-
PDF
- Split View
-
Views
-
Cite
Cite
Ibrahim Alonazi, Yam Alharthy, Ghadeer Alghamdi, Sleeve gastrectomy in a patient with situs inversus: a case report, Journal of Surgical Case Reports, Volume 2022, Issue 7, July 2022, rjac325, https://doi.org/10.1093/jscr/rjac325
Close - Share Icon Share
Abstract
Situs inversus (SI) is a very rare congenital disease affecting one in 10 000 people. It is characterized by a mirror image transposition of both abdominal and thoracic organs. Diagnosis of SI is usually made incidentally while investigating for unrelated medical problem. It can be associated with cardiac and respiratory anomalies that may cause perioperative morbidity if not diagnosed before surgery. There are limited case reports in literature of SI patients that underwent bariatric procedures. We report a case of a 32-year-old female with SI partialis and levocardia who successfully underwent laparoscopic sleeve gastrectomy. We concluded that sleeve gastrectomy is safe in patients with SI if diagnosed preoperatively and if all the necessary precautions are taken into consideration before and during the surgery.
INTRODUCTION
Situs solitus is the normal distribution of organs inside the human body. Any abnormality in the left–right asymmetry will produce a spectrum of laterality disturbances. There are >100 genes related to laterality defects. One of the laterality defects is the situs inversus (SI) where there is a mirror image transposition of organs that can be complete or partial. It is a very rare congenital disease first reported by Fabricius [1] in 1600.
Obesity nowadays is a major health problem and currently becomes the fifth most leading cause of death worldwide [2]. It is estimated that 20% of the world population will be obese by 2030, while 38% will be overweight. Obesity is a modifiable and preventable risk factor for many diseases including diabetes mellitus, hypertension, hyperlipidemia, sleep apnea, asthma, osteoarthritis and infertility [3].
We present a case of morbid obesity and SI with levocardia which successfully underwent laparoscopic sleeve gastrectomy.
CASE PRESENTATION
We report a case of a 32-year-old female with morbid obesity, weighing 144 kg, height of 162 cm and BMI of 55 kg/m2.
The patient was diagnosed with SI while being operated for sleeve gastrectomy in other country, 7 years ago. The operation was aborted due to abnormal findings of reverse intra-abdominal organs.
The patient presented to our centre where she was evaluated by a multidisciplinary team including cardiology, psychology, anaesthesia, dietician and bariatric surgery team.
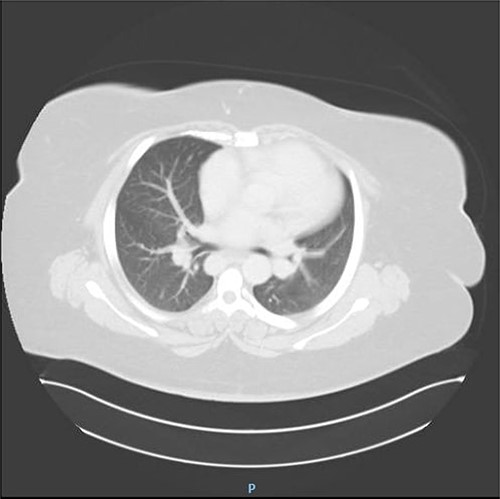
The patient underwent complete preoperative workup which includes clinical history, physical examination, complete blood count (CBC), coagulation profile, chemistry, lipid profile, endocrinology tests, US abdomen, chest X-ray, transthoracic echocardiography, computed tomography (CT) chest and CT abdomen, which showed reversal of intra-abdominal organs as shown in Figs 1, 2 and 3.
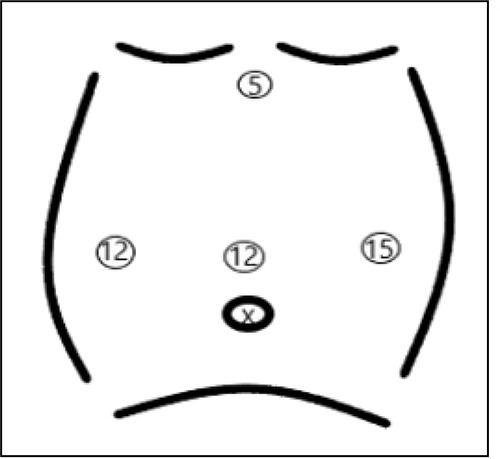
The patient was admitted 1 day before surgery for preoperative monitoring. Following general anaesthesia, patient was put in reverse trendelenburg and French position with the surgeon standing between the legs. Pneumoperitoneum was created using Veress needle which was inserted 2 cm below the right costal margin in the midclavicular line. First, optical trochar of size 12 mm was inserted 15 cm below the xiphoid process. Intra-abdominal exploration was done which confirmed the presence of complete reversal intra-abdominal organs (Fig. 4). Other three trochars of sizes 12, 15 and 5 mm were inserted as shown in Fig. 5.

Omentum was dissected from the greater curvature using Ligasure 5 mm. Gastric tube size 36F was inserted by the anaesthesiologist, reaching the pylorus. Stapling of stomach started 4 cm proximal to the pylorus using Endo GIA Covidien 5 purple colours and the last stapler was tan coloured.
Haemostasis was secured by applying clips to bleeding points along the stapler line. Methelyen blue test confirmed no leak and the specimen was removed via the 15 mm trochar on the left side. All trochars were removed under camera guidance. All trochars sites were closed by skin staplers. The patient was extubated immediately after surgery and sent to recovery room where she stayed for 2 h.
No immediate or later complications happened after the patient was transferred to general ward.
On postoperative Day 1, the patient was doing fine tolerating orally and mobilizing. The patient only developed bradycardia which was treated conservatively by cardiologist. The patient was discharged home on Day 2 with follow-up in our clinic 1 month later. She was seen in clinic 1, 3, 6 and8 months post surgery. Her current BMI is 38 kg/m2.

CT abdomen showing reversal of intra-abdominal organs with polysplenia.

Intra-abdominal exploration showing stomach on the right side of patient.
DISCUSSION
Obesity is a chronic disease that affects 650 millions around the world. In most countries, overweight and obesity kills more people than underweight [4]. Saudi Arabia has higher rates of obesity and deaths attributable to obesity compared with the global average [5]. Currently, bariatric surgery is considered to be the most effective treatment of obesity and metabolic syndrome compared with non-surgical treatment [6]. With the increasing trend of bariatric surgery around the world, rare cases such as SI will be encountered either during preoperative workup or intraoperative during surgery.
SI is a very rare congenital disease affecting one in 10 000 people. It is characterized by a mirror image transposition of both abdominal and thoracic organs where it is called SI totalis or it may involves partially one compartment only [7, 8]. It can be associated with vascular, cardiac, abdominal and respiratory anomalies (Kartagener syndrome). Therefore, it is necessary to diagnose SI preoperatively and to be managed by a multidisciplinary team to avoid perioperative complications [8, 9, 10]. Most of the SI patients do not have clinical problems that are related to their abnormal anatomy and discovered incidentally.
Diagnosing SI preoperatively allows the anaesthesiologist to take all precautions to prevent perioperative respiratory and cardiological complications. Also knowing that patient has SI preoperatively gives the surgeon time to adapt mentally and physically before surgery. The surgeon will plan for trochars placement and team position to avoid technical difficulties [8, 10].
To facilitate cognitive adaptation to reverse anatomy, we advise to review radiological imaging before surgery and using continuous reminders and cross-checks by surgical team during surgery [8, 11]. To overcome technical difficulties, we found that French position gives good exposure and fast adaptation to the reverse anatomy of stomach [8, 9, 10] .
If difficult adhesions are encountered, we advise a right-handed surgeon not to use the left hand for dissection here. The surgeon also should have low threshold to add more trochars in case of difficult dissection. Post-operatively, patient should be monitored for possible anaesthesia complications.
Regarding surgical complications, it is reported in literature that laparoscopic sleeve gastrectomy is safe in patients with SI if diagnosed preoperatively and managed by multidisciplinary team. Surgical complications that reported being related to abnormal anatomy were splenic infarctions with patients with polysplenism [8]. However, our patient has polysplenia and no immediate or late surgical complications happened. The patient was followed for 8 months where she lost ~50% of her excess weight loss.
CONCLUSION
SI is a very rare congenital disease. With increasing trend of bariatric surgery being used as an effective treatment for obesity, such rare cases will be encountered more effectively. It is safe to do sleeve gastrectomy in patients with SI if the diagnosis is made before surgery and all precautions are taken into consideration before and after the surgery.
CONFLICT OF INTEREST STATEMENT
Authors declare no conflicts of interest.
FUNDING
None.
PATIENT CONSENT
The authors certify that they have obtained all appropriate patient consent.
References



