-
PDF
- Split View
-
Views
-
Cite
Cite
John Mikhail, Gregory Kennedy, Sunil Singhal, Isabella Tondi Resta, Bilal Nadeem, Feredun Azari, Chronic unrelenting cough secondary to pericardial cyst impingement of right phrenic nerve, Journal of Surgical Case Reports, Volume 2022, Issue 5, May 2022, rjac123, https://doi.org/10.1093/jscr/rjac123
Close - Share Icon Share
Abstract
Located in the mediastinum, pericardial cysts are rare and benign congenital abnormalities commonly identified as incidental findings on imaging. However, some patients with abnormally enlarged cysts present with compressive symptoms, which include recurrent infections, tamponade from cardiac compression and respiratory complications. Our report highlights a challenging case of a patient with recurrent respiratory symptoms secondary to phrenic nerve compression. Misdiagnosis over the past decade resulted in ineffective interventions. After clear identification of the cyst compression of the ipsilateral phrenic nerve, the patient underwent a minimally invasive robotically assisted cyst resection with phrenic nerve preservation that alleviated respiratory symptoms.
INTRODUCTION
Pericardial cysts are rare, benign congenital abnormalities located in the mediastinum. They are most commonly detected at the costophrenic angle (right 70%, left 22%), or, rarely, in the mediastinal compartments (8%) [1, 2]. Pericardial cysts are usually asymptomatic (>50%) and are mostly found incidentally on radiographic imaging [3]. Occasionally, when they do become symptomatic, they are associated with complications such as recurrent infections, tamponade from local compression into the cardiac cavity, hemorrhage and respiratory symptoms that may necessitate treatment [4]. Common signs and symptoms described in the literature include dyspnea, chest pain, hemoptysis, or rarely, a chronic cough [3].
We present a rare, challenging case of a patient with a worsening chronic cough. Multiple physicians over several years were unable to make a diagnosis. A computed tomography (CT) scan uncovered a pericardial cyst which was not expected to explain the symptoms. However, due to lack of medical options, a decision to remove the cyst relieved the cough. In surgery, an anatomical explanation was uncovered.
CASE PRESENTATION
A 66-year-old female presented with a medical history of severe persistent allergic asthma, morbid obesity with obstructive sleep apnea on nightly rest, continuous positive airway pressure, deep vein thrombosis on anticoagulation and pulmonary embolism. Over a 14-year period, the patient was evaluated for a worsening, chronic non-productive cough without clear diagnosis. The patient underwent multiple medical and invasive interventions without relief. Use of different bronchodilators, high-dose steroids, proton pump inhibitors for presumed reflux bronchitis, benzodiazepines, antihistamines, monoclonal antibodies (omalizumab), as well as Botox injections to the vocal cord for suspected irritable larynx syndrome did not alleviate the unrelenting chronic cough experienced by the patient.
At the time of presentation to the pulmonologist, the patient was afebrile with a normal cardiopulmonary exam and vital signs. Chest X-ray revealed an enlarged right-sided heart border (Fig. 1). CT showed multiple sub-centimeter bilateral pulmonary nodules as well as a 6 x 2 cm right-sided pericardial cyst (Fig. 1). Further evaluation by MRI demonstrated gadolinium enhancement on T2 sequences with hypo enhancement noted on T1 sequences, confirming that the lesion was fluid-filled and cystic in nature.
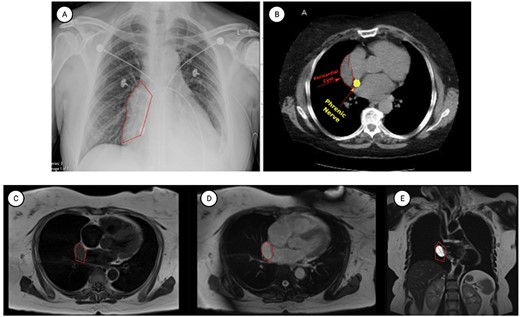
Representative images of pericardial cysts on commonly employed imaging modalities. (A) The chest X-ray imaging of the patient described in the case report AP CXR showing widened mediastinum in a patient with a wide differential diagnosis which ultimately was found to be pericardial cyst. (B) CT imaging of the patient described in the case report with representative images of our patient demonstrating a sizeable pericardial cyst marked with red arrows and its close association with right phrenic nerve marked in gold. (C–E) MRI T1 (C) and T2 (D–E) appearances of pericardial cysts. Representative images of pericardial cyst appearance on gadolinium-enhanced MRI sequences. *Figure edited with BioRender.
Given the patient’s medical history and co-morbidities, discussion was held regarding non-surgical options, including percutaneous aspiration. However, such options would not allow a full histopathologic assessment of the lesion. Moreover, the patient reported that the cough significantly limited her activities of daily living. Considering that pericardial cysts recur at a rate of 33% along with the patient’s desire to proceed with a durable solution to her respiratory complications, the patient was referred to the thoracic surgery service [5].
After careful preoperative screening, she underwent minimally invasive robotic assisted thoracoscopic resection of her pericardial cyst. Robotic-assisted thoracoscopic surgery (RATS) at large medical centers is a safe technique with minimal post-operative physical limitation and swift return to activities to daily life. RATS-guided resection allowed the patient to undergo potentially curative resection compared with other non-surgical techniques that have considerable recurrence risk.
OPERATIVE TECHNIQUE
Patient was brought to the operating theatre and placed in a left-lateral decubitus position. She was intubated with a dual lumen endotracheal tube, which allowed for single-lung ventilation during surgery. Initial camera port was placed at the ninth intercostal space at the mid-axillary line. After the pleura was inspected, additional working ports were placed at the (2 ports) eighth and (1 port) fifth intercostal spaces. Once the ports had been safely inserted, the robotic system was docked, and surgical dissection was initiated.
Dissection of the offending pericardial cysts showed intimate adherence and compression of the phrenic nerve. Involvement of the phrenic nerve was thought to be the predominant cause of the patient’s treatment resistant cough. Using the high degree of articulation afforded by the robotic dissectors, the phrenic nerve was carefully isolated and preserved from the pericardial cyst (Fig. 2). Given the significant compression of the nerve noted intra-operatively, the diaphragm was carefully inspected. The diaphragm did not demonstrate atrophy and ultimately was not plicated given the absence of preoperative radiographic signs of diaphragmatic paralysis.
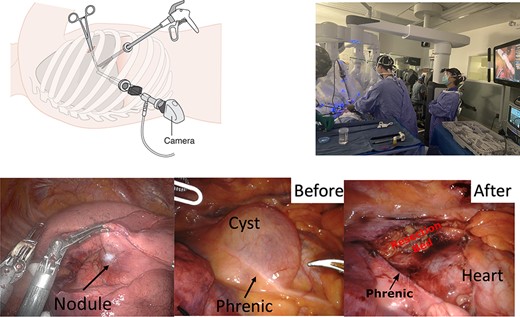
Top row: intra-operative patient positioning, instrument placement and robotic device deployment for minimally invasive thoracoscopic resections. CC4.0: CRUK Wikimedia commons bottom row: left column: mobilization of the right upper lobe with visualization of a SPN noted on preoperative cross-sectional imaging. Middle column: visualization of the pericardial cyst which demonstrates very close relationship and compression of the right phrenic nerve. Right column: the pericardial cyst was removed and resection showing preservation of the nerve.
Post-operatively, the patient did not have additional respiratory difficulties and there was no evidence of unilateral diaphragmatic paralysis on follow-up roentgenograms. Patient was observed on the regular surgical floor without any need for intensive care management. Chest tubes did not demonstrate air leakage and were removed on post-operative Day 2 at the time of discharge. Two weeks post operatively, the patient reported |$\sim$|90% improvement in her cough using the cough-specific quality of life questionnaire [6] and had discontinued many of her maintenance medications. In addition, there was a significant improvement of patient’s respiratory mechanics and pulmonary function parameters [FEV1 61(pre)–78% (post), FVC 68 (pre)–81% (post)]. Final histopathologic evaluation showed the cyst to be unilocular with thin fibrous wall lined with bland epithelium without papillary hyperplasia (Fig. 3).
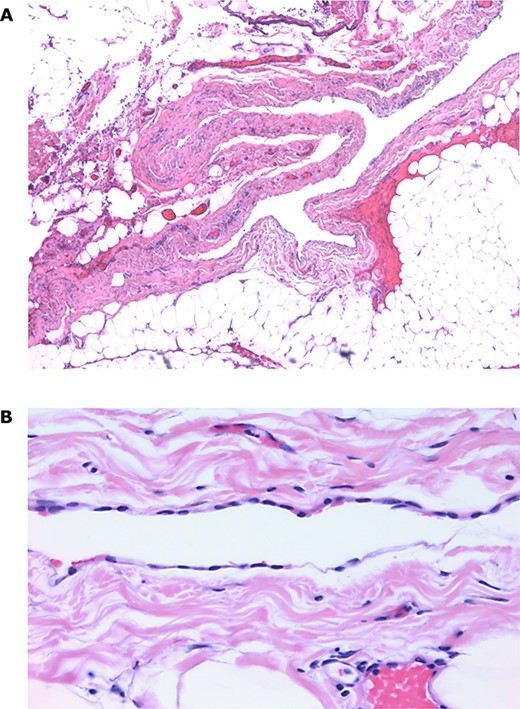
Histopathologic analysis of the pericardial cyst. (A) Pericardial cyst lining demonstrating fibrous wall surrounded by pericardial fat and blood vessels (×5 image); (B) Simple pericardial cyst lining surrounded by fibrous wall (×40 image).
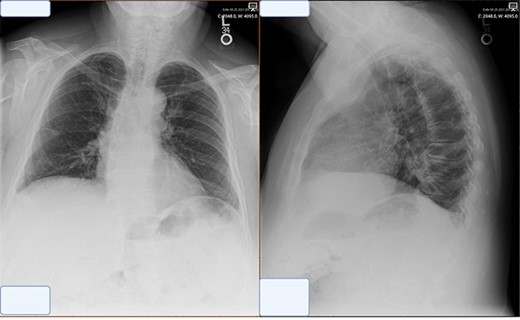
Post-operative chest X-ray obtained at 2 week follow-up showing trace pleural effusion and otherwise normal X-ray.
DISCUSSION
Pericardial cysts are an uncommon cause of mediastinal masses. Their estimated prevalence is 1/100 000 [1, 7]. Cysts usually range in size from 2 to 3 cm but have been reported as large as 28 cm [8]. Our patient presented with a chronic non-productive cough and was found to have a larger 6 cm pericardial cyst causing local compression of the adjacent phrenic nerve. This case is unique as there are a few reported cases in the literature where cough is the predominant presenting symptom. Usually, these cysts are discovered incidentally on imaging and require further evaluation on cross-sectional imaging to arrive at accurate diagnosis. This report describes a seldom encountered manifestation of this rare disease where the cyst is significantly compressing the phrenic nerve to the degree of changing the patient’s respiratory mechanics.
CT and echocardiography are the preferred modality of diagnosis [7, 9]; however, cardiac magnetic resonance imaging can also offer a superb, detailed anatomic evaluation of pericardial lesions during preoperative workup [3].
Surgery has been identified as the only definitive cure. Advent of minimally invasive thoracoscopic techniques has significantly reduced the morbidity associated with resection of pericardial cysts. Use of robotic-assisted technology has added benefits in this realm as the extra degree of articulation afforded by instruments allows particularly safe removal of cysts from anatomically challenging locations such as the mediastinal cavities. In contrast, prior open surgical techniques such as median sternotomy and posterolateral thoracotomy subjected the patient to increased post-operative pain and hospital length of stay. Given the potential benefits with minimal morbidity associated with surgical intervention, it would seem reasonable to offer resection for all pericardial cysts in otherwise healthy symptomatic patients particularly in those with local compressive findings such as our patient [8, 10].
CONCLUSION
Although rare, pericardial cysts should not be ignored as a cause of chronic cough. Surgical options should be considered in symptomatic patients with low risk for complications.
FUNDING
Feredun Azari: supported by Stephen CC Cheung Fellowship in Surgical Oncology. Gregory T. Kennedy: American Philosophical Society.



