-
PDF
- Split View
-
Views
-
Cite
Cite
Sreekumar Sundara Rajan, Rashmi Verma, Bade L Murthy, Chest wall perforator flap to partially reconstruct central mound of breast tissue – evolution of the technique, Journal of Surgical Case Reports, Volume 2022, Issue 6, June 2022, rjac276, https://doi.org/10.1093/jscr/rjac276
Close - Share Icon Share
Abstract
We describe the use of chest wall perforator flap (CWPF) to reconstruct the central mound of breast tissue in women presenting with central/retro areolar breast cancer. We describe the results of seven patients (median age, 59 years) with a median follow-up of 9 months. We were able to conserve the breast in all except one woman who was found to have extensive DCIS. Two patients were taken back to theatre, one for a washout of infected seroma and second for a wound debridement. There was no flap loss or donor site complications in our series. We were able to conserve the breast, maintain aesthetic contour of the central mound along with projection and achieve excellent cosmetic outcome for our patients. Partial breast reconstruction using CWPF provides an oncologically safe and cosmetically superior alternative in selected women with breast cancer needing central wide local excision.
INTRODUCTION
The introduction of chest wall perforator flap (CWPF) to partially reconstruct breast [1, 2] has revolutionized the way an Oncoplastic surgeon can approach breast conserving surgery. The consistent and robust nature of various chest wall perforators has led to its widespread acceptance amongst oncoplastic breast surgeons and plastic surgeons. A central excision with removal of the nipple and areola is usually recommended as an alternative to simple mastectomy for Paget’s disease, invasive and in situ breast cancer involving or close to the nipple and areola complex. There are various surgical techniques including Grissoti flap, vertical or transverse incision wedge mammoplasty described in literature to approach a central wide local excision by adhering to oncoplastic principles [3, 4]. The disadvantage of these methods being the loss of projection and/or the need for contralateral symmetrization surgery. The main challenge faced by an Oncoplastic surgeon in such circumstances is to maintain the aesthetic contour and shape of the breast after excising the nipple-areola complex without compromising the oncological safety and avoiding box deformity. In this case series, we describe a surgical approach for partial breast reconstruction following central wide local excision and the use of skin island to facilitate future reconstruction of nipple-areola complex.
RESULTS
We present the oncological and cosmetic outcomes of seven consecutive patients who underwent central wide local excision and CWPF reconstruction from 01 January 2021 to 31 October 2021 at Central Lancashire Breast Unit (Table 1). All patients presented symptomatically, and the median age was 59 years (range, 44–74). The pre and postoperative outcome of a women who presented with Paget’s disease of the nipple (Patient 5) is depicted in Fig. 1. The preoperative marking (Fig. 1A and B) shows the two areas considered for the future skin paddle. The lateral marked area was used for creating the skin paddle for the central mound and medial end of the flap was used for achieving projection in this patient. The postoperative outcome (Fig. 1C–F) clearly demonstrates the aesthetic contour of the breast maintained with good symmetry.
| Case no: . | Age . | Pre-op distance of cancer from NAC (mm) . | Type of cancer . | Grade of Invasive/ In-situ cancer . | Whole tumour size (mm) . | Axillary surgery . | Nodal status . | Further surgery . | Complications . | Follow-up in months . |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 63 | 3 | IMC | 2 | 39 | SLNB | Negative | Re-excision of inferior margin | Organized small haematoma on USS at 9 months | 12 |
| 2 | 74 | 4 | IDC | 3 | 28 | SLNB | Negative | None | NA | 11 |
| 3 | 58 | <1 | IDC | 2 | 25 | SLNB | Negative | None | Partial skin necrosis | 10 |
| 4 | 66 | 6 | IDC | 2 | 50 | ANC | 1 of 28 | Completion mastectomy | NA | 10 |
| 5 | 44 | NA | Paget’s | HG | 20 | SLNB | Negative | None | NA | 7 |
| 6 | 57 | <1 | IDC | 2 | 15 | SLNB | Negative | None | Infected seroma | 5 |
| 7 | 48 | 1 | IDC | 3 | 35 | ANC | 1 of 15 | None | NA | 5 |
| Case no: . | Age . | Pre-op distance of cancer from NAC (mm) . | Type of cancer . | Grade of Invasive/ In-situ cancer . | Whole tumour size (mm) . | Axillary surgery . | Nodal status . | Further surgery . | Complications . | Follow-up in months . |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 63 | 3 | IMC | 2 | 39 | SLNB | Negative | Re-excision of inferior margin | Organized small haematoma on USS at 9 months | 12 |
| 2 | 74 | 4 | IDC | 3 | 28 | SLNB | Negative | None | NA | 11 |
| 3 | 58 | <1 | IDC | 2 | 25 | SLNB | Negative | None | Partial skin necrosis | 10 |
| 4 | 66 | 6 | IDC | 2 | 50 | ANC | 1 of 28 | Completion mastectomy | NA | 10 |
| 5 | 44 | NA | Paget’s | HG | 20 | SLNB | Negative | None | NA | 7 |
| 6 | 57 | <1 | IDC | 2 | 15 | SLNB | Negative | None | Infected seroma | 5 |
| 7 | 48 | 1 | IDC | 3 | 35 | ANC | 1 of 15 | None | NA | 5 |
| Case no: . | Age . | Pre-op distance of cancer from NAC (mm) . | Type of cancer . | Grade of Invasive/ In-situ cancer . | Whole tumour size (mm) . | Axillary surgery . | Nodal status . | Further surgery . | Complications . | Follow-up in months . |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 63 | 3 | IMC | 2 | 39 | SLNB | Negative | Re-excision of inferior margin | Organized small haematoma on USS at 9 months | 12 |
| 2 | 74 | 4 | IDC | 3 | 28 | SLNB | Negative | None | NA | 11 |
| 3 | 58 | <1 | IDC | 2 | 25 | SLNB | Negative | None | Partial skin necrosis | 10 |
| 4 | 66 | 6 | IDC | 2 | 50 | ANC | 1 of 28 | Completion mastectomy | NA | 10 |
| 5 | 44 | NA | Paget’s | HG | 20 | SLNB | Negative | None | NA | 7 |
| 6 | 57 | <1 | IDC | 2 | 15 | SLNB | Negative | None | Infected seroma | 5 |
| 7 | 48 | 1 | IDC | 3 | 35 | ANC | 1 of 15 | None | NA | 5 |
| Case no: . | Age . | Pre-op distance of cancer from NAC (mm) . | Type of cancer . | Grade of Invasive/ In-situ cancer . | Whole tumour size (mm) . | Axillary surgery . | Nodal status . | Further surgery . | Complications . | Follow-up in months . |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 63 | 3 | IMC | 2 | 39 | SLNB | Negative | Re-excision of inferior margin | Organized small haematoma on USS at 9 months | 12 |
| 2 | 74 | 4 | IDC | 3 | 28 | SLNB | Negative | None | NA | 11 |
| 3 | 58 | <1 | IDC | 2 | 25 | SLNB | Negative | None | Partial skin necrosis | 10 |
| 4 | 66 | 6 | IDC | 2 | 50 | ANC | 1 of 28 | Completion mastectomy | NA | 10 |
| 5 | 44 | NA | Paget’s | HG | 20 | SLNB | Negative | None | NA | 7 |
| 6 | 57 | <1 | IDC | 2 | 15 | SLNB | Negative | None | Infected seroma | 5 |
| 7 | 48 | 1 | IDC | 3 | 35 | ANC | 1 of 15 | None | NA | 5 |
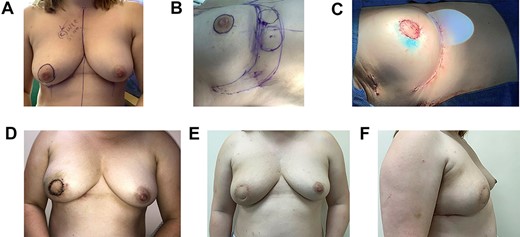
Images showing preoperative marking (A and B), the postoperative outcome on-table (C), at 2 weeks (D) and 6 months after radiotherapy (E and F) in a patient with Paget’s disease of the nipple.
Amongst our series, Patient 6 developed infected seroma which was initially treated with recurrent aspiration and antibiotics. However, she was found to have a loculated collection on ultrasound and failed to respond. She underwent wound washout and drain insertion 6 weeks postoperatively and this resulted in complete resolution of her symptoms. Patient 3 was taken back to theatre for wound debridement and primary closure of partial necrosis of the central skin island. The flap was found to be well perfused without any venous congestion. Radiotherapy was administered within the therapeutic window in both these cases.
We were able to avoid mastectomy in all except one patient (Patient 4) who was found to have multifocal invasive ductal cancer with extensive ductal carcinoma in situ (DCIS). There were no delayed surgical complications in our series during ongoing prospective follow-up.
DISCUSSION
Patient selection and operative planning are of paramount importance as with any oncoplastic procedures. We have carefully selected our patients and describe in detail below the criteria that was used and refined during our learning curve.
Ideal candidate
Women with no ptosis or grade 1 ptosis of the breast
Nipple to infra-mammary fold (IMF) distance should be ≤10 cm
Mobile and lax soft tissue below the IMF
Soft tissue pinch thickness of ≥4 cm below IMF along the breast meridian
Preoperative confirmation of the presence of chest wall perforators
Surgical technique
Pre-operatively the breast meridian, IMF and lateral mammary folds are marked with the patient in standing position and arms by the side. The natural fold of lax soft tissue below the IMF is identified and marked in standing position. This allows the surgeon to determine the width of the flap. The marking of the chest wall perforator is performed in supine position with the arm abducted to 90°. The lateral and medial intercostal perforator arteries are identified using hand-held Doppler machine. The distance between the pivot point of the flap (site of perforator) to the nipple is measured and the length of the flap is kept at least 4 to 5 cm more than this. Depending on the distance between the perforator to the nipple, a decision is made regarding the perforator to be used to provide adequate projection and symmetry.
The central wide local excision is performed through a circum-areolar incision. The perforator flap is then raised through a crescent incision along the inframammary fold [3]. Once the flap is raised, assessment should be made to ensure that the flap can be trans positioned into the cavity without tension. This is usually facilitated by splitting the breast tissue along the path of shortest distance and resistance from the IMF. Depending on the flap length, flap can be based on two consecutive intercostal perforators to perfuse effectively, though this may restrict the mobility of the flap.
The required projection and central fullness can be achieved by folding the distal end of the flap. The patients are then sat up at 40–50° to ensure that flap can be positioned appropriately to achieve the necessary aesthetic outcome. The skin paddle for creating nipple areola complex is marked and ideally placed 4–5 cm away from the distal edge of the flap to allow folding of the distal part to improve central projection. Subsequently, de-epithelization of the remaining skin over the flap is performed and leaving this step to the end also helps to assess for flap vascularity.
The folded flap is then secured in position within the central cavity using 2/0 Vicryl™. Subsequently, the donor site is closed ensuring that IMF has been recreated without any tension along the suture line. Closure of the donor site will also give the surgeon a better understanding of the insetting of the flap within the central cavity. Finally, with the patient in supine position, the central skin paddle is sutured using 3/0 Monocryl™ in two layers.
It is not a routine practice to place drains and none of the patient in our series had drains postoperatively. All our patients were cared for in a day-case ward and went home the same evening with simple analgesics. Patients were followed up postoperatively on Days 7 and 14 and then 6 months after the completion of radiotherapy (Fig. 1E and F). We have demonstrated that using CWPF to reconstruct the central mound of breast tissue after wide local excision is an oncologically safe surgical method. Moreover, the surgical outcomes demonstrated that we were able to achieve aesthetically acceptable central breast projection and avoided contralateral symmetrizing surgery in all our patients.
CONCLUSION
We describe here a robust application of CWPF to partially reconstruct the central mound of breast tissue by maintaining the aesthetic projection and use of the skin paddle for future nipple reconstruction and areolar tattooing.
CONFLICT OF INTEREST STATEMENT
None declared.



