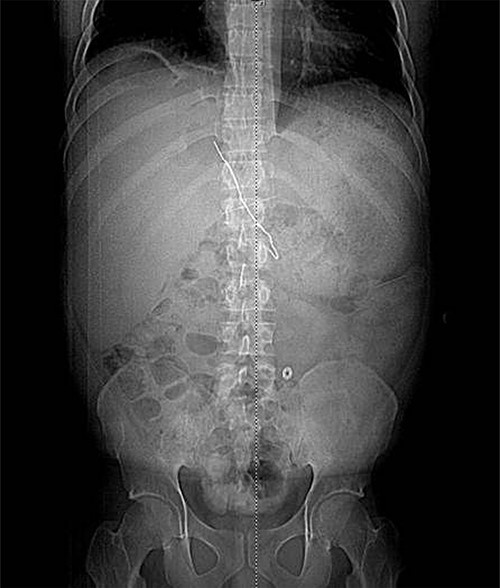
The patient presented after ingestion of an open paperclip and insertion of a sewing needle into his ventral hernia ~4 months prior. He presented with fever, tachycardia and abdominal pain, but a benign abdominal exam, noting only mild tenderness over his large, reducible ventral hernia. A computed tomography (CT) of the abdomen and pelvis showed a 10-cm metallic foreign body extending from the mid transverse colon to the left hepatic lobe with an intrahepatic abscess measuring 9.1 x 7.3 cm (Figs 1–3). In addition, there were two other metallic foreign bodies: one extraluminal in the left upper quadrant, which was stable from prior imaging, and a subcutaneous foreign body above the hernia contents. Blood cultures grew streptococcus intermedius and he was started on broad spectrum antibiotics (piperacillin–tazobactam). The case was discussed with Interventional Radiology (IR) and deemed reasonable for attempt at percutaneous abscess drainage and trans-hepatic foreign body retrieval.
The patient underwent left hepatic abscess drainage and fluoroscopic-guided foreign body retrieval of intrahepatic foreign body. Through an image guided intercostal approach, an 0.035 inch guidewire was coiled within the hepatic abscess and a vascular sheath was introduced. The hepatic end of the paper clip was able to be snared, but could not be completely removed due to lack of traction. The snare was able to guide the end of the paperclip into the sheath where a high pressure non-compliant balloon (Conquest) was the inserted over an 0.035 inch stiff Glidewire and inflated in the sheath adjacent to end of the paperclip to wedge the paperclip into the vascular sheath, and under fluoroscopic guidance, the inflated Conquest balloon, paperclip and vascular sheath were successfully removed as a unit (Figs 4 and 5). A drain was left in the hepatic collection. The two small extraluminal foreign bodies were left in place.
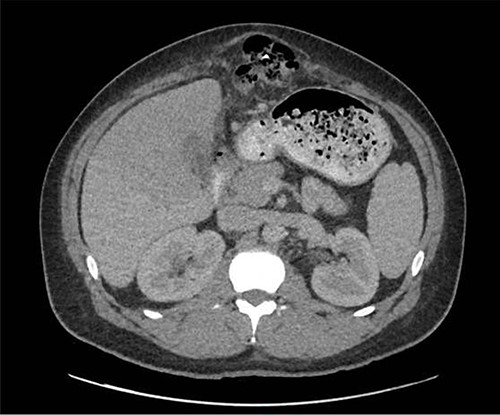

CT view of metallic foreign body within the liver abscess cavity.
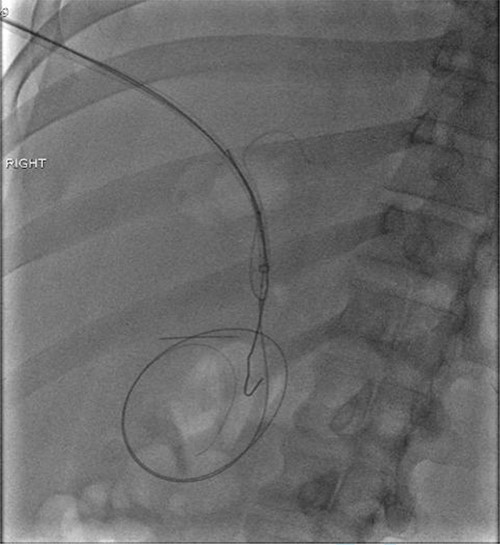
Fluoroscopic image obtained intraoperatively demonstrating removal of the metallic foreign body

Abscess cultures grew Escherichia coli and Streptococcus intermedius. His post-procedure course was complicated by a large, loculated right pleural effusion requiring thoracostomy tube placement and 3 days of fibrinolytic therapy. This tube was removed following resolution of his symptoms and effusion.
Interval CT imaging demonstrated reduced size of his hepatic collection; however, additional pre-rectal and right upper quadrant fluid collections were noted, requiring percutaneous IR drainage. All drains were removed on hospital Day 34 after imaging demonstrated resolution of the collections. He was subsequently discharged on oral antibiotics (amoxicillin–clavulanate).
DISCUSSION
Many case reports have described liver abscesses following foreign body ingestion, such as fish bones, toothpicks or various metallic foreign bodies. Diagnosis of liver abscess secondary to foreign bodies is clinically challenging, as patients frequently present with non-specific symptoms and most patients do not reveal a history of ingestion or insertion of foreign bodies. In addition, initial imaging is often negative (70%) and 53% of foreign bodies are not seen on imaging [2]. Our patient had a delayed presentation, which is common in patients with PLA, with symptoms ranging from 1 day to 1 year (mean 39 days) [2]. This is likely due to the gradual nature of perforation and close proximity of the omentum, which contains the perforation and limits a systemic response [3]. Furthermore, the small caliber of the foreign body may reduce bowel spillage and risk of peritonitis, delaying presentation.
The mainstay of treatment of PLA caused by a foreign body involves percutaneous or surgical abscess drainage, foreign body removal and broad-spectrum antibiotics [4]. Some studies describe serial percutaneous drainages of PLA without drain placement with a success rate of 96.5% after 3 drainages; however, a foreign body was not the inciting cause [5]. Surgical foreign body removal is frequently performed with laparotomy or laparoscopy, often due to an acute abdomen.
In select stable patients with favorable anatomy, percutaneous removal of foreign bodies may be attempted. To date, there have been two case reports of successful percutaneous transhepatic foreign body removal [6, 7]. Our team considered both surgical and percutaneous removal, however due to the patient’s history of multiple prior foreign body insertions, we had concern that surgical intervention could be complicated by further future foreign body insertion. The patient underwent successful percutaneous removal of the foreign bodies. He had a prolonged hospital course secondary to reactive pleural effusion and subsequent abdominal collections that were effectively managed with minimally invasive techniques.
CONCLUSION
PLA secondary to foreign body ingestion should be considered in patients with history of foreign body ingestion, solitary abscess without systemic cause, left lobe involvement or treatment failure. Percutaneous drainage and foreign body removal should be considered in select patients who are hemodynamically stable with a favorable anatomy to avoid a complex surgical operation. However, close monitoring is required to monitor for peritonitis necessitating an emergent exploratory laparotomy.



