-
PDF
- Split View
-
Views
-
Cite
Cite
Thomas Kotsis, Panagitsa Christoforou, Achilles Chatziioannou, Nikolaos Memos, Kassiani Theodoraki, Manousos Konstadoulakis, Vena cava balloon occlusion for pulmonary embolism prevention during resection of giant uterus fibroids, Journal of Surgical Case Reports, Volume 2022, Issue 5, May 2022, rjac234, https://doi.org/10.1093/jscr/rjac234
Close - Share Icon Share
Abstract
We report the case of a single 46-year-old woman presenting with huge uterine fibroids growing for the last 12 years, resulting in a recent common iliac vein thrombosis. Due to the high risk for pulmonary embolism, an occluding balloon was inserted through the right jugular vein before the abdominal incision and occluded the vena cava just inferior to the renal veins. The tumor was easily mobilized, and the vena cava bifurcation was exposed and controlled until the uterus with the masses was resected. We recommend this method for oncovascular surgeries involving deep vein thrombosis and vein thromboembolism.
INTRODUCTION
A 46-year-old woman who presented with left iliac-femoral vein thrombosis provoked by mechanical compression from huge uterine fibroids. Following a multi-disciplinary preoperative evaluation, which included vascular surgeon participation, a high risk for pulmonary embolism (PE) was emphasized and vena cava filter insertion was rejected. Instead of the latter, the use of an occlusion balloon in the vena cava was suggested for temporal vena cava occlusion during the fibroid mobilization until the proximal control of the thrombosed left common iliac vein.
CASE REPORT
A single 46-year-old woman had a known history of huge uterine fibroids growing for the last 12 years. In her current presentation, the uterine with the fibroids was extending from the xiphoid to pubis, resulting in a recent common iliac vein thrombosis. The patient underwent a magnetic resonance imaging study of the abdomen, which showed enlarged uterine fibroids; the largest (21 cm in diameter) projected to the right lateral abdomen, compressing the gallbladder and the inferior vena cava (IVC).
One month later, after vascular consultation, a chest and pelvis computed tomography angiography was performed and a huge mass originating from the uterine wall was revealed (26 cm in diameter) (Fig. 1). The mass compressed the surrounding organs, especially IVC (Fig. 2). Furthermore, thrombosis of left femoral and external and common iliac veins, as well as infrarenal IVC patency (without clarification of IVC thrombosis), was detected. The common, internal and external right iliac veins were patent, and no PE was detected.
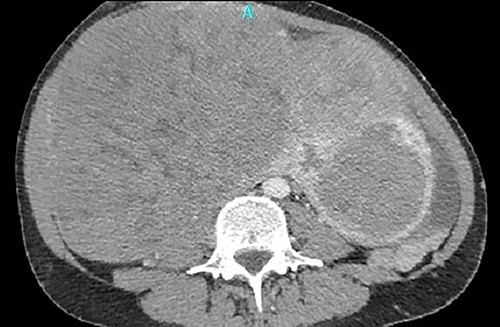
A huge mass originating from the uterine wall was revealed after pelvis CTA.

Thrombosis of left femoral and external and common iliac veins.
Under fluoroscopy, an aortic occlusion balloon catheter (Reliant AB46 Medtronic Minneapolis, SENSH 1228 W) through a 12F introducer sheath was inserted to the right internal jugular vein into the IVC and was positioned in the restricted free inferior caval space just below the renal veins (Fig. 3). Before the final placement of the balloon and the initiation of any surgical procedure, the hemodynamic condition of the patient was checked during the placement and extension of the balloon. No hemodynamic instability was observed, so the operation proceeded to the next step. The catheter balloon was inflated with the appropriate volume of physiologic saline solution to occlude the IVC and the operation began. The temporal vena cava occlusion continued until the fibroid mobilization and the proximal control of the thrombosed left common iliac vein. After mass mobilization, the vena cava was checked manually for possible clots within the vein, coming from the common iliac veins, especially from the left one. Following removal of the fibroids with the uterus, the occlusion balloon was deflated and removed without any complication. The blood pressure and heart rate were monitored continuously throughout the operation; no significant changes occurred. A total hysterectomy with bilateral adnexectomy was also conducted.
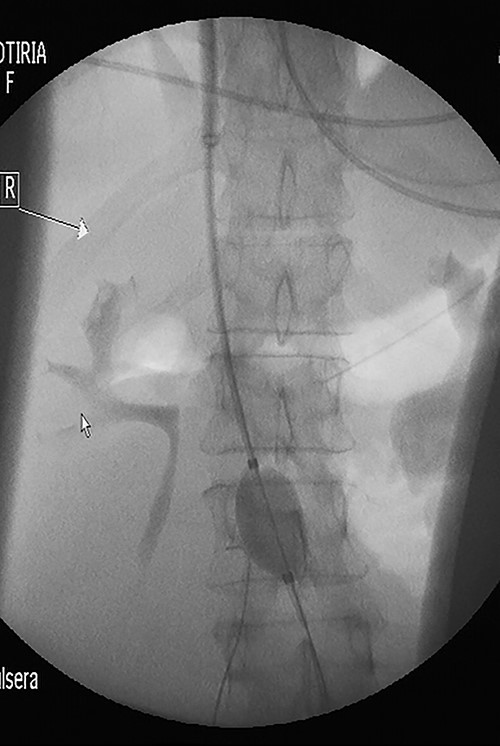
Under fluoroscopy, an aortic occlusion balloon catheter was positioned in the restricted free inferior caval space just below the renal veins.
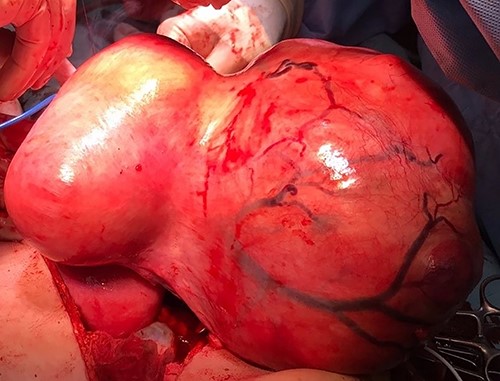
The macroscopic description reported a large compact solid mass with oblique perimeter with dimensions of 27 × 18 × 15.5 cm (Fig. 4). The microscopic examination reported a leiomyoma of uterus with vitreous degeneration, with mild to moderate lesions of cervicitis.
DISCUSSION
Uterine fibroids or myomas or leiomyomas are clonal neoplasms of the uterus [1]. Moreover, studies have also established an association between large uterine fibroids and acute venous thromboembolism, deep vein thrombosis (DVT) and PE [2].
Hysterectomy is the standard treatment, but in patients who want to preserve their fertility, myomectomy provides a conservative option together with using IVC filters and anticoagulant agents [3–5].
During the surgical removal of the uterus myoma in a patient with concurrent DVT, the primary goal is to avoid detachment of the thrombi and, thus, to decrease the risk of a PE. Some authors suggest the preoperative IVC filter placement with the aim to prevent a potentially fatal PE [6–8].
Since 1975, the balloon occlusion of the IVC had been described by Hunter et al. [9, 10]. The Bridge Occlusion Balloon described by Pecha et al. was a compliant balloon, specifically designed for temporary superior vena cava occlusion in case of laceration during lead extraction procedures [11]. Metcalfe et al. described transjugular balloon occlusion of the suprahepatic IVC for the control of the IVC during IVC thrombectomy [12]. According to Yang et al., temporary balloon occlusion of the IVC is a simple and reliable technique that decreases the risk of PE and facilitates the resection of renal tumor with IVC thrombus [13].
The choice to apply a vena cava filter was rejected because the pressure of IVC by fibroids was significant, so it would be dangerous and impossible for the wires to pass.
The decision to place an occlusion balloon in the IVC, before main surgery, was the best approach because of the extensive left iliac vein’s DVT and the high risk to mobilize thrombi during the surgical manipulation of the tumor. This is the main reason for placement of the occlusion balloon catheter into IVC to prevent clots removal from the venous iliac axis to lungs and to create a PE. After venting, the patency of the right common iliac vein and vena cava were checked, an attempt for proximal common iliac vein thrombectomy was performed using a fogarty catheter, which failed, so it was preferred to ligate and divide the left common iliac vein to avoid any future displacement of the thrombi. The main goal, in our case, was to protect the patient from PE and the target was accomplished.
CONCLUSION
We report our experience with using an occlusion balloon catheter into IVC before removal of huge uterine fibroids. The described technique showed no complications and was performed easily. We recommend this method for oncovascular surgeries, involving deep vein thrombosis and vein thromboembolism.
CONFLICT OF INTEREST STATEMENT
No conflict of interest.
FUNDING
None.



