-
PDF
- Split View
-
Views
-
Cite
Cite
Daniel Barbash, Aakash A Trivedi, James Y Yang, Richard B Nguyen, John C Huribal, Jamshed Zuberi, Osama Elsawy, Scott Wessner, Incidental discovery of goblet cell carcinoid, a rare appendiceal malignancy case report, Journal of Surgical Case Reports, Volume 2022, Issue 7, July 2022, rjac356, https://doi.org/10.1093/jscr/rjac356
Close - Share Icon Share
Abstract
Goblet cell carcinoid (GCC) tumor is a rare appendiceal carcinoma that has had several names throughout its history. Often found incidentally on pathology following an appendectomy, treatment includes a right hemicolectomy and possible adjuvant chemotherapy. Survival rate has been shown to be correlated with the histological features. Here, we report a 45-year-old African American male who presented with signs and symptoms consistent with acute appendicitis, but was ultimately diagnosed with GCC. After undergoing a right hemicolectomy, he continues to undergo long-term surveillance with his oncologist. Due to the rarity of this tumor, we describe the history of GCC and our recommendations for surgical and long-term management.
INTRODUCTION
Goblet cell carcinoid (GCC) is a rare malignancy of the appendix that displays features of both adenocarcinoma and carcinoid tumors, including goblet or signet cells along with Paneth cells, but not absorptive cells [1]. Since its identification in 1969 [2], it has been called various names such as adenocarcinoid, mucinous carcinoid, crypt cell carcinoma and mucin-producing neuroendocrine tumor [3]. Their biologic behavior and prognosis still remains unclear. We report a case of a 45-year-old male who presented with signs of acute appendicitis, but was diagnosed incidentally with GCC via pathologic inspection of his appendix following laparoscopic appendectomy. After the diagnosis of GCC, the patient underwent a laparoscopic right hemicolectomy with complete resection and negative nodal involvement.
CASE REPORT
A 45-year-old African American male with a past medical history of hypertension, end stage renal disease and congestive heart failure presented to the emergency department complaining of severe abdominal pain for three days. The pain started in the epigastric region, moved to lower quadrants and was associated with two loose bowel movements the day prior.
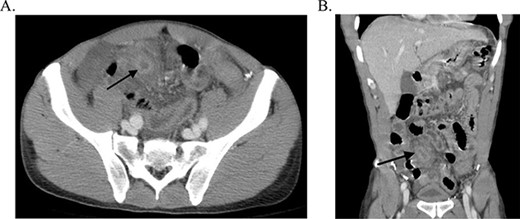
The patient was afebrile with stable vital signs. His abdomen was diffusely tender with greatest tenderness to palpation in the right lower quadrant as well as involuntary guarding, rebound tenderness and positive McBurney’s point. On admission, the patient had leukocytosis. CT abdomen/pelvis showed a thickened tubular structure in the right lower quadrant that was concerning for appendicitis (Fig. 1), with wall thickening of multiple small bowel and colonic loops possible secondary to peritonitis. The patient underwent an emergent laparoscopic appendectomy with lysis of adhesions.
During surgery, the appendix was perforated, necrotic with an edematous base, purulent fluid throughout the peritoneum and adhesions to the small bowel. Pathology displayed GCC with a positive proximal margin as well as neuronal and vascular invasion (Fig. 2). Subsequently, the patient underwent a diagnostic laparoscopy and laparoscopic right hemicolectomy with primary anastomosis to remove the GCC malignancy six days later. There were intraabdominal adhesions and possible mucocele at the appendiceal base (Fig. 3). The pathologic examination showed the right colon with the terminal ileum having no residual GCC and 12 benign lymph nodes. The terminal ileum was sent for further analysis that showed one out of three blocks with rare malignant signet ring cells (SGC). Upon discussion with medical oncology, the patient will require lifelong radiologic and endoscopic surveillance, but currently no adjuvant therapy is indicated. Patient tolerated the procedure well and was discharged home a week later.
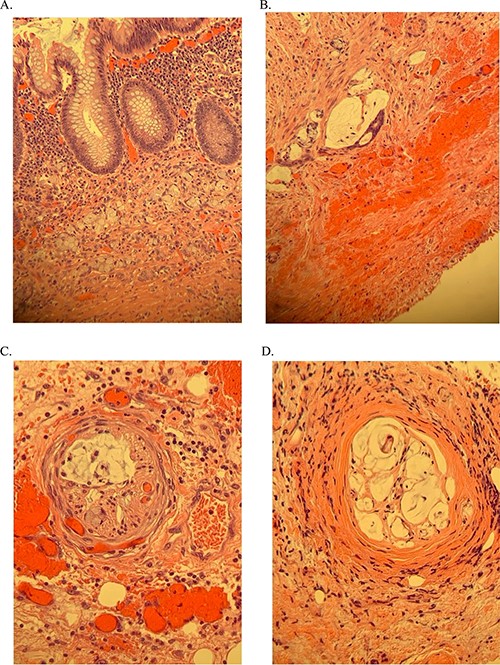
Histology of the appendix following initial laparoscopic appendectomy. (A and B) goblet cells with positive margins. (C) Neuronal invasion. (D) Vascular invasion.
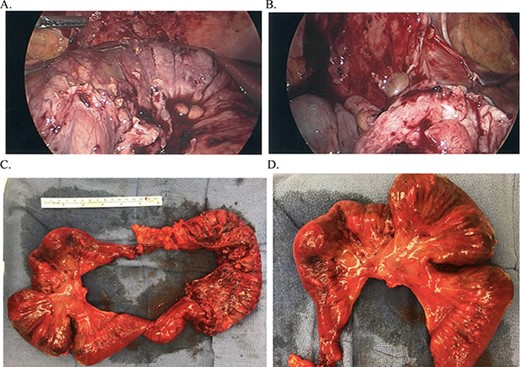
(A and B) Intraoperative findings during laparoscopic right hemicolectomy and (C and D) Right hemicolectomy specimen, mucocele near appendiceal base.
DISCUSSION
Goblet cell carcinoid (GCC) is a rare cancer that still has many questions surrounding its biological behavior, prognosis and nomenclature. Part of the problem is that this tumor has also been called adenocarcinoid, mucinous carcinoid and mucin-producing neuroendocrine tumor. The first description of a tumor in the appendix that displayed both the glandular and neuroendocrine features was made in 1969 by Gagne et al. [2]. In 1974, the term ‘Goblet Cell Carcinoid’ was coined by Subbuswamy et al. Many others have reported tumors of similar description and various names trying to encapsulate the essence of this neoplasm.
The average age of presentation of patients with GCC is in the fifth or sixth decade of life [1, 3–6]. The most common clinical presentation of GCC is acute appendicitis [3, 4], abdominal pain, appendiceal mass or asymptomatic with CT scan obtained for other unrelated reasons [3, 4, 6]. Treatment is typically an appendectomy and/or right hemicolectomy [3, 4, 6, 7]. If the extent of the disease warrants chemotherapy, 5-FU and leucovorin are often used [4]. The five-year survival has been reported to be between 60 and 84% [3, 4, 7], better when compared to appendiceal adenocarcinoma, and worse than a malignant carcinoid tumor [8].
Grossly, GCCs rarely have a discrete mass. Instead, a thickened, nodular appendix is usually seen [3, 6]. Lack of a discrete mass makes measurements difficult, but on average tumors are >2 cm [3, 6]. Histologically, GCCs typically display clusters of goblet cells and positive staining for various neuroendocrine markers, which is usually patchy in intensity [1, 3–5, 9]. Paneth cells are typically found in the deep submucosa [1]. Immunohistochemical staining shows focal areas of positivity with chromogranin, synaptophysin [3, 6, 9], CEA, CK20 and CDX-2 [1, 3, 9].
Recently, some authors have pushed for a reclassification of GCC, arguing the suffix ‘carcinoid’ suggests a more benign tumor and an incorrect interpretation as a neuroendocrine tumor, leading to staging and prognostic errors [10]. Several proposed dividing GCC into subdivisions, which would aid in treatment and better prognostic value. Tang et al. subclassified 66 cases of GCC based on histological features into typical GCC, SGC type and poorly differentiated adenocarcinoma type, finding a 5-year survival of 100, 38 and 0% respectively [6]. Taggart et al. divided 74 patients with GCC into three groups based on the percentage of adenocarcinoma: Group 1 with less than 25% adenocarcinoma features, group 2 with between 25 and 50% adenocarcinoma features, group 3 with more than 50% adenocarcinoma features and group 4 had only adenocarcinoma features. They found that higher percentage of adenocarcinoma correlates with higher stage at presentation and lower mean survival in months; 83.8, 60.6, 45.6 and 33.6. months, respectively [11]. Lee et al. divided 78 patients with GCC into two groups, high-grade and low-grade, based on cytologic atypia, peritumoral stromal desmoplasia and solid growth pattern, finding a 10-year survival for the low-grade and high-grade groups was 80.5 and 0%, respectively [12].
CONCLUSION
GCC typically presents with signs and symptoms of acute appendicitis or abdominal pain. Usually, the diagnosis is made incidentally on pathologic analysis of the appendix after appendectomy as it was in this case. Recommendations for treatment include appendectomy, hemicolectomy, and possible adjuvant therapy depending on the extent of the disease. Due to the high variability of biologic behavior displayed by these tumors, it is difficult to determine one’s prognosis. Subclassifications and alternate nomenclatures have been proposed by several groups, which have shown better prognostic value. Recent studies suggest that having a higher proportion of histologic features similar to adenocarcinoma than carcinoid indicate a poorer prognosis. Until a classification system is universally accepted and a consensus on a treatment algorithm can be made, it will be difficult to predict the course of the disease. Surgery, with or without chemotherapy, should be assessed based on the extent of the disease and lifelong surveillance may be warranted.



