-
PDF
- Split View
-
Views
-
Cite
Cite
Jorge H Figueras, Ramsey S Sabbagh, Cameron G Thomson, Nihar S Shah, Henry A Kuechly, Ashley Mennenga, Brian Grawe, Rotator cuff tear with scapular dyskinesis treated with a pectoralis major transfer and rotator cuff repair: a case report, Journal of Surgical Case Reports, Volume 2022, Issue 5, May 2022, rjac201, https://doi.org/10.1093/jscr/rjac201
Close - Share Icon Share
Abstract
We report a 45-year-old man who presented with a rotator cuff tear and scapular dyskinesis of his left shoulder and underwent a pectoralis major split transfer with an allograft to the inferior border of his scapula. The patient reported significant improvement in shoulder function and decreased severity of his scapular dyskinesis. Combined arthroscopic rotator cuff repair and allograft scapula stabilization is a novel technique for the unusual clinical presentation reported in this case report. To the best of our knowledge, this is the first reported surgical management of a patient with rotator cuff repair and non-palsy-related scapular dyskinesis.
INTRODUCTION
Scapular mechanics are essential for adequate shoulder function. The most common cause of scapular dyskinesis is neuropathic; however, scapular dyskinesis can have other non-neurogenic causes, such as disruptions within the muscular and tendinous components of scapular stabilization. Surgical intervention is indicated in patients with scapular dyskinesis in the presence of structural compromise of the glenohumeral (GH) or acromioclavicular (AC) joints [1, 2]. Studies in the literature have described management of scapular dyskinesis with AC and coracoclavicular ligamentous involvement, serratus anterior injury and combined rhomboid and trapezius injuries [3–11]. However, management of patients with significant scapular dyskinesia and concomitant tears of the rotator cuff is unclear. We present the first report of traumatic scapular dyskinesis and associated full-thickness tear of the supraspinatus managed by a pectoralis major split transfer augmented with a tibialis anterior allograft to the inferior border of the scapula.
CASE REPORT
This is a case report of a right-hand dominant 45-year-old male that sustained a 32-foot fall and landed on his left shoulder. Three months after his injury, he presented with persistent pain in his left shoulder, especially in the medial scapula, with minimal improvement in pain and range of motion of his shoulder. He presented with significant scapular dyskinesis, which he noticed began after his injury (Fig. 1a). He was able to abduct his shoulder to 90°, forward flex to 90°, externally rotate to 5° and internally rotate to L4. With his arms at his side, his left scapula was located inferior and lateral to the spine when compared with the right scapula. With shoulder abduction, his left scapula moved more lateral and superior compared with his right side. Forced reduction of his left scapula allowed the patient to have about 180° of shoulder flexion (Fig. 1b).
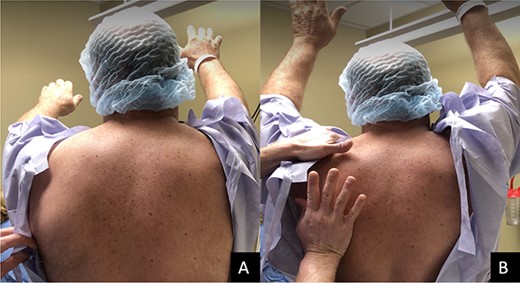
(A) Limited forward flexion to 90° with significant inferior and lateral to the spine when compared with the right scapula. (B) Forward shoulder flexion to about 180° with forced reduction on the scapula.
Magnetic resonance imaging (MRI) demonstrated a full-thickness tear of the distal supraspinatus tendon and a partial-thickness articular sided tear of the infraspinatus tendon (Fig. 2).
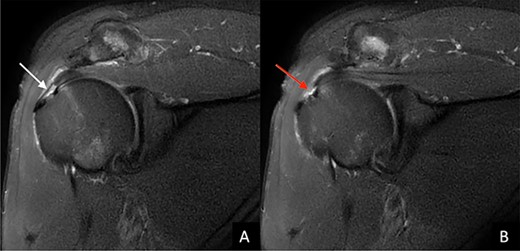
T2-weighted coronal MRI image of the left shoulder shows (A) the degree of medial to lateral involvement (white arrow) of (B) the full thickness tear of the distal portion of the supraspinatus tendon.
Electromyography study showed no electrodiagnostic evidence of a left long thoracic mononeuropathy or radiculopathy affecting the left upper extremity (UE).
Based on MRI findings of a full-thickness tear of the supraspinatus tendon and the lack of functional and pain improvement of his shoulder for several months, the patient was indicated for arthroscopic repair of his supraspinatus. A pectoralis major split transfer to the inferior border of his scapula was also offered to provide scapular stabilization and improve function of the patient’s shoulder.
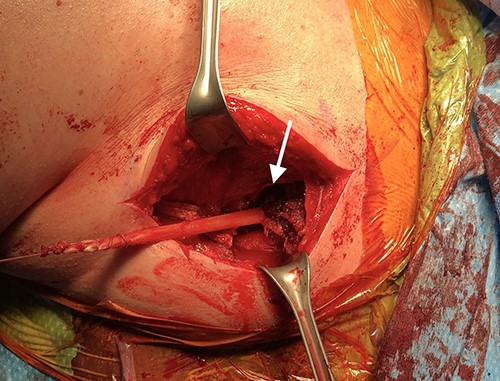
An incision was made using a deltopectoral approach distally. The sternal border of the pectoralis major muscle was identified, traced out laterally, and removed sharply from the periosteum (Fig. 3). After mobilizing the pectoralis major, a tibialis anterior autograft was prepared on the back table; each side was tagged with a fiber loop, and a Pulvertaft weave was used to connect the graft to the pectoralis major (Figs 4 and 5).
Intraoperative photograph showing the surgical exposure using the deltopectoral approach (A). The pectoralis major muscle is identified and tagged, demonstrated by the white arrow (B).
Intraoperative photograph shows the tibialis anterior graft with the Pulvertaft weave onto the pectoralis major. The white arrows show the insertion of the tibialis anterior graft onto the pectoralis major muscle.
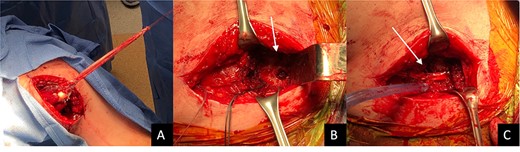
Intraoperative photograph shows the semi-T whipstitched graft at full length (A). The white arrow in (B) shows the 9-mm hole drilled in the inferior border of the scapula. The white arrow in (C) shows the semi tendinosis transferred through the whole and tied to itself with #2 FiberWire®.
A posterior portal approach was then performed to address the rotator cuff. Two medial row anchors were placed, and tape was passed from anterior to posterior to get four passes with a suture limb in each pass to get appropriate compression of the cuff.
The patient was evaluated at 2 weeks, 6 weeks, 3 months, 6 months and 8 months postoperatively. His shoulder motion improved (forward flexion to 150° and external rotation to 85°) and he was able to reach his back pocket. His lateral slide test was negative for scapular dyskinesia, and he had a subtle positive Scapular Dyskinesia Test (Videos 1 and 2).
Patient-reported outcome measures were administered to the patient postoperatively for preoperative function as well as postoperative function. PROS included the Patient-Reported Outcomes Measurement Information System (PROMIS) UE and Pain Interference (PI), the American Shoulder and Elbow Surgeons (ASES) form and the Visual Analog Scale (VAS) for pain. His patient-reported outcome scores showed clinically significant improvement using the respective minimal clinically important change score (MCID) values for rotator cuff repairs via PROMIS UE(4.02), PROMIS PI(−4.12), ASES(27.1) and VAS(2.4) [12, 13].
DISCUSSION
Despite the well-known relationship between the scapula and shoulder, there is limited evidence to support whether shoulder dysfunction contributes to developing scapular dyskinesia or vice versa [1].
Tamai et al. in 1983 first reported a case of a 31-year-old male that presented with scapular dyskinesis and an intratendinous tear of the supraspinatus tendon [14]. The patient underwent an open rotator cuff repair that failed and required the patient to undergo revision surgery with more aggressive debridement of his rotator cuff. There was no long-term follow-up and there is uncertainty with the amount of shoulder function that was restored following surgical intervention.
Lo et al. recently reported on a 21-year-old woman with reducible scapular dyskinesis similar to the patient from this case report, but the patient’s dyskinesis was secondary to a long thoracic nerve palsy [15]. The patient was treated with an open split pectoralis major tendon transfer to salvage shoulder motion. In the setting of intractable shoulder instability and reducible scapular dyskinesis, Lo et al. showed that it is reasonable to consider surgical intervention for both the GH and scapulothoracic pathologies. The patient also had a longer history of shoulder instability and scapular dyskinesis, compared with the patient presented in this case report that had an acute presentation.
In our case report, the patient had an acute, traumatic rotator cuff tear following a fall to his shoulder with subsequent scapular dyskinesis. Reduction of the patient’s scapula allowed him to gain full range of motion of his shoulder, suggesting that his torn rotator cuff was likely the cause of both his shoulder and scapular dysfunction. Our assumptions are further supported by the restoration of shoulder function seen by the patient during his follow-up visits postoperatively.
To our knowledge, this is the first report on a surgical technique describing a combined soft tissue rebalancing of an acutely torn rotator cuff with associated scapular dyskinesis. Combined arthroscopic rotator cuff repair and allograft scapula stabilization is a novel technique and a viable option for the unusual case presentation reported in this case report.
CONFLICT OF INTEREST STATEMENT
The authors have no conflicts of interest to declare.
FUNDING
None.



