-
PDF
- Split View
-
Views
-
Cite
Cite
Takuya Ohashi, Mitsumasa Kawago, Fuminori Ota, Yoshimitsu Hirai, Megumi Kiyoi, Miwako Miyasaka, Yumi Yata, Mari Kawaji, Aya Fusamoto, Hideto Iguchi, Hitomi Nakanishi, Takahito Nakaya, Yuki Fujiwara, Yoshiharu Nishimura, Combination treatment by the cervical approach with mediastinal drainage and continuous saline irrigation for descending necrotizing mediastinitis type IIb: a three-case series, Journal of Surgical Case Reports, Volume 2022, Issue 5, May 2022, rjac237, https://doi.org/10.1093/jscr/rjac237
Close - Share Icon Share
Abstract
Descending necrotizing mediastinitis (DNM) is a severe, life-threatening disease and requires prompt treatment. The primary treatment for DNM is cervical and mediastinal drainage in addition to antibiotic treatment. However, the most appropriate drainage approach and the effectiveness of additional treatment remain unclear. In this study, we performed cervical and mediastinal drainage for three patients with type IIB DNM using the cervical approach alone. Continuous saline irrigation was administered as additional treatment. There is little evidence for the use of saline irrigation for DNM. We propose that this combination treatment may be more effective and has the potential to improve patient prognosis. In our report, the average drainage duration was 13 days, and the average hospital stay was 30 days. Furthermore, both drainage duration and hospital stay were shorter than those in previously reported cases. Our case series provides valuable insight into the use of combination treatment to treat DNM.
INTRODUCTION
Descending necrotizing mediastinitis (DNM) occurs when an infection spreads over a wide area of the cervical and mediastinal spaces [1]. Rapid and appropriate drainage is important for treating DNM; various drainage methods have been reported in the literature [2–4], and it is unclear which methods are more effective. In this report, we present three cases of patients with DNM who were successfully treated using combination treatment with a cervical approach with mediastinal drainage and continuous saline irrigation.
CASE SERIES
Case 1
A 77-year-old woman had a chief complaint of sore throat and was diagnosed with a retropharyngeal abscess. Cervicothoracic computed tomography (CT) showed that the infection had spread to the mediastinum (Fig. 1A). The patient was diagnosed with type IIB DNM. Cervical drainage and mediastinal drainage through the cervical approach were performed on the day of admission. Staphylococcus epidermidis, Streptococcus mitis and Acinetobacter lwoffii were detected in the mediastinal abscess cavity. The patient was administered ampicillin/sulbactam at 12 g/day for 3 weeks. Continuous irrigation with saline (2 l/day) was initiated immediately post-surgery. The duration of irrigation, drainage and hospital stay were 4, 10 and 30 days, respectively. Four weeks post-surgery, cervicothoracic CT showed no abscess cavity and the infection had improved (Fig. 1B).
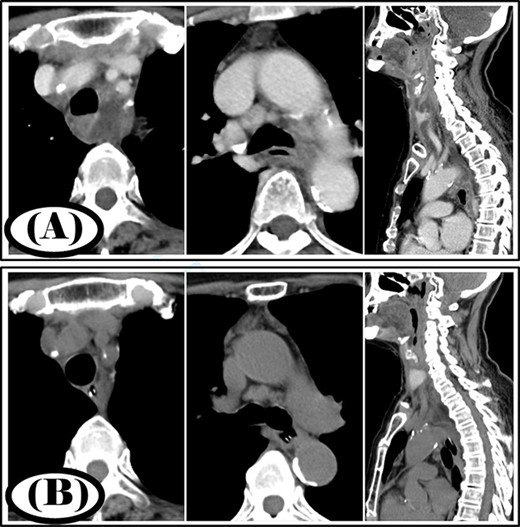
Case 1: pre- and post-treatment cervicothoracic CT; (A) pre-operative cervicothoracic CT and (B) cervicothoracic CT 4 weeks after treatment.
Case 2
A 35-year-old man was diagnosed with a cervical abscess and initially underwent cervical drainage. The next day, he developed upper gastrointestinal perforation that was covered with an omental patch in a laparoscopic procedure. The cervical abscess did not improve and chest CT revealed that the infection had developed into the mediastinum (Fig. 2A). The patient was diagnosed with type II DNM and underwent mediastinal drainage using a cervical approach 3 days later. Initial antibiotic therapy consisted of meropenem at 9 g/day for 6 days as broad-spectrum antibiotic therapy. After Streptococcus anginosus group was detected in the mediastinal abscess cavity, the antibiotic was changed to ampicillin/sulbactam 12 g/day and was administered via intravenous infusion for 15 days. Continuous irrigation with saline (2 L/day) was initiated immediately post-surgery; however, 500 ml per day of saline was used for irrigation on the first 4 days. The duration of irrigation, drainage and hospital stay were 4, 16 and 39 days, respectively. Five weeks post-surgery, cervicothoracic CT showed no abscess cavity and an improvement in infection (Fig. 2B).
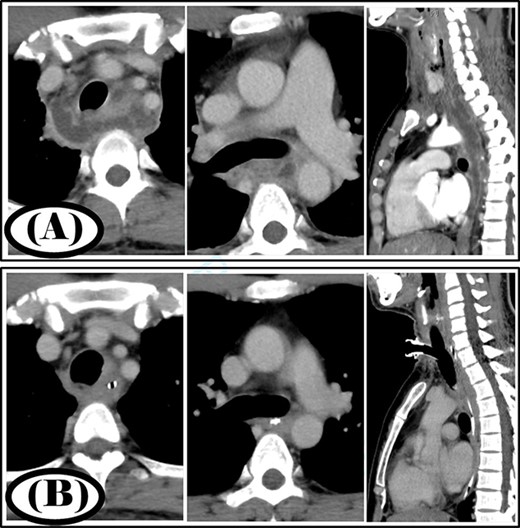
Case 2: pre- and post-treatment cervicothoracic CT; (A) pre-operative cervicothoracic CT and (B) cervicothoracic CT 5 weeks after treatment.
Case 3
A 68-year-old woman was diagnosed with a posterior pharyngeal abscess triggered by a fever and sore throat. Cervicothoracic CT showed that the infection had spread to the mediastinum (Fig. 3A), and the patient was diagnosed with type IIB DNM. Cervical drainage and mediastinal drainage were performed simultaneously. Mediastinal drainage using only the cervical approach was sufficient. Streptococcus sanguinis was detected in the mediastinal abscess cavity. Continuous irrigation with saline (2 l/day) was initiated immediately post-surgery. The duration of irrigation, drainage and hospital stay were 10, 13 and 22 days, respectively. Four weeks post-surgery, cervicothoracic CT showed no abscess cavity and an improvement in infection was noted (Fig. 3B).
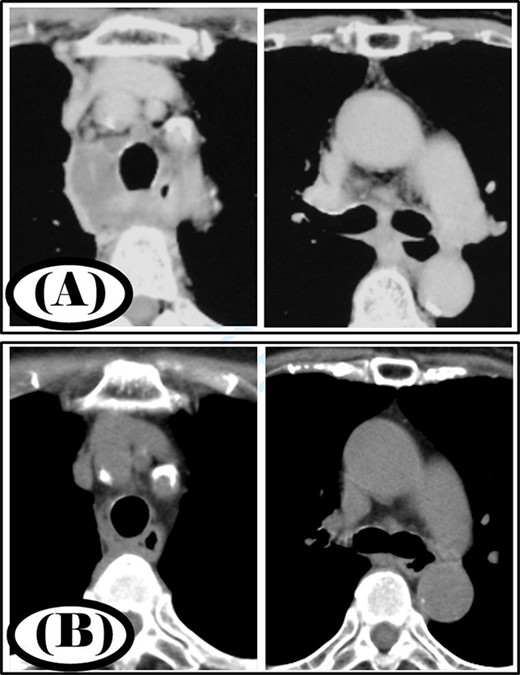
Case 3: pre- and post-treatment cervicothoracic CT; (A) pre-operative cervicothoracic CT and (B) cervicothoracic CT 4 weeks after treatment.
DISCUSSION
DNM is triggered by a deep cervical or odontogenic infection, which can spread to the mediastinum through the blood vessels and muscle space [5]. It is associated with a high mortality rate and requires prompt treatment, particularly with antibiotics and drainage of the cervical and mediastinal spaces. Endo et al. [2] classified DNM into three types. The localized type (type I) is confined to the superior mediastinum cephalad to the tracheal bifurcation, whereas the extensive type extends to the caudal mediastinum. Extensive-type DNM can be further classified into the anterior mediastinal type (type IIA) which is mainly anterior mediastinal, and the posterior mediastinal type (type IIB), which extends through the esophageal interstitium to the inferior mediastinum. Palma et al. [3] reported that type IIB DNM was more severe than the others, with an average length of hospital stay (intensive care unit) of 3.2 days or longer.
The most common drainage methods for DNM are cervical drainage and additional mediastinal drainage. Cervical drainage alone is associated with a mortality rate of 47%, but this was reduced to 19% when combined with mediastinal drainage [4]. However, there are various approaches to mediastinal drainage, including posterolateral incision, sternotomy, glenoid incision and clamshell incision. Furthermore, there are differences in the techniques, such as open surgery or thoracoscopic surgery, and the use of a mediastinoscope. Other approaches to mediastinal drainage, except for the cervical approach, are drainage methods which disrupt anatomical membrane structures such as the parietal pleura. Endo et al. [2] stated that type I DNM requires a cervical approach, type IIA requires a subxiphoid approach in addition to a cervical approach and type IIB requires a transthoracic approach in addition to a cervical approach for adequate mediastinal drainage surgery. However, Hsu et al. [6] reported that there was no difference in the length of hospital stay and mortality rate between mediastinal drainage through the cervical approach alone or through combined cervical and thoracic approaches. Although mediastinal drainage is essential, a standardized approach has not yet been established.
There are a few reports on continuous irrigation with saline for DNM. Oshima et al. [7] reported that the mediastinum and thoracic cavity were irrigated with 2 l of saline daily, and the patient was discharged 80 days post-operatively. Okamoto et al. [8] reported mediastinal and thoracic irrigation with 5 l of saline. In a report of 10 patients who underwent continuous irrigation with 1000–2000 ml of saline, the authors reported a good clinical course with an average drainage duration of 26.7 days and an average length of hospital stay of 62.3 days [9]. The amount of saline used has not been consistent across studies, but all studies suggest the effectiveness of continuous irrigation.
In our study, we encountered three cases of type IIB DNM that were managed by mediastinal drainage through a combination of the cervical approach and continuous saline irrigation. Although the patients had type IIB DNM, mediastinal drainage could be adequately performed using the cervical approach alone. Preserving anatomical membrane structures such as the parietal pleura may have allowed the mediastinum to be cleaned efficiently. This report presents a three-patient case series, and many more cases should be considered in the future. The combination of mediastinal drainage using the cervical approach and continuous saline irrigation did not result in death, and both the drainage duration and hospitalization duration were favorable. Results from this case series are meaningful because continuous saline irrigation should be actively considered for type IIB DNM.
AUTHORS’ CONTRIBUTIONS
T.O. and M.K. were involved in study design and wrote the manuscript as equal first authors. Y.H., M.K., M.M., Y.Y., M.K., A.F., H.I., H.N. and Y.N. assisted in the writing of the manuscript. All authors critically revised the report, commented on drafts of the manuscript and approved the final report.
CONFLICT OF INTEREST STATEMENT
The authors have no actual or potential conflicts of interest to declare.
ETHICS APPROVAL
Patients provided written informed consent for these medical procedures as well as for the anonymized publication of clinical findings and associated images.
FUNDING
We did not receive any external funding for this work.
References
Author notes
T. Ohashi and M. Kawago are equal first authors.



