-
PDF
- Split View
-
Views
-
Cite
Cite
Samir El Youbi, Salma Boulman, Hamza Naouli, Hamid Jiber, Abdellatif Bouarhroum, Surgical management of a congenital arteriovenous fistula of the forearm, Journal of Surgical Case Reports, Volume 2022, Issue 6, June 2022, rjac259, https://doi.org/10.1093/jscr/rjac259
Close - Share Icon Share
Abstract
Congenital arteriovenous fistula (AVF) is a rare vascular disease, which may occur anywhere in the body. The forearm is a very rare location. Clinical manifestations are not very specific and can vary from an asymptomatic fistula to a life-threatening congestive heart failure. Although embolization can be an alternative treatment for AVF of the forearm, surgery is still considered as the standard treatment. Herein, we report the case of a 7-year-old boy with a congenital AVF between the radial artery and the superficial cephalic vein in the forearm without any dysmorphic features treated surgically.
INTRODUCTION
Arteriovenous fistula (AVF) is an abnormal communication between an artery and a vein that might be congenital or acquired [1] and may occur anywhere in the body [2]. Although AVFs occur most commonly in the legs or arms, congenital fistulas between the radial artery and the cephalic vein of the forearm in children are very rare and have never been reported in the literature. We report the case of a 7-year-old boy with an AVF between the radial artery and the superficial cephalic vein in the forearm without any notion of trauma.
CASE PRESENTATION
A 7-year-old boy, without any pathological history, was admitted to our department for the management of an arteriovenous fistula of the right forearm evolving since birth, with a progressive dilatation of the cephalic vein of the forearm over the years. The lesion was incidentally discovered by his parents.
On physical examination, the patient appeared healthy without any dysmorphic features. Examination of the right arm revealed a thrill on palpation along the course of the right cephalic vein of the forearm and its collateral branches without any inflammatory signs. The radial and ulnar pulses were present bilaterally and symmetrically. Routine blood tests were normal.
Duplex ultrasonography revealed an arteriovenous fistula in the distal third of the forearm between the radial artery and the cephalic vein of the forearm. The radial artery was dilated measuring 3.9 mm, flowing with an average velocity measured at 48 cm/s, and a flow rate at 340 ml/min (high flow rate for a normal radial artery). The antebrachial cephalic vein is dilated and gives numerous collaterals that are also dilated.
A curative surgical treatment was proposed and accepted by the child’s family and was undertaken by a vascular surgeon. A longitudinal incision was made directly over the AVF. After the dissection and the identification of the AVF to its origin on the radial artery (Fig. 1), we proceeded to tie off the AVF and the radial artery was preserved and repaired with 7-0 Prolene sutures (Fig. 2). The postoperative outcomes were uneventful. The result at 3 years was satisfactory and stable.
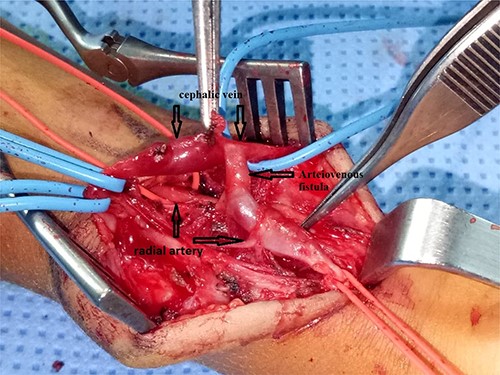
Surgical exploration showing an arteriovenous fistula between the radial artery and the cephalic vein of the forearm.
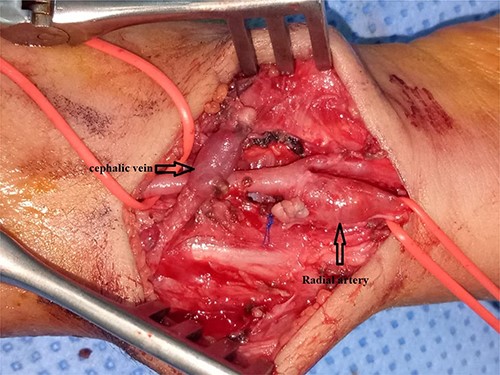
Ligation of the arteriovenous fistula and the radial artery was preserved and repaired with 7-0 Prolene sutures.
DISCUSSION
Arteriovenous fistulas are a rare vascular disease and, among the different types, the most common is that of post-traumatic origin [1]. Congenital arteriovenous fistula can occur anywhere in the body but the most frequent anatomical sites are located in the femoro-popliteal and subclavian sectors [3, 4]. Congenital arteriovenous fistulas are very rare entities and few cases are reported in the literature.
AVF may be sporadic and are observed in patients with hereditary hemorrhagic telangiectasia [5] or in Capillary Malformation-Arteriovenous Malformation Syndrome (CM-AVM) RASA1-related disease (RAS p21 protein activator [GTPase activating protein]) [6].
Diagnosis and treatment algorithms of the congenital arteriovenous fistula of radial artery cannot be found in any published literature due to its rarity.
Clinical manifestations vary from none to life-threatening congestive heart failure, the common clinical manifestations of AVFs of the trunk and extremities are a thrill, dilatation of draining vein, pain, ulceration, tissue necrosis and venous hypertension and/or cardiac failure.
In the case presented, the advantages of Duplex ultrasonography should be reiterated [7, 8]: the tests is non-invasive and do not require irradiation nor injection of contrast material; the location and direction of blood flow can be easily traced and identified for measurement; is the best tool to assess the adequacy of tissue perfusion for perioperative assessment and provide information for evidence-based decision-making about whether to ligate or reconstruct the radial artery.
Cardiac examination (echocardiography) may be necessary when there is an AVF: with direct arterial flow into the venous system and bypass of the capillary beds, the volume of diverted blood flow is high and heart failure may occur due to an increase in the volume of blood returning to the heart.
Magnetic resonance imaging (MRI), computed tomography angiography (CTA) and direct angiography have been established for the diagnosis of arteriovenous fistula, but each modality has its own advantages and disadvantages. Although they produce stationary images, they can provide a general mapping of the arteries and aid in planning surgery, particularly in selective angiography of the radial and ulnar arteries. In addition, they can be used as a therapeutic option in the form of favorable lesion embolization. Rather, the choice of which modality to use should be based on its availability, experience and the possibility of endovascular intervention [9, 10].
Untreated AVF often leads to overload of venous drainage or distal limb ischemia. However, in the situation of limited venous drainage, such as small vein size, as presented in this case, high AVF pressure could lead to local vascular dilation and lead to vessel angulation or formation of aneurysms [7]. In such conditions, the development of thromboembolic complications with subsequent ischemia of the finger and hand can occur. Therefore, unless AVF is needed for a specific purpose, vascular resection and reconstruction should be performed for best long-term results [7, 9]. Surgery is the standard treatment for AVFs of the forearm, embolization can be proposed.
Sacrificing the radial artery during AVF resection is feasible and fairly easy, but even with careful perioperative confirmation of collateral circulation, the potential for short- or long-term insufficient tissue perfusion remains [8]. Therefore, vascular preservation was a must and the first therapy of choice, in our young patient.
CONCLUSION
The forearm is a very rare location of congenital arteriovenous fistulas. Clinical manifestations vary from none to life-threatening congestive heart failure. The AVF is cured by a well-conducted surgical treatment or by embolization and the objective of treatment is to preferentially occlude these fistulas leaving the peripheral hypervascularization without shunt.
DATA AVAILABILITY
All data generated or analyzed during this study are included in this published article.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no competing interests.
FUNDING
The authors received no specific funding for this study.



