-
PDF
- Split View
-
Views
-
Cite
Cite
Daniel J Arenas, Paul T Hernandez, Jasmine Hwang, Divyansh Agarwal, Alexander K Warshauer, Daniel N Holena, A low appendiceal mucinous neoplasm lesion in an inflamed appendix within an inguinal hernia, Journal of Surgical Case Reports, Volume 2022, Issue 6, June 2022, rjab489, https://doi.org/10.1093/jscr/rjab489
Close - Share Icon Share
Abstract
Amyand’s hernia, an incarcerated appendix inside an inguinal hernia, accounts for <1% of hernias in children and even less in adults. Similarly, low-grade appendiceal mucinous (LAMN) lesions are only found in <1% of removed appendices. We present the case of a 72-year-old man with a 15-year history of a large right inguinoscrotal hernia that presented with right lower quadrant pain, was found by computed tomography imaging to have an incarcerated appendix with a large fluid collection, and was post-operatively diagnosed with an LAMN lesion. Although our case is rare due to the simultaneity of the Amyand’s hernia and LAMN conditions, each separate condition is prevalent enough for most surgical providers to encounter at least one of these. For our case, we discuss the decisions made in the pre-operative and post-operative management and relevant literature.
INTRODUCTION
Although Amyand’s hernias, an incarcerated appendix inside an inguinal hernia, and appendiceal neoplasms are relatively rare conditions in adults, the high numbers of appendicitis cases at every major hospital increase the chances that providers will encounter each condition at some point [1]. For Amyand’s hernias, the prevalence is ~0.8% of all appendicitis cases in children and ~0.2% in adults (see Supplementary Fig. S1 in supplementary document). Similarly, appendiceal neoplasms are found in ~1% of all appendectomies [2].
CASE REPORT
A 72-year-old man with a 15-year history of a large, right inguinoscrotal hernia was transferred from an outside hospital with right lower quadrant pain that migrated to the scrotum after several hours. His pain was associated with nausea and non-bilious vomiting, though he continued to have bowel movements and pass flatus.
Physical examination revealed a soft, non-tender abdomen and a large, soft, non-tender right inguinal hernia extending into the right hemiscrotum. Lab work demonstrated mild leukocytosis (12 500/μl). Computed tomography (CT) of the abdomen and pelvis showed a large indirect inguinal hernia, containing a large amount of simple fluid as well as the cecum and a non-perforated appendix. There were no signs of bowel incarceration. Notably, the appendix was dilated to 2.9 cm (Fig. 1).
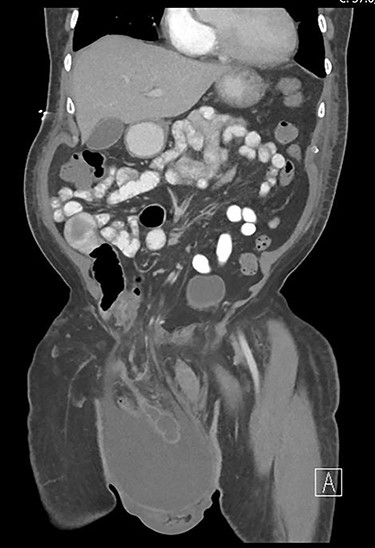
Coronal view of the pre-operative abdominal CT. The appendix was incarcerated inside the inguinal hernia and surrounded by a large amount of simple fluid.
The patient had a high level of medical knowledge and understanding, but he had been hesitant to undergo treatment for his hernia due to having witnessed surgery complications in a loved one. After meeting with the medical team, the patient agreed to undergo elective hernia repair the day after admission. The hernia was dissected free from the spermatic cord and the sac entered, draining approximately one liter of serous fluid. The appendix was mildly inflamed measuring 13 cm in length with a 3-cm mass involving the tip. The mesoappendix was ligated, and the appendix was resected at its base (Supplementary Fig. S2 of supplementary document). A tension-free hernia repair was then performed with an aphasic mesh. Pathology identified a low-grade appendiceal mucinous neoplasm (LAMN) with negative margins, without extension to the serosa, as well as three lymph nodes negative for tumor. The patient was referred to an oncologist. Two months after the operation, his CA19-9 and CA-125 serum levels were within normal limits, and his carcinoembryonic antigen (CEA) level was 0.3 mg/dl above the upper limit of normal (4.7 mg/dl). Magnetic resonance imaging (MRI) 2 and 5 months after the patient’s surgery suggested no signs of pseudomyxoma peritonei or recurring disease. The patient continues to be under active surveillance.
DISCUSSION
Pre-operatively, our patient’s CT imaging (Fig. 1) proved useful in identifying the Amyand’s hernia and in planning an appendectomy simultaneous with hernia repair. Although, a large proportion of Amyand’s hernias are found during appendectomy, pre-operative diagnoses have been previously reported [3, 4]. In addition to the incarcerated appendix, the large fluid collection in his remarkable abdominal CT imaging was concerning for an inflammatory process. The inflammation was relevant to the categorization and potential management of the Amyand’s hernia [5], as signs of appendicitis would escalate an Amyand’s hernia to a Type 2. This type unsurprisingly carries a higher risk of infection and therefore advices caution when considering a repair with a mesh [5]. However, for our patient, since the size of the hernia was worrisome for promptly recurrence, we decided on the use of an acellular mesh to decrease the risk of recurrence while minimizing the risk of infection.
Further relevant to Amyand’s categorization, the CT imaging and physical examination showed no signs of perforation, peritonitis, or other abnormal pathology; therefore, the Amyand’s hernia was not pre-operatively escalated to either a Type 3 or Type 4. However, as there was no available recent CT imaging, it was considered that the fluid collection and potential inflammation may have been masking another pathology process [4].
Operatively, as the mesoappendix was ligated and the appendix isolated, it was important to check for signs of perforation of abscesses that could have been masked by the large fluid collection [6]. Although no perforation or abscesses were found, the inflamed erythematous lesions in the appendix (Supplementary Fig. S2 of supplementary document), immediately raised concerns for a potential neoplastic lesion. This concern added further importance that mucinous deposits were ruled out as they could later escalate the diagnosis to a seeding neoplasm.
LAMN lesions comprise ~10% of noncarcinoid appendiceal neoplasms and their classification and management is a continuously evolving field [7]. In the case of our patient, if was reassuring that there had been no appendix perforation as this finding is associated with a higher risk of future pseudomyxoma peritonei [8]. Therefore, LAMN and high-grade mucinous neoplasms (HAMN) with perforation, or mucinous metastasis, are usually managed with cytoreduction, prophylactic chemotherapy and potential right hemicolectomy [8]. However, the management of LAMN/HAMN lesions without perforations or mucinous metastasis, as in our patient, do not have a clear management directive [8]. Recent cohort data suggest that observation is sufficient since the data suggest a lower risk of recurrence for patients with negative margins, without perforation and with normal levels of tumor markers [7]. Other studies also suggest an excellent prognosis in similar conditions [9–11]. For our patient, the literature therefore suggests a good prognosis probability since his CA-125, CA19-9 were normal, and his CEA was elevated but not far from the upper limit of normal. Although, his 5-month negative follow-up MRI was comforting, the patient remains in observation as the risk beyond 5 years requires more research [10].
Although our patient’s case is highly rare due to the simultaneity of Amyand’s hernia and an LAMN lesion, his management (before, during and after the surgery) required understanding of the two conditions. It is our hope that our case report is useful to providers that will likely deal with at least one of these conditions. Lastly, we hope this case report adds to the motivation to perform more cohort studies that investigate the management of LAMN lesions without signs of perforation or mucinous metastasis.
ACKNOWLEDGEMENTS
The authors would like to thank our patient for his willingness in sharing his case and for his continued communication. DJA would like to thank Walter and Anne Gamble for continued support.



