-
PDF
- Split View
-
Views
-
Cite
Cite
Patricia Rodríguez-Zamorano, María Galán-Olleros, Javier Garcia-Coiradas, Sergio Llanos, José Antonio Valle-Cruz, Fernando Marco, Simultaneous bilateral extracapsular proximal femur fractures in the elderly. A case report, Journal of Surgical Case Reports, Volume 2022, Issue 7, July 2022, rjac313, https://doi.org/10.1093/jscr/rjac313
Close - Share Icon Share
Abstract
Simultaneous and bilateral proximal femoral fractures (PFF) are rare and have scarcely been reported in the literature. A case of a bilateral extracapsular PFF is herein presented. Besides, an exhaustive review of the literature was performed, analyzing the information of all previously reported cases.
An 81-year-old woman, who suffered a casual fall, was diagnosed with bilateral PFF consisting of both a subtrochanteric and an intertrochanteric fracture. She underwent concurrent intramedullary fixation for both fractures without any relevant complication and started early ambulation. Simultaneous bilateral extracapsular PFF are exceptional, with only 23 cases described in the current literature. In the elderly, they deserve special attention with treatment strategies in between the ones for unilateral hip fractures and those provided to old multiply injured patients. PFF management is not well established. Minimal reaming and careful nailing can be safely performed bilaterally under close monitoring, in order to start an early functional recovery.
INTRODUCTION
Simultaneous and bilateral proximal femoral fractures (PFF) are rare and have scarcely been reported in the literature. This fracture pattern has generally been described for femoral neck fractures and in association with high-energy trauma, systemic diseases that involve bone structure alterations (primary hyperparathyroidism, multiple myeloma, metastatic disease, chronic kidney failure or cirrhosis) and as a result of violent seizures [1]. Even more exceptionally, some simultaneous and bilateral extracapsular PFF have been reported in relation to high-energy trauma, though they have very rarely been described after low-energy trauma.
A case of a bilateral extracapsular PFF in an octogenarian woman is herein presented.
CASE REPORT
An 81-year-old woman who suffered a casual fall presented at our emergency department. She had a history of arterial hypertension, dyslipidemia, atrial fibrillation (anticoagulated with acenocoumarol®) and stage III chronic kidney disease. She lived together with her grandchildren, was independent for the basic activities of daily living, her Charlson Comorbidity Index was 4 points, and she scored 95 points on Barthel scale and 8 on Parker’s. She denied a history of osteoporosis or fragility fractures, although she was on regular treatment with calcium and vitamin D.
On examination, external rotation deformity of both lower limbs was evident, as well as pain upon palpation in the trochanteric region and during mobilization. The radiological study revealed a left and a right intertrochanteric femur fracture (Fig. 1). She was given analgesia, immobilized with two cutaneous tractions (Fig. 2), and was admitted to the Orthogeriatric Unit.
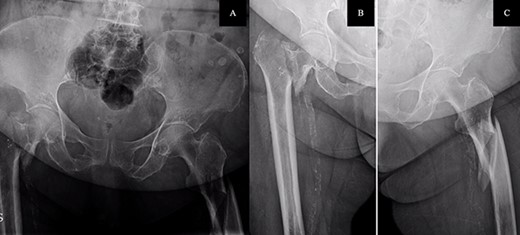
A. Anteroposterior pelvis radiograph evidencing a left subtrochanteric (AO:32-B2a) and a right intertrochanteric femur fracture (AO:31-A2.3). B. Radiograph of the right hip without any criteria of fracture instability. C. Radiograph of the left hip showing a simple wedge pattern of fracture.

Patient immobilization in the emergency department: each lower limb was temporarily immobilized with a 3-kg skin traction.
On her second day, she presented low levels of calcium (7.9 mg7 dl) and 25-hydroxyvitamin D (15.9 ng/ml) along with high parathyroid hormone levels (132 pg/ml), thus having secondary hyperparathyroidism influenced by renal insufficiency. After optimization of the calcium metabolism and renal function and correction of coagulation parameters with vitamin K administration, she underwent concurrent surgical intervention for both fractures three days after admission. Under general anesthesia, ultrasound-guided bilateral fascia iliaca block, and placement on a radiolucent traction table, the left subtrochanteric fracture was first reduced with percutaneous assistance and synthesized with a reamed endomedular long nail with distal locking screws. After closed reduction, the right intertrochanteric fracture was fixated with a non-reamed short nail with distal dynamic locking screws. Fluoroscopic image controls were acceptable, and there were no intraoperative complications.
The postoperative course was satisfactory, without medical problems apart from non-complicated anemia (Hb 7.9 g/dl), solved with two units of red blood. On the first postoperative day, a radiographic control was completed (Fig. 3) and started early ambulation assisted by physiotherapists. On day twelve, she was transferred to a rehabilitation hospital. Outpatient follow-up visits evolving reasonably well. In the 6-month and 1-year check-up, the consolidation of the fracture was observed in the radiographic study (Fig. 4). No surgical wound problems, infections, or limping were identified. Anti-osteoporotic drug treatment was implemented along with an emphasis on a healthy diet with adequate protein intake and supplementation with calcium and vitamin D.

Postoperative anteroposterior pelvis radiograph: The left subtrochanteric fracture was first reduced with percutaneous assistance and synthesized with a reamed intramedullary long Gamma3 nail (340 mm,125°, Stryker®) with cephalic dynamic locking screw and two static distal locking screws. Then, after closed reduction, the right intertrochanteric fracture was fixated with a non-reamed short Gamma3 nail (180 mm,125°, Stryker®) with cephalic and distal dynamic locking screws.

Radiological evaluation on follow-up at 1 year. Pelvis anteroposterior radiograph view showing signs of consolidation, without evidence of loss of reduction or implant failure.
Outline of the simultaneous bilateral extracapsular or combined intra-extracapsular proximal femur fractures published in the literature up to date
| Study . | N . | Sex . | Age (years) . | Mechanism of injury . | Left fracture . | Left osteosynthesis . | Right fracture . | Right osteosynthesis . | Time to loading . | Associated injuries . | Complications . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Dendrinos et al. (1993) [6] | 3 | Male | 63 | Tractor run over | Subtrochanteric comminuted | Plate-screw | Subtrochanteric comminuted | Plate-screw (+ cannulated screw) | 2 months | Maxillary fracture | Two-stage surgery due to hemodynamic instability (16 red blood cell units) |
| Male | 53 | Car accident | Intertrochanteric comminuted | Plate-screw | Intertrochanteric comminuted | Plate-screw | 17 weeks | Ulna fracture (Sx), Liver laceration (Sx) | Sepsis. Removal of implants | ||
| Male | 26 | Car accident | Subtrochanteric comminuted | Plate-screw | Subtrochanteric comminuted | Plate-screw | 8 weeks | Bilateral acetabular fracture. Forearm fracture (Sx) | Fat embolism syndrome before surgery | ||
| Martínez et al. (2000) [8] | 2 | Male | 86 | Casual fall | Intertrochanteric | Intramedullary Nail Gamma (Stryker®) | Intertrochanteric | Intramedullary Nail Gamma (Stryker®) | No | — | No tolerance to ambulation |
| Female | 84 | Casual fall | Basicervical | Plate-screw DHS (Synthes®) | Basicervical | Plate-screw DHS (Synthes®) | 4 days | — | — | ||
| Bori et al. (2005) [1] | 1 | Male | 23 | Motorcycle accident | Intertrochanteric AO:31-A2.2 | Intramedullary Nail PNF (Synthes®) | Femoral neck AO 31-B1.3 Garden III | 3 Cannulated screw | 15 days (left), 6 weeks (right) | — | Pain or discomfort with implant |
| Bori et al. (2008) [9] | 2 | Female | 78 | Casual fall | Subtrochanteric AO:32-A1.1 | Plate-screw DHS (Synthes®) | Intertrochanteric AO:31- A2.3 | Intramedullary Nail short PNF (Synthes®) | 3 weeks (right), 6 weeks (left) | — | — |
| Female | 82 | Casual fall | Subtrochanteric AO:32-A1.1 | — | Intertrochanteric AO: 31- A1.2 | — | — | — | Hemodynamic instability. Deceased before surgery | ||
| Grisoni et al. (2008) [4] | 8 | Male | 34 | Motorcycle accident | Subtrochanteric | Plate-screw DHS (Synthes®) | Subtrochanteric | Intramedullary Nail (+ cerclage) | — | L3 vertebral, tibial plateau fracture and femoral shaft fractures. | — |
| Male | 44 | Motorcycle accident | Intertrochanteric | Plate-screw DHS (Synthes®) | Subtrochanteric | Intramedullary Nail | — | Distal radius fracture | — | ||
| Female | 53 | Car accident | Intertrochanteric | Plate-screw DHS (Synthes®) | Intertrochanteric | Plate-screw DHS (Synthes®) | — | Tibia and patela fracture | — | ||
| Male | 53 | Car accident | Femoral neck | Cannulated screw | Intertrochanteric | Plate-screw DHS (Synthes®) | — | Severe thoracic trauma | Respiratory failure. Deceased | ||
| Male | 70 | Car run-over | Subtrochanteric | Intramedullary Nail | Subtrochanteric | Intramedullary Nail | — | Intracranial hemorrhage, pneumothorax, humerus fracture | — | ||
| Female | 78 | Car run-over | Intertrochanteric | Intramedullary Nail | Femoral neck | Hemiarthroplasty | — | Distal radius and patella fracture | — | ||
| Female | 86 | Casual fall | Subtrochanteric | Intramedullary Nail | Intertrochanteric | Plate-screw DHS (Synthes®) | — | — | Acute on chronic kidney failure. Deceased | ||
| Female | 88 | Casual fall | Intertrochanteric | Plate-screw DHS (Synthes®) | Intertrochanteric | Plate-screw DHS (Synthes®) | — | — | Pulmonary thromboembolism. Deceased | ||
| Verma et al. (2012) [5] | 4 | Female | 65 | Tractor run over | Subtrochanteric | Plate-screw DHS (Synthes®) | Intertrochanteric | Plate-screw DHS (Synthes®) | 3.5 months | — | — |
| Male | 40 | Bus run-over | Intertrochanteric | — | Intertrochanteric | — | — | Right tibia and fibula fractures. Left leg degloving | Fat embolism syndrome. Deceased before surgery | ||
| Male | 40 | Car run-over | Intertrochanteric | Plate-screw DHS (Synthes®) | Intertrochanteric | Plate-screw DHS (Synthes®) | — | — | —- | ||
| Female | 60 | Casual fall | Intertrochanteric | Plate-screw DHS (Synthes®) | Intertrochanteric | Plate-screw DHS (Synthes®) | 3 months | — | — | ||
| Rajeev et al. (2014) [10] | 1 | Female | 92 | Casual fall (repeated) | Intertrochanteric | Plate-screw DHS (Synthes®) | Intertrochanteric | Plate-screw DHS (Synthes®) | Immediate | — | — |
| Aydın et al. (2015) [11] | 1 | Male | 76 | Casual fall | Intertrochanteric | Intramedullary Nail | Intertrochanteric | Intramedullary Nail | — | — | — |
| Vaishya et al. (2017) [7] | 1 | Male | 47 | Car accident | Intertrochanteric + diaphyseal | Intramedullary Nail T2 (Synthes®) and interlocking screws | Intertrochanteric | Five-hole reversed distal femoral locking plate | 2 months | Rib, patella (Sx) and finger fractures (Sx) | Right femur implant failure. New osteosynthesis at 9 months with an intramedullary Nail T2 (Synthes®) |
| Current report (2022) | 1 | Female | 81 | Casual fall | Subtrochanteric AO: 32-B2a | Intramedullary nail long Gamma (Stryker®) | Intertrochanteric AO: 31-A2.3 | Intramedullary Nail short Gamma (Stryker®) | 2 days | — | — |
| Study . | N . | Sex . | Age (years) . | Mechanism of injury . | Left fracture . | Left osteosynthesis . | Right fracture . | Right osteosynthesis . | Time to loading . | Associated injuries . | Complications . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Dendrinos et al. (1993) [6] | 3 | Male | 63 | Tractor run over | Subtrochanteric comminuted | Plate-screw | Subtrochanteric comminuted | Plate-screw (+ cannulated screw) | 2 months | Maxillary fracture | Two-stage surgery due to hemodynamic instability (16 red blood cell units) |
| Male | 53 | Car accident | Intertrochanteric comminuted | Plate-screw | Intertrochanteric comminuted | Plate-screw | 17 weeks | Ulna fracture (Sx), Liver laceration (Sx) | Sepsis. Removal of implants | ||
| Male | 26 | Car accident | Subtrochanteric comminuted | Plate-screw | Subtrochanteric comminuted | Plate-screw | 8 weeks | Bilateral acetabular fracture. Forearm fracture (Sx) | Fat embolism syndrome before surgery | ||
| Martínez et al. (2000) [8] | 2 | Male | 86 | Casual fall | Intertrochanteric | Intramedullary Nail Gamma (Stryker®) | Intertrochanteric | Intramedullary Nail Gamma (Stryker®) | No | — | No tolerance to ambulation |
| Female | 84 | Casual fall | Basicervical | Plate-screw DHS (Synthes®) | Basicervical | Plate-screw DHS (Synthes®) | 4 days | — | — | ||
| Bori et al. (2005) [1] | 1 | Male | 23 | Motorcycle accident | Intertrochanteric AO:31-A2.2 | Intramedullary Nail PNF (Synthes®) | Femoral neck AO 31-B1.3 Garden III | 3 Cannulated screw | 15 days (left), 6 weeks (right) | — | Pain or discomfort with implant |
| Bori et al. (2008) [9] | 2 | Female | 78 | Casual fall | Subtrochanteric AO:32-A1.1 | Plate-screw DHS (Synthes®) | Intertrochanteric AO:31- A2.3 | Intramedullary Nail short PNF (Synthes®) | 3 weeks (right), 6 weeks (left) | — | — |
| Female | 82 | Casual fall | Subtrochanteric AO:32-A1.1 | — | Intertrochanteric AO: 31- A1.2 | — | — | — | Hemodynamic instability. Deceased before surgery | ||
| Grisoni et al. (2008) [4] | 8 | Male | 34 | Motorcycle accident | Subtrochanteric | Plate-screw DHS (Synthes®) | Subtrochanteric | Intramedullary Nail (+ cerclage) | — | L3 vertebral, tibial plateau fracture and femoral shaft fractures. | — |
| Male | 44 | Motorcycle accident | Intertrochanteric | Plate-screw DHS (Synthes®) | Subtrochanteric | Intramedullary Nail | — | Distal radius fracture | — | ||
| Female | 53 | Car accident | Intertrochanteric | Plate-screw DHS (Synthes®) | Intertrochanteric | Plate-screw DHS (Synthes®) | — | Tibia and patela fracture | — | ||
| Male | 53 | Car accident | Femoral neck | Cannulated screw | Intertrochanteric | Plate-screw DHS (Synthes®) | — | Severe thoracic trauma | Respiratory failure. Deceased | ||
| Male | 70 | Car run-over | Subtrochanteric | Intramedullary Nail | Subtrochanteric | Intramedullary Nail | — | Intracranial hemorrhage, pneumothorax, humerus fracture | — | ||
| Female | 78 | Car run-over | Intertrochanteric | Intramedullary Nail | Femoral neck | Hemiarthroplasty | — | Distal radius and patella fracture | — | ||
| Female | 86 | Casual fall | Subtrochanteric | Intramedullary Nail | Intertrochanteric | Plate-screw DHS (Synthes®) | — | — | Acute on chronic kidney failure. Deceased | ||
| Female | 88 | Casual fall | Intertrochanteric | Plate-screw DHS (Synthes®) | Intertrochanteric | Plate-screw DHS (Synthes®) | — | — | Pulmonary thromboembolism. Deceased | ||
| Verma et al. (2012) [5] | 4 | Female | 65 | Tractor run over | Subtrochanteric | Plate-screw DHS (Synthes®) | Intertrochanteric | Plate-screw DHS (Synthes®) | 3.5 months | — | — |
| Male | 40 | Bus run-over | Intertrochanteric | — | Intertrochanteric | — | — | Right tibia and fibula fractures. Left leg degloving | Fat embolism syndrome. Deceased before surgery | ||
| Male | 40 | Car run-over | Intertrochanteric | Plate-screw DHS (Synthes®) | Intertrochanteric | Plate-screw DHS (Synthes®) | — | — | —- | ||
| Female | 60 | Casual fall | Intertrochanteric | Plate-screw DHS (Synthes®) | Intertrochanteric | Plate-screw DHS (Synthes®) | 3 months | — | — | ||
| Rajeev et al. (2014) [10] | 1 | Female | 92 | Casual fall (repeated) | Intertrochanteric | Plate-screw DHS (Synthes®) | Intertrochanteric | Plate-screw DHS (Synthes®) | Immediate | — | — |
| Aydın et al. (2015) [11] | 1 | Male | 76 | Casual fall | Intertrochanteric | Intramedullary Nail | Intertrochanteric | Intramedullary Nail | — | — | — |
| Vaishya et al. (2017) [7] | 1 | Male | 47 | Car accident | Intertrochanteric + diaphyseal | Intramedullary Nail T2 (Synthes®) and interlocking screws | Intertrochanteric | Five-hole reversed distal femoral locking plate | 2 months | Rib, patella (Sx) and finger fractures (Sx) | Right femur implant failure. New osteosynthesis at 9 months with an intramedullary Nail T2 (Synthes®) |
| Current report (2022) | 1 | Female | 81 | Casual fall | Subtrochanteric AO: 32-B2a | Intramedullary nail long Gamma (Stryker®) | Intertrochanteric AO: 31-A2.3 | Intramedullary Nail short Gamma (Stryker®) | 2 days | — | — |
DHS, Dynamic Hip Screw; Sx, Surgery
Outline of the simultaneous bilateral extracapsular or combined intra-extracapsular proximal femur fractures published in the literature up to date
| Study . | N . | Sex . | Age (years) . | Mechanism of injury . | Left fracture . | Left osteosynthesis . | Right fracture . | Right osteosynthesis . | Time to loading . | Associated injuries . | Complications . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Dendrinos et al. (1993) [6] | 3 | Male | 63 | Tractor run over | Subtrochanteric comminuted | Plate-screw | Subtrochanteric comminuted | Plate-screw (+ cannulated screw) | 2 months | Maxillary fracture | Two-stage surgery due to hemodynamic instability (16 red blood cell units) |
| Male | 53 | Car accident | Intertrochanteric comminuted | Plate-screw | Intertrochanteric comminuted | Plate-screw | 17 weeks | Ulna fracture (Sx), Liver laceration (Sx) | Sepsis. Removal of implants | ||
| Male | 26 | Car accident | Subtrochanteric comminuted | Plate-screw | Subtrochanteric comminuted | Plate-screw | 8 weeks | Bilateral acetabular fracture. Forearm fracture (Sx) | Fat embolism syndrome before surgery | ||
| Martínez et al. (2000) [8] | 2 | Male | 86 | Casual fall | Intertrochanteric | Intramedullary Nail Gamma (Stryker®) | Intertrochanteric | Intramedullary Nail Gamma (Stryker®) | No | — | No tolerance to ambulation |
| Female | 84 | Casual fall | Basicervical | Plate-screw DHS (Synthes®) | Basicervical | Plate-screw DHS (Synthes®) | 4 days | — | — | ||
| Bori et al. (2005) [1] | 1 | Male | 23 | Motorcycle accident | Intertrochanteric AO:31-A2.2 | Intramedullary Nail PNF (Synthes®) | Femoral neck AO 31-B1.3 Garden III | 3 Cannulated screw | 15 days (left), 6 weeks (right) | — | Pain or discomfort with implant |
| Bori et al. (2008) [9] | 2 | Female | 78 | Casual fall | Subtrochanteric AO:32-A1.1 | Plate-screw DHS (Synthes®) | Intertrochanteric AO:31- A2.3 | Intramedullary Nail short PNF (Synthes®) | 3 weeks (right), 6 weeks (left) | — | — |
| Female | 82 | Casual fall | Subtrochanteric AO:32-A1.1 | — | Intertrochanteric AO: 31- A1.2 | — | — | — | Hemodynamic instability. Deceased before surgery | ||
| Grisoni et al. (2008) [4] | 8 | Male | 34 | Motorcycle accident | Subtrochanteric | Plate-screw DHS (Synthes®) | Subtrochanteric | Intramedullary Nail (+ cerclage) | — | L3 vertebral, tibial plateau fracture and femoral shaft fractures. | — |
| Male | 44 | Motorcycle accident | Intertrochanteric | Plate-screw DHS (Synthes®) | Subtrochanteric | Intramedullary Nail | — | Distal radius fracture | — | ||
| Female | 53 | Car accident | Intertrochanteric | Plate-screw DHS (Synthes®) | Intertrochanteric | Plate-screw DHS (Synthes®) | — | Tibia and patela fracture | — | ||
| Male | 53 | Car accident | Femoral neck | Cannulated screw | Intertrochanteric | Plate-screw DHS (Synthes®) | — | Severe thoracic trauma | Respiratory failure. Deceased | ||
| Male | 70 | Car run-over | Subtrochanteric | Intramedullary Nail | Subtrochanteric | Intramedullary Nail | — | Intracranial hemorrhage, pneumothorax, humerus fracture | — | ||
| Female | 78 | Car run-over | Intertrochanteric | Intramedullary Nail | Femoral neck | Hemiarthroplasty | — | Distal radius and patella fracture | — | ||
| Female | 86 | Casual fall | Subtrochanteric | Intramedullary Nail | Intertrochanteric | Plate-screw DHS (Synthes®) | — | — | Acute on chronic kidney failure. Deceased | ||
| Female | 88 | Casual fall | Intertrochanteric | Plate-screw DHS (Synthes®) | Intertrochanteric | Plate-screw DHS (Synthes®) | — | — | Pulmonary thromboembolism. Deceased | ||
| Verma et al. (2012) [5] | 4 | Female | 65 | Tractor run over | Subtrochanteric | Plate-screw DHS (Synthes®) | Intertrochanteric | Plate-screw DHS (Synthes®) | 3.5 months | — | — |
| Male | 40 | Bus run-over | Intertrochanteric | — | Intertrochanteric | — | — | Right tibia and fibula fractures. Left leg degloving | Fat embolism syndrome. Deceased before surgery | ||
| Male | 40 | Car run-over | Intertrochanteric | Plate-screw DHS (Synthes®) | Intertrochanteric | Plate-screw DHS (Synthes®) | — | — | —- | ||
| Female | 60 | Casual fall | Intertrochanteric | Plate-screw DHS (Synthes®) | Intertrochanteric | Plate-screw DHS (Synthes®) | 3 months | — | — | ||
| Rajeev et al. (2014) [10] | 1 | Female | 92 | Casual fall (repeated) | Intertrochanteric | Plate-screw DHS (Synthes®) | Intertrochanteric | Plate-screw DHS (Synthes®) | Immediate | — | — |
| Aydın et al. (2015) [11] | 1 | Male | 76 | Casual fall | Intertrochanteric | Intramedullary Nail | Intertrochanteric | Intramedullary Nail | — | — | — |
| Vaishya et al. (2017) [7] | 1 | Male | 47 | Car accident | Intertrochanteric + diaphyseal | Intramedullary Nail T2 (Synthes®) and interlocking screws | Intertrochanteric | Five-hole reversed distal femoral locking plate | 2 months | Rib, patella (Sx) and finger fractures (Sx) | Right femur implant failure. New osteosynthesis at 9 months with an intramedullary Nail T2 (Synthes®) |
| Current report (2022) | 1 | Female | 81 | Casual fall | Subtrochanteric AO: 32-B2a | Intramedullary nail long Gamma (Stryker®) | Intertrochanteric AO: 31-A2.3 | Intramedullary Nail short Gamma (Stryker®) | 2 days | — | — |
| Study . | N . | Sex . | Age (years) . | Mechanism of injury . | Left fracture . | Left osteosynthesis . | Right fracture . | Right osteosynthesis . | Time to loading . | Associated injuries . | Complications . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Dendrinos et al. (1993) [6] | 3 | Male | 63 | Tractor run over | Subtrochanteric comminuted | Plate-screw | Subtrochanteric comminuted | Plate-screw (+ cannulated screw) | 2 months | Maxillary fracture | Two-stage surgery due to hemodynamic instability (16 red blood cell units) |
| Male | 53 | Car accident | Intertrochanteric comminuted | Plate-screw | Intertrochanteric comminuted | Plate-screw | 17 weeks | Ulna fracture (Sx), Liver laceration (Sx) | Sepsis. Removal of implants | ||
| Male | 26 | Car accident | Subtrochanteric comminuted | Plate-screw | Subtrochanteric comminuted | Plate-screw | 8 weeks | Bilateral acetabular fracture. Forearm fracture (Sx) | Fat embolism syndrome before surgery | ||
| Martínez et al. (2000) [8] | 2 | Male | 86 | Casual fall | Intertrochanteric | Intramedullary Nail Gamma (Stryker®) | Intertrochanteric | Intramedullary Nail Gamma (Stryker®) | No | — | No tolerance to ambulation |
| Female | 84 | Casual fall | Basicervical | Plate-screw DHS (Synthes®) | Basicervical | Plate-screw DHS (Synthes®) | 4 days | — | — | ||
| Bori et al. (2005) [1] | 1 | Male | 23 | Motorcycle accident | Intertrochanteric AO:31-A2.2 | Intramedullary Nail PNF (Synthes®) | Femoral neck AO 31-B1.3 Garden III | 3 Cannulated screw | 15 days (left), 6 weeks (right) | — | Pain or discomfort with implant |
| Bori et al. (2008) [9] | 2 | Female | 78 | Casual fall | Subtrochanteric AO:32-A1.1 | Plate-screw DHS (Synthes®) | Intertrochanteric AO:31- A2.3 | Intramedullary Nail short PNF (Synthes®) | 3 weeks (right), 6 weeks (left) | — | — |
| Female | 82 | Casual fall | Subtrochanteric AO:32-A1.1 | — | Intertrochanteric AO: 31- A1.2 | — | — | — | Hemodynamic instability. Deceased before surgery | ||
| Grisoni et al. (2008) [4] | 8 | Male | 34 | Motorcycle accident | Subtrochanteric | Plate-screw DHS (Synthes®) | Subtrochanteric | Intramedullary Nail (+ cerclage) | — | L3 vertebral, tibial plateau fracture and femoral shaft fractures. | — |
| Male | 44 | Motorcycle accident | Intertrochanteric | Plate-screw DHS (Synthes®) | Subtrochanteric | Intramedullary Nail | — | Distal radius fracture | — | ||
| Female | 53 | Car accident | Intertrochanteric | Plate-screw DHS (Synthes®) | Intertrochanteric | Plate-screw DHS (Synthes®) | — | Tibia and patela fracture | — | ||
| Male | 53 | Car accident | Femoral neck | Cannulated screw | Intertrochanteric | Plate-screw DHS (Synthes®) | — | Severe thoracic trauma | Respiratory failure. Deceased | ||
| Male | 70 | Car run-over | Subtrochanteric | Intramedullary Nail | Subtrochanteric | Intramedullary Nail | — | Intracranial hemorrhage, pneumothorax, humerus fracture | — | ||
| Female | 78 | Car run-over | Intertrochanteric | Intramedullary Nail | Femoral neck | Hemiarthroplasty | — | Distal radius and patella fracture | — | ||
| Female | 86 | Casual fall | Subtrochanteric | Intramedullary Nail | Intertrochanteric | Plate-screw DHS (Synthes®) | — | — | Acute on chronic kidney failure. Deceased | ||
| Female | 88 | Casual fall | Intertrochanteric | Plate-screw DHS (Synthes®) | Intertrochanteric | Plate-screw DHS (Synthes®) | — | — | Pulmonary thromboembolism. Deceased | ||
| Verma et al. (2012) [5] | 4 | Female | 65 | Tractor run over | Subtrochanteric | Plate-screw DHS (Synthes®) | Intertrochanteric | Plate-screw DHS (Synthes®) | 3.5 months | — | — |
| Male | 40 | Bus run-over | Intertrochanteric | — | Intertrochanteric | — | — | Right tibia and fibula fractures. Left leg degloving | Fat embolism syndrome. Deceased before surgery | ||
| Male | 40 | Car run-over | Intertrochanteric | Plate-screw DHS (Synthes®) | Intertrochanteric | Plate-screw DHS (Synthes®) | — | — | —- | ||
| Female | 60 | Casual fall | Intertrochanteric | Plate-screw DHS (Synthes®) | Intertrochanteric | Plate-screw DHS (Synthes®) | 3 months | — | — | ||
| Rajeev et al. (2014) [10] | 1 | Female | 92 | Casual fall (repeated) | Intertrochanteric | Plate-screw DHS (Synthes®) | Intertrochanteric | Plate-screw DHS (Synthes®) | Immediate | — | — |
| Aydın et al. (2015) [11] | 1 | Male | 76 | Casual fall | Intertrochanteric | Intramedullary Nail | Intertrochanteric | Intramedullary Nail | — | — | — |
| Vaishya et al. (2017) [7] | 1 | Male | 47 | Car accident | Intertrochanteric + diaphyseal | Intramedullary Nail T2 (Synthes®) and interlocking screws | Intertrochanteric | Five-hole reversed distal femoral locking plate | 2 months | Rib, patella (Sx) and finger fractures (Sx) | Right femur implant failure. New osteosynthesis at 9 months with an intramedullary Nail T2 (Synthes®) |
| Current report (2022) | 1 | Female | 81 | Casual fall | Subtrochanteric AO: 32-B2a | Intramedullary nail long Gamma (Stryker®) | Intertrochanteric AO: 31-A2.3 | Intramedullary Nail short Gamma (Stryker®) | 2 days | — | — |
DHS, Dynamic Hip Screw; Sx, Surgery
DISCUSSION
PFF entails considerable individual, social and economic impact, mainly due to its high incidence in the elderly and associated functional impairment [2]. The lifetime risk of unilateral hip fracture is estimated to be high, ranging from 40 to 50% in women and from 13 to 22% in men [3]. However, bilateral and simultaneous PFF are rare and hardly described in the literature [2]. In fact, only 23 bilateral and simultaneous extracapsular or combined intra-extracapsular PFF cases have been reported to date (Table 1). In the largest series, Grisoni et al. [4] reported eight cases over 10 years, the estimated frequency being 0.3% of the total number of hip fractures attended, while Verma et al., [5] in their series of 4 cases over 3 years, estimate a similar rate of 0.24%. This low reported incidence challenges the acquisition of experience in the management of these combined fractures; therefore, only one literature review on its management has been described to date [2].
When analyzing the published cases of simultaneous bilateral extracapsular fractures, three profiles can be identified. (i) Young patients involved in traffic accident with multiple associated injuries [1, 4–7] in which the definitive surgical intervention was sometimes delayed, having an impact on the overall survival. (ii) Patients aged 65–75 years old with fractures in the context of high-energy accidents [4–6]. (iii) Patients over 80 years who sustain fragility fractures after casual falls from their height [4, 8–11], in which the current case is included.
To date, despite the extensive literature on the subject, there are still many controversies regarding the surgical treatment of extracapsular hip fractures. We opted for intramedullary fixation as it seems to have advantages over extramedullary fixation, such as shorter surgical time and length of stay, less soft tissue injury and blood loss and less time until loading. Even though the failure rate of nailing appears to be higher than that of extramedullary systems [12], intramedullary fixation is currently the most oft-used surgical technique. In the cases examined, there is a great deal of variability in the type of surgical technique, probably related to the point in time when the surgeries were performed, the surgeon’s experience and the available resources.
As far as nailing, there is, an open debate at present around the need to ream the medullary canal, especially in patients with comorbidities and multiple injuries. Reaming allows the use of a wider nail diameter and improving bone-implant contact area while main disadvantages are that reaming reduces endosteal circulation, has systemic effects given the possibility of embolism and increases surgical time. For unilateral femoral shaft fractures, non-reamed nailing may have a role in polytrauma patients or those with significant respiratory compromise in whom quickness and blood loss minimization are essential. In our case, we decided only to ream the long nail, to successfully surpass the femoral isthmus and decrease the risk of intraoperative fracture, while we opted not to ream the short nail to minimize the risks associated with a bilateral procedure. The incidence of adult respiratory distress syndrome is also considered significantly higher in bilateral fractures [13]. Additionally, fat embolism syndrome (FES) in bilateral femur fractures has been reported to be higher than in unilateral ones (1–10%) [14]. However, Bonnevialle et al. [15] concluded that simultaneous nailing could be safely performed with minimal reaming without an increase in the risk of FES.
The average length of hospitalization in the review is about 29 days in the older patients compared to the average hospitalization for unilateral fragility hip fracture in our country: 9–11 days [16]. Concerning mortality, although no robust data are reported, it is considerably higher than for unilateral cases. Grisoni et al. [4] reported an in-hospital mortality for young patients of 25% [4]. On the other hand, the same authors found an in-hospital mortality rate for older patients as high as 50%, compared to 4.38% for unilateral hip fractures [16].
In conclusion, simultaneous bilateral extracapsular PFF are exceptional, severe and life-threatening. A total of 24 of these fractures have been described in the literature considering this report; hence, their management is not well established, and even less so for the elderly subgroup of patients who have high morbimortality. Proper medical and surgical stabilization, in addition to early mobilization, are priorities. Minimal reaming and careful nailing can be safely performed bilaterally under close monitoring, allowing the surgery to be performed at one time in order to start an early functional recovery [2].
CONFLICT OF INTEREST STATEMENT
The authors or their immediate families, and any research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article.
FUNDING
None.



