-
PDF
- Split View
-
Views
-
Cite
Cite
Sofia Ridolfo, Francesco Cammarata, Alessandro M Bonomi, Albert Troci, Michele Crespi, Paola Molteni, Alessandro Pellegrinelli, Sandro Ardizzone, Piergiorgio Danelli, Gastrointestinal tuberculosis presenting as acute abdomen: a case report, Journal of Surgical Case Reports, Volume 2022, Issue 6, June 2022, rjac305, https://doi.org/10.1093/jscr/rjac305
Close - Share Icon Share
Abstract
Intestinal tuberculosis (ITB) represents an important diagnostic challenge in the clinical setting, as it generally can occur as a chronic condition often mimicking other diseases such as Crohn’s disease (CD), and can present itself with acute onset, which can be life-threatening. A 29-years-old Chinese woman coming to ER with abdominal pain, fever and weight loss. Computed tomography and colonoscopy images were not diagnostic. Despite medical therapy, the patient progressively worsened developing sepsis requiring emergency surgery. Pathological and microbiological examination of the colon both pointed towards gastrointestinal tuberculosis involvement. Although ITB is generally a chronic-wasting condition, it can also occur as acute abdomen representing an absolute surgical emergency. Although caseation and necrosis in granulomas can be used for diagnosis of ITB, preoperative diagnosis is still challenging. Endoscopic biopsies targeted to ulcerous lesions could be an essential diagnostic tool, contrary to those targeted to the ulcers’ edges as performed in CD.
KEY CLINICAL MESSAGE
Although gastrointestinal tuberculosis is generally a chronic-wasting condition, it can also occur as acute abdomen representing an absolute surgical emergency. We therefore highlight the importance of suspecting ITB when evaluating patients with ulcers.
INTRODUCTION
Intestinal tuberculosis (ITB) represents an important diagnostic challenge in the clinical setting even for more experienced physicians, as it can mimic other gastrointestinal diseases such as Crohn’s disease (CD). It generally presents as a chronic condition with an insidious onset, non-specific signs and symptoms but sometimes it can occur with an acute abdominal presentation, which can be life-threatening, thus requiring more intensive management and surgical intervention.
CASE REPORT
We present the case of a 29-year-old Chinese female, Height 1,59 m, weight 35 kg and BMI 13,8, who came into the ER in February 2021 with abdominal pain, fever, weight loss, bloody diarrhea the previous week, but neither nausea nor vomit. Her clinical history began in 2016 but in 2020 abdominal pain became more frequent, associated with asthenia and weight loss (7 kg in a year). Her previous medical history was negative.
The following tests were carried out in ER: swab for severe acute respiratory syndrome coronavirus 2 (SARS-CoV2; negative), electrocardiogram, blood tests showing normocytic anemia, without leukocytosis, mild lymphocytopenia, and elevated C-reactive protein (CRP, 47 mg/L), chest X-ray (negative). Contrast-enhanced computed tomography (CT) showed increased densification of adipose tissue along the whole colon, the cecum and part of the ascendant had thickened walls (Fig. 1, panel A and B) with enhancement of the mucosa and submucosa edema, locoregional lymphoglandular large ~2 cm also partially colliquate (Fig. 1, panel C and D); lumen narrowing and strictures along the preterminal ileum and ascites. A colonscopy was performed, which revealed a patulous ileocecal valve, a bowel that was completely subverted from the cecum to the hepatic flexure with multiple and extensive deep fibrin-coated ulcers; the residual mucosa appeared pink with multiple pseudopolipoid protrusions (Fig. 2). Tests for HIV, HCV, stool cultures, parasitological and Clostridium difficile toxin were all negative and she was immune to hepatitis B virus. Quantiferon-test still outstanding.
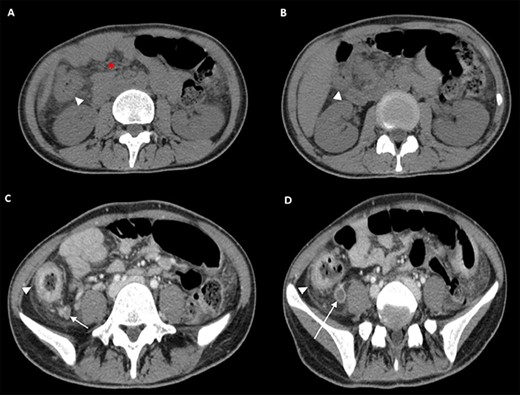
CT scan of the Abdomen obtained at this presentation. Transverse CT images (Panel A and B), obtained before administration of intravenous contrast material, show increased densification of adipose tissue (asterisk) along the whole colon, the cecum and part of the ascendant, which had thickened walls (arrowheads). Transverse CT images (Panel C and D), obtained after administration of intravenous contrast material, show the mucosa enhancement and submucosa edema due to flogosis (arrowheads), locoregional lymphoglandular also partially colliquate (arrows).
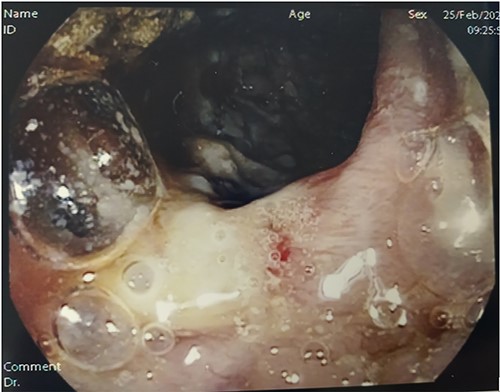
Colonoscopy. Digital photograph from optical colonoscopy shows the endoscopic capture of suffering and ischemic mucosa with deep fibrin-coated ulcers.
An entero-MRI was carried out, which highlighted another intestinal loop thickened. The patient then got a lot worse. She was in septic shock (102/66 mmHg and, 108 bpm) and hyperventilating; she had acute abdomen with a positive Blumberg sign and was tachypnoeic with 95% oxygen saturation. Surgeons were consulted and indication for exploratory laparotomy was given considering the clinical picture of sepsis and initial haemodynamic instability. Although the patient was preparing for surgery, Quantiferon-test result arrived with a positive result. At surgical intervention, abundant yellowish peritoneal effusion was found and sent to microbiological examination. The right colon was markedly altered and fibrotic, with multiple mesenterial nodes and miliary whitish granular dissemination on the right colon visceral peritoneum and peritoneal right-side wall. At 20-cm proximal to ileocecal valve, a hard and fibrotic lesion infiltrating the same ileal loop near the valve and a 20–30 cm further ileal double stricture were observed. The macroscopical presentation was more compatible with ITB than with CD or cancer. The bacterial translocation sepsis caused by TBC, which produced a severe right colon subversion therefore it was an absolute surgical emergency. Hence, a right hemicolectomy (Fig. 3, panel A) was performed. An ileal resection using the ileal stumps for a temporary loop ileostomy was preferred for the ileal stricture due to the clinical severity and the uncertain diagnosis, as an alternative to strictureplasty. A mesenteric lymph node sent to microbiological examination resulted positive on PCR for Mycobacterium tuberculosis, confirming ITB (Fig. 3, panel B and Fig. 4, panel A).
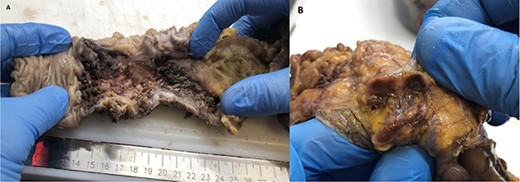
Operating pieces. Panel A shows right colon with a subverted mucosa; in particular, the blackish color indicates a suffering and ischemic mucosa. Panel B shows dissected pathological lymph node on which TBC diagnosis was made.
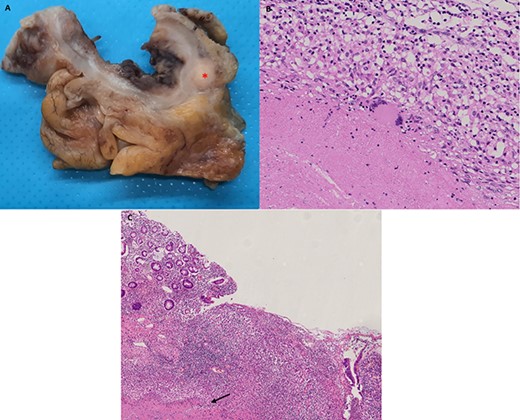
Histopathology of operative specimen. Panel A shows operating piece fixed with formalin: in panel A a large lymph node touched by disease is visible (asterisk). Panel B shows typical TB granuloma with caseation necrosis, lymphocytes, macrophages and also Giant cells. Panel C shows ulcer covered with fibrin and under granulation tissue. Under ulcer, there is caseation necrosis (arrow). Endoscopist should have to perform biopsies here to increase exam sensitivity.
Post-operative clinical course had no complications from a surgical point of view, expect from an episode of liver toxicity due to antitubercular drug regimen, which had probably been introduced too early after surgery in addition to the post-operative pain relief medications essential in this phase. Liver toxicity regressed in a few days after stopping the TBC medications. The antitubercular therapy was then reintroduced in the following weeks. After a year she completed the therapy, and the stoma was closed.
DISCUSSION
ITB accounts for 1–3% of all TB cases worldwide. In the past, TB was thought to be associated with active pulmonary disease, but there is an increase evidence it can occur as a primary infection without evidence of pulmonary infection [1]. Among extra-pulmonary forms, intestinal involvement is less common than the one involving the genito-urinary tract, bone and meninges, yet it may cause significant morbidity and death. In a large retrospective study 6% of 66 034 admissions associated with tuberculosis had acute abdomen [2, 3]. Mycobacterium tuberculosis is the pathogen responsible for the majority of cases of ITB. Mycobacterium bovis is responsible for cases related to ingestion of infected dairy products. The principal route of infection is swallowing micro-organisms through sputum or contaminated liquids/food [4]. The mucosal layer of GI tract can be infected by bacilli forming epithelioid tubercles in the submucosa lymphoid tissue. Caseous necrosis of the tubercles, after 2–4 weeks, leads to ulceration of the overlying mucosa and it can later spread into the deeper layers, adjacent lymph nodes and into the peritoneum [5]. Mycobacterium can affect any region of the GI tract, even if the ileum and cecum are the most common sites. Various factors such as intestinal fluid stasis, presence of abundant lymphoid tissue, increased absorption rate at this site and close contact of the bacilli with the mucosa contribute to the terminal ileum infection [6]. ITB can manifest itself in three distinct phenotypes: ulcerative, hypertrophic and ulcerohypertrophic, with the ulcerative type being the most common. Ulcerative disease usually shows transverse ulcers often superficial and heal by fibrosis. Hypertrophic forms show thickening and a mass-like appearance of the bowel associated with scarring and fibrosis [1]. ITB can mimic other diseases including CD, as their clinical manifestations non-specific: the most common patient complaint is chronic abdominal pain. Clinical features are diarrhoea, haematochezia, perianal disease and extraintestinal manifestations, which point to CD diagnosis, whereas fever, night sweats, lung involvement and ascites indicate ITB diagnosis. Endoscopic features such as left colonic involvement, presence of longitudinal ulcers, aphthous ulcers, cobblestoning and skip lesions are more common in CD, whereas presence of transverse ulcers and patulous ileocecal valve are more common in ITB. Both CD and ITB are characterized by chronic granulomatous inflammation: both size and number of granulomas were higher in ITB than in CD. Giant cells, caseation necrosis, confluent granulomas and granuloma with lymphoid cuff were more frequently associated with ITB [7] (Fig. 4 panel B). Although caseation and necrosis in granulomas or positive stain for AFB is virtually diagnosis for ITB, the poor yield of endoscopic sampling results in the disease being diagnosed in <30% [8]. In CD, the endoscopist performs biopsies on the mucosa adjacent to the ulcerated mucosa; if ITB is suspected, biopsies should be carried out in the ulcerated area resulting from the underlying caseation necrosis (Fig. 4, panel C).
ACKNOWLEDGEMENTS
The authors acknowledge the support of the APC central fund of the University of Milan.
CONFLICT OF INTEREST STATEMENT
All authors declare that they have no conflict of interest. (Informed consent was obtained from the patient being included in the study.)
FUNDING
No funding were received to conduct this study. Article processing charges were kindly covered by University of Milan.
References
- sepsis
- cachexia
- abdominal pain
- acute abdomen
- computed tomography
- weight reduction
- colonoscopy
- crohn's disease
- ulcer
- fever
- chronic disease
- granuloma
- necrosis
- preoperative care
- gastrointestinal tuberculosis
- colon
- diagnosis
- intestinal tuberculosis
- clinical diagnostic instrument
- biopsy, endoscopic
- emergency surgical procedure
- medical management



