-
PDF
- Split View
-
Views
-
Cite
Cite
Kensuke Suzuki, Yasuhito Shimizu, Mihono Hirota, Masafumi Fujino, Daigo Nobumoto, Hitoshi Kubosawa, Kenji Oda, Masayuki Ohtsuka, Duplicate appendix complicated by low-grade appendiceal mucinous neoplasm: a rare case report and review of the literature, Journal of Surgical Case Reports, Volume 2022, Issue 6, June 2022, rjac267, https://doi.org/10.1093/jscr/rjac267
Close - Share Icon Share
Abstract
Low-grade appendiceal mucinous neoplasms (LAMNs) have been a very controversial tumor, and there is a lack of standardization for the optimal surgical procedure due to the infrequency of this disease. This is the first case report of duplicate appendix complicated by LAMN. The preoperative imaging examinations revealed that the mucinous tumor was shrinking spontaneously, allowing for safe laparoscopic resection. The histopathological findings indicated a dilated common base of the duplicated appendix, suggesting that the mucinous content drained spontaneously to the cecum. Further studies of the various complications of LAMNs are needed to establish the optimal surgical approach for LAMNs.
INTRODUCTION
Low-grade appendiceal mucinous neoplasms (LAMNs) are characterized by low-grade cytologic atypia and the absence of destructive invasion. They are among the rarest appendiceal tumors with an incidence of ~0.7–1.7% [1]. The appropriate surgical approach, adjuvant therapy and follow-up duration for the optimal management of LAMNs are still controversial. Appendiceal duplication is also exceedingly rare with an incidence of 0.004–0.009% in appendectomy specimens [2] [3]. In the present study, we report the first case of LAMN on the duplicate appendix.
CASE REPORT
A 74-year-old female with hypertension, hyperlipidemia and hyperuricemia had a colonoscopy as a screening examination. The colonoscopy revealed an extrinsic compression with ulceration located at the cecum (Fig. 1). A multidetector computed tomography (CT) identified a low-attenuation distorted cystic lesion with focal calcification in the anatomic region of the right iliac fossa, measuring 6.1 × 5.0 × 3.7 cm (Fig. 2). Findings from the routine laboratory examinations were unremarkable, and all tumor markers were within normal range. The patient was scheduled for ileocecal resection with lymph node dissection due to the possibility of malignancy, such as appendiceal mucinous adenocarcinoma, because of the large and distorted tumor. Contrast-enhanced CT was conducted for further assessment of the findings, and we found that the cystic lesion was dramatically shrinking. It seemed improbable that rupture of the tumor had happened since no findings implied the spread of mucinous components, such as ascites or mucinous peritoneal nodules on CT. It was considered that the mucinous content was spontaneously drained from the root of the appendix to the cecum. However, the enhanced and distorted lesion with focal calcification, suggesting malignancy, had remained in concordance with the base of appendix (2.7 × 2.1 × 1.9 cm) (Fig. 3). Therefore, ileocecal resection was performed as planned, and laparoscopic procedure was selected due to the unlikelihood of the tumor rupturing. The base of appendix was distended and there were no obvious peritoneal anomalies upon visualization of the abdomen (Fig. 4). The specimen was handled with care and there was no spillage of cystic contents. The post-operative course was uneventful, and the patient was discharged on post-operative day 8.
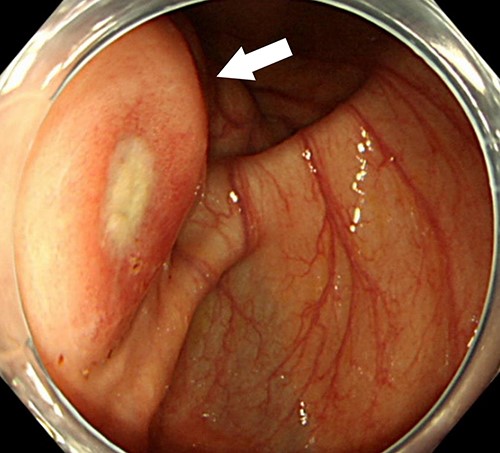
Colonoscopy examination showing an extrinsic compression with ulceration located at the cecum (arrow).

Abdominal CT showing a cystic lesion with some calcification in the right iliac fossa (arrow).

Contrast-enhanced CT showing the enhanced and distorted lesion with focal calcification (arrow).
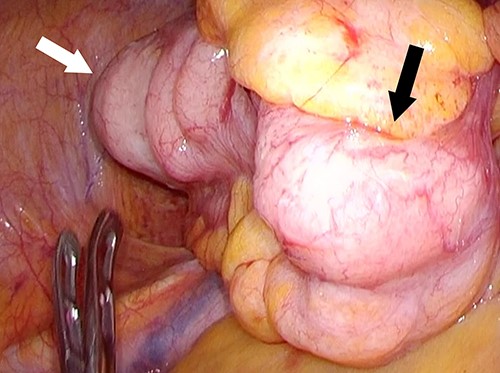
Screen capture of the appendiceal tumor during the surgical laparoscopic procedure (white arrow: cecum, black arrow: distended appendix).
Macroscopic examination of the specimen disclosed the presence of a duplicated appendix, which had partial duplication with both appendices sharing a common dilated base, like ‘Y-shaped’, measuring 1.5 cm on a single caecum (Fig. 5). Microscopic examination showed replacement of the normal appendiceal epithelium by mucin-producing columnar glandular epithelium with low-grade dysplasia from the common base to both duplicated appendices (Fig. 6). There were no histological findings of conventional, high-grade mucinous appendiceal adenocarcinoma, such as the proliferation of mucinous epithelial cells with high-grade dysplasia, architectural complexity, cribriform pattern or glands infiltrating in a desmoplastic stroma. The pathological diagnosis was a LAMN with pTis (LAMN) pN0 stage 0, using pTNM, Eighth Edition of AJCC, with free surgical margins and on the duplicate appendix. A follow-up CT was performed 6 months after the surgery, reporting no evidence of distant metastasis or pseudomyxoma peritonei (PMP) which is the clinical term for the spread of LAMN to the peritoneal cavity.
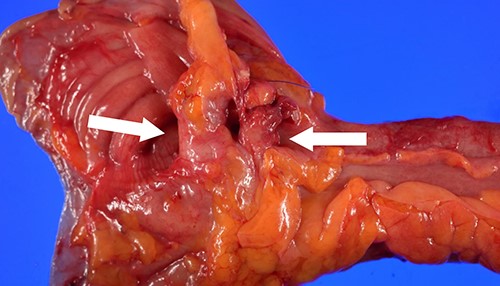
Gross examination of the surgical specimen showing the presence of a partial duplicated appendix, both appendices (white arrows) sharing a 1.5-cm dilated base in a ‘Y-shaped’ pattern on a single caecum.
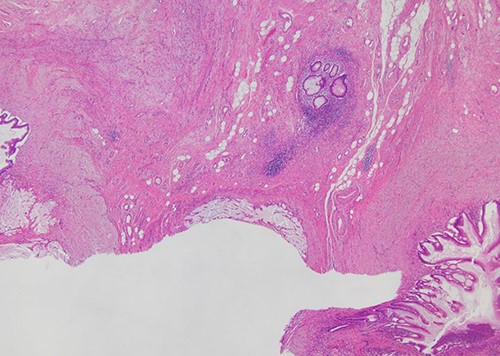
Histopathological examination (H&E stain; ×40 magnification) showing that mucin-producing columnar glandular epithelium with low-grade dysplasia replaced the normal appendiceal epithelium from the common base to both of duplicated appendices.
DISCUSSION
LAMNs are rare noninvasive epithelial tumors of the appendix. In 2016, a consensus regarding the classification of PMP and associated appendiceal neoplasia replaced the term ‘mucinous cystadenomas’ with the new term ‘low-grade appendiceal mucinous neoplasm—LAMN’ [4]. These tumors possess the potential for peritoneal spread and can eventually lead to death even in the absence of overtly malignant cytologic features. The common abdominal CT findings include cystic dilation within the appendiceal lumen with wall calcifications and irregular appendiceal wall thickening as demonstrated in our case.
Controversy remains on the best surgical approach for the optimal management of LAMNs. Recently, the practice of ileocecal resection has been replaced with appendectomy, which is the only approach used for the treatment of benign appendiceal mucoceles [5]. Although cecectomy without lymph node dissection has also been proposed to accomplish a surgery with a free surgical margin for LAMNs [6], additional ileocecal resection may be required for the dissection of potential lymph node metastases if the infiltration of malignancy into submucosa are detected on histological examination of the resected specimen. LAMN >6 cm, such as our case, has been reported to present with a higher risk of malignant cells, a higher risk of appendiceal perforation and development of PMP [7]. Therefore, we selected ileocecal resection with the patient’s consent to avoid any remaining malignant tumor cells left behind from the first surgery.
A multicenter study demonstrated the safety of laparoscopic surgery for appendiceal mucocele [8]. However, the feasibility of this procedure for giant tumors, which has potential malignancy, is still controversial [9]. Fortunately, the cystic tumor shrank in the present case, and a laparoscopic procedure could be performed without any complications. The shrinking tumor is rarely observed in LAMNs patients, but our case was a partially duplicated appendix with a common dilated base, which can allow for the spontaneous draining of mucinous content to the cecum. Indeed, histological examination revealed the dilated base of appendix (1.5 cm) to be larger than the normal base (0.8 cm) [10].
Appendiceal duplication is an exceedingly rare congenital anomaly, the incidence of which has been reported to be as low as 0.004% in appendectomy specimens [2] [3]. These anomalies are classified into Types A–D [11]. Our case falls under Type A, which has a single cecum with various degrees of incomplete appendiceal duplication. The frequency of neoplasm in enteric duplication is still unknown, but it has been rarely reported and appears limited to only a small number of cases [12, 13]. Appendiceal cancer also has been associated with few prior reports of a duplicated appendix [14, 15]. Furthermore, to our knowledge, our case is the first report of duplicated appendix complicated by LAMNs.
In the present study, we describe an extremely rare case of LAMN complicated by a duplicated appendix, which is also a rare congenital anomaly. The optimal surgical approach of LAMNs requires further studies with various cases, including congenital anomalies as in our case.
AUTHORS’ CONTRIBUTIONS
K.S., Y.S. and M.H. performed the operation. K.S. conceived and designed the study and wrote the original draft of the manuscript. M.F., D.N., K.O. and M.O. reviewed and edited the manuscript. H.K. performed the histological analysis. All authors read and approved the final version of the manuscript.
ACKNOWLEDGEMENTS
We thank the patient for allowing the disclosure of her medical report and intraoperative photographic records.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
CONSENT
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review from the editor-in-chief of this journal on request.



