-
PDF
- Split View
-
Views
-
Cite
Cite
Tushar Ranjan Dalei, Barada Prasanna Samal, Asish Kumar Gupta, Rajesh Senapati, Tarini Prasad Sahoo, Coraco-clavicular endobutton and fiber tape fixation for Neer’s type II unstable lateral clavicular fracture: a case series with literature review, Journal of Surgical Case Reports, Volume 2022, Issue 4, April 2022, rjac120, https://doi.org/10.1093/jscr/rjac120
Close - Share Icon Share
Abstract
Neer’s type II lateral end clavicle fracture is inherently unstable due to coraco-clavicular ligament disruption. Timely surgery can avoid complications of conservative management. Our study is based on open reduction and fixation with double endobutton and fibre tape in 12 patients. Radiological and functional outcome were assessed using Quick DASH score and SPADI score at regular interval. All the fractures achieved both clinical and radiological union. No intra-operative or post-operative complication was noted. Functional out come and range of motion at 1-year follow-up was quite satisfactory. Open reduction and fixation with double endobutton and fibre tape for lateral end clavicle fracture is a quite rewarding surgery with less steep learning curve, economical and enough stable fixations leading to union and good functional outcome without need of re-surgery for implant removal.
INTRODUCTION
Approximately 10–25% of clavicle fractures occur in the distal third segment and are usually caused by direct trauma to the shoulder due to fall in adults [1]. Treatment of these injuries depends on the displacement and stability of the distal end of the clavicle, as determined by the status of the coraco-clavicular ligament. In Neer’s type 2 fractures in which the coraco-clavicular ligaments are either attached to the lateral fragment or torn, there is significant superior clavicle displacement [3]. Owing to this displacement, there is a high chance of non-union (25–44%) if these cases are not managed operatively [4, 5]. Persistent pain, restricted movement and loss of strength and endurance of the shoulder are also frequently associated with this non-union. Management of such established non-union is quite difficult and technically challenging; hence, timely surgery is frequently recommended as the primary treatment [2–5].
Operative modalities, as described in literature, include direct osteosynthesis using anatomical pre-contoured locking plate fixation or hook plate fixation or indirect coraco-clavicular ligament stabilization using suture anchor, coraco-clavicular screw fixation, double looped endobutton, etc. Indirect fixation works by neutralizing the deforming forces on the fracture fragment, thus converting the unstable fracture into a stable pattern. This process permits fracture healing by direct apposition of the fracture fragment without the use of any significant hardware. The endobutton technique is a new and simple technique that has been proposed to overcome the complications of direct osteosynthesis, with an excellent outcome [26]. In due consideration of the above facts, we performed a prospective study on Neer’s type II distal clavicle fracture fixation using double endobutton (BIOTEK ON Button) stabilization with fibre tape system (BioFiber 2 mm). The short-term clinical and functional outcomes have been described herein.
MATERIAL AND METHODS
After obtaining the requisite institutional ethical committee approval, this study was conducted in a prospective manner in VIMSAR, Burla, Odisha, India. All patients with acute Neer’s type II lateral end clavicle fractures who were aged <50 years and presented between June 2019 and June 2020 were included in the study. Open fractures, fractures with neurovascular injury and patients with concomitant shoulder pathology were excluded.
Surgical technique
All surgeries were performed by a single surgical group after obtaining necessary pre-operative investigations. Implants used in this method of fixation were two endobuttons (BIOTEK ON Button) with a fibre tape system (BioFibre, 2 mm in size). Under general anaesthesia, maintaining the beach chair position, a 6-cm bra-strap incision was made from the lateral end clavicle to the coracoid tip. After the separation of the deltotrapezial fascia, the coracoid was identified and a drill hole of 3.2 mm was created at its base (Fig. 2A). Following which, fracture site was opened; freshened and provisionally fixed with a k wire. A similar drill hole was also made over the proximal fragment of the clavicle (Fig. 2B). With the help of a 26G thin SS wire, the endobutton was positioned just below the coracoid and the fibre tape passing through the endobutton was drawn out at the superior surface of the coracoid process (Fig. 2C).The fibre tape was tied over another endobutton placed at the proximal end of the clavicle to maintain the reduction (Fig. 2D). Intra-operative reduction was confirmed fluoroscopically prior to wound closure. Post-operatively, the shoulder was immobilized with an arm sling. Abduction of the shoulder was delayed for 3 weeks. After the surgery, the patients were followed up at 1.5-, 3- and 6-month and 1-year intervals for assessing the radiological and clinical outcomes. There was no loss to follow-up. At the last follow-up, which was nearly a year after the surgery, range of motion and functional outcome scores such as Quick Disabilities of the Arm, Shoulder and Hand score (QDASH score) and the Shoulder Pain and Disability Index score (SPADI score) were calculated. Complications such as infection, implant failure and need for reoperation were noted in the datasheet and were analyzed. Maintenance of reduction and fracture union were observed in each visit by obtaining radiographs in a suitable position (Fig. 1). To avoid inter-observer bias, the scores were calculated by two separate residents and the mean was taken as the final reading.
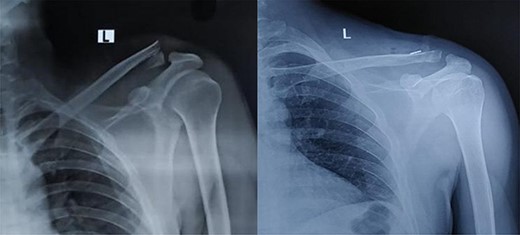
Pre op and 1-year follow-up X-ray image of Neer’s type II unstable lateral end clavicle fracture.
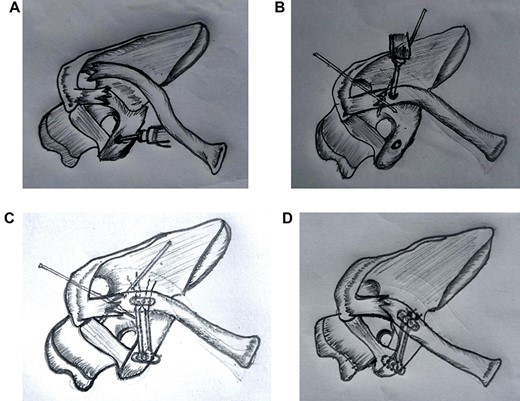
(A) After exposing coracoid a drill hole was made at the base Coracoid with 3.2-mm drill bit. (B) Fracture reduced and provisionally fixed with k wire and a Drill hole was made over clavicle medial to fracture. (C) Fibre tape entangled in endobutton passed through drill hole of coracoid and subsequently through a drill hole of clavicle with the help of 26G ss wire. (D) Final construct with second endobutton over clavicle and fibre tape tied followed by removal of k - wire.
Statistical analysis
In this study, continuous variables such as age, waiting period for surgery and duration of surgery were expressed as mean and range. On the other hand, the range of motion and functional outcome scores were evaluated as mean ± standard deviation (SD) using descriptive statistics.
RESULTS
A total of 12 patients were included in the study following the application of the inclusion and exclusion criteria. The mean age of our study group was 30.5 years (range: 22–39 years). There were nine men and three women. Right and left shoulder involvements were in equal proportions. The predominant mode of injury was road traffic accident, except two cases in which the injury was due to a fall. The mean waiting period for the surgery was 4.167 days (range: 2–7 days), and the mean duration of the surgery was 52.08 minutes (range: 40–70 minutes). Epidemiology, final functional outcome scores and range of motion at final follow-up are listed in Table 1.
| Sl No . | Age . | Time to surgery(in days) . | Surgery time (minutes) . | QDASH score . | SPADI SCORE . | RANGE OF MOTION . | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| PAIN . | DISABILTY . | COMBINED . | FF . | EXT . | ABD . | |||||
| 1 | 22 | 2 | 45 | 4.5 | 6 | 3.8 | 4.6 | 160 | 50 | 160 |
| 2 | 26 | 7 | 50 | 6.8 | 8 | 3.8 | 5.4 | 120 | 50 | 120 |
| 3 | 27 | 5 | 60 | 9.1 | 10 | 6.3 | 7.7 | 120 | 60 | 120 |
| 4 | 37 | 3 | 40 | 11.4 | 10 | 5 | 6.9 | 120 | 40 | 100 |
| 5 | 32 | 4 | 40 | 4.5 | 6 | 3.8 | 4.6 | 120 | 50 | 160 |
| 6 | 33 | 4 | 45 | 11.4 | 10 | 6.3 | 7.7 | 140 | 50 | 120 |
| 7 | 29 | 5 | 50 | 9.1 | 8 | 7.5 | 7.7 | 100 | 50 | 100 |
| 8 | 39 | 4 | 50 | 4.5 | 6 | 3.8 | 4.6 | 160 | 60 | 160 |
| 9 | 33 | 6 | 50 | 6.8 | 6 | 3.8 | 4.6 | 160 | 60 | 160 |
| 10 | 31 | 3 | 60 | 4.5 | 8 | 5 | 6.2 | 120 | 60 | 160 |
| 11 | 29 | 2 | 70 | 4.5 | 6 | 5 | 5.4 | 120 | 60 | 120 |
| 12 | 28 | 5 | 65 | 6.8 | 6 | 3.8 | 4.6 | 160 | 60 | 120 |
| Sl No . | Age . | Time to surgery(in days) . | Surgery time (minutes) . | QDASH score . | SPADI SCORE . | RANGE OF MOTION . | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| PAIN . | DISABILTY . | COMBINED . | FF . | EXT . | ABD . | |||||
| 1 | 22 | 2 | 45 | 4.5 | 6 | 3.8 | 4.6 | 160 | 50 | 160 |
| 2 | 26 | 7 | 50 | 6.8 | 8 | 3.8 | 5.4 | 120 | 50 | 120 |
| 3 | 27 | 5 | 60 | 9.1 | 10 | 6.3 | 7.7 | 120 | 60 | 120 |
| 4 | 37 | 3 | 40 | 11.4 | 10 | 5 | 6.9 | 120 | 40 | 100 |
| 5 | 32 | 4 | 40 | 4.5 | 6 | 3.8 | 4.6 | 120 | 50 | 160 |
| 6 | 33 | 4 | 45 | 11.4 | 10 | 6.3 | 7.7 | 140 | 50 | 120 |
| 7 | 29 | 5 | 50 | 9.1 | 8 | 7.5 | 7.7 | 100 | 50 | 100 |
| 8 | 39 | 4 | 50 | 4.5 | 6 | 3.8 | 4.6 | 160 | 60 | 160 |
| 9 | 33 | 6 | 50 | 6.8 | 6 | 3.8 | 4.6 | 160 | 60 | 160 |
| 10 | 31 | 3 | 60 | 4.5 | 8 | 5 | 6.2 | 120 | 60 | 160 |
| 11 | 29 | 2 | 70 | 4.5 | 6 | 5 | 5.4 | 120 | 60 | 120 |
| 12 | 28 | 5 | 65 | 6.8 | 6 | 3.8 | 4.6 | 160 | 60 | 120 |
| Sl No . | Age . | Time to surgery(in days) . | Surgery time (minutes) . | QDASH score . | SPADI SCORE . | RANGE OF MOTION . | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| PAIN . | DISABILTY . | COMBINED . | FF . | EXT . | ABD . | |||||
| 1 | 22 | 2 | 45 | 4.5 | 6 | 3.8 | 4.6 | 160 | 50 | 160 |
| 2 | 26 | 7 | 50 | 6.8 | 8 | 3.8 | 5.4 | 120 | 50 | 120 |
| 3 | 27 | 5 | 60 | 9.1 | 10 | 6.3 | 7.7 | 120 | 60 | 120 |
| 4 | 37 | 3 | 40 | 11.4 | 10 | 5 | 6.9 | 120 | 40 | 100 |
| 5 | 32 | 4 | 40 | 4.5 | 6 | 3.8 | 4.6 | 120 | 50 | 160 |
| 6 | 33 | 4 | 45 | 11.4 | 10 | 6.3 | 7.7 | 140 | 50 | 120 |
| 7 | 29 | 5 | 50 | 9.1 | 8 | 7.5 | 7.7 | 100 | 50 | 100 |
| 8 | 39 | 4 | 50 | 4.5 | 6 | 3.8 | 4.6 | 160 | 60 | 160 |
| 9 | 33 | 6 | 50 | 6.8 | 6 | 3.8 | 4.6 | 160 | 60 | 160 |
| 10 | 31 | 3 | 60 | 4.5 | 8 | 5 | 6.2 | 120 | 60 | 160 |
| 11 | 29 | 2 | 70 | 4.5 | 6 | 5 | 5.4 | 120 | 60 | 120 |
| 12 | 28 | 5 | 65 | 6.8 | 6 | 3.8 | 4.6 | 160 | 60 | 120 |
| Sl No . | Age . | Time to surgery(in days) . | Surgery time (minutes) . | QDASH score . | SPADI SCORE . | RANGE OF MOTION . | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| PAIN . | DISABILTY . | COMBINED . | FF . | EXT . | ABD . | |||||
| 1 | 22 | 2 | 45 | 4.5 | 6 | 3.8 | 4.6 | 160 | 50 | 160 |
| 2 | 26 | 7 | 50 | 6.8 | 8 | 3.8 | 5.4 | 120 | 50 | 120 |
| 3 | 27 | 5 | 60 | 9.1 | 10 | 6.3 | 7.7 | 120 | 60 | 120 |
| 4 | 37 | 3 | 40 | 11.4 | 10 | 5 | 6.9 | 120 | 40 | 100 |
| 5 | 32 | 4 | 40 | 4.5 | 6 | 3.8 | 4.6 | 120 | 50 | 160 |
| 6 | 33 | 4 | 45 | 11.4 | 10 | 6.3 | 7.7 | 140 | 50 | 120 |
| 7 | 29 | 5 | 50 | 9.1 | 8 | 7.5 | 7.7 | 100 | 50 | 100 |
| 8 | 39 | 4 | 50 | 4.5 | 6 | 3.8 | 4.6 | 160 | 60 | 160 |
| 9 | 33 | 6 | 50 | 6.8 | 6 | 3.8 | 4.6 | 160 | 60 | 160 |
| 10 | 31 | 3 | 60 | 4.5 | 8 | 5 | 6.2 | 120 | 60 | 160 |
| 11 | 29 | 2 | 70 | 4.5 | 6 | 5 | 5.4 | 120 | 60 | 120 |
| 12 | 28 | 5 | 65 | 6.8 | 6 | 3.8 | 4.6 | 160 | 60 | 120 |
During the final follow-up at 12 months, the mean QDASH score was 6.99 ± 2.67 and the mean combined SPADI score was 5.83 ± 1.33 (pain component mean: 7.5 ± 1.73; disability component means: 4.82 ± 1.27). The mean range of motion at the final assessment was forward flexion 133.3 ± 21.46, extension 54.17 ± 6.68 and abduction 133.3 ± 24.61. Regarding the radiological outcomes, there was no failure of fixation or loss of reduction over the entire follow-up period. Bony union was achieved in all cases in a mean duration of 12.8 weeks. No intra-operative complication was noted, and there was no post-operative infection or peri-operative fracture. None required revision or additional surgery. All the patients were comfortable in their daily activities within 6 weeks of surgery and returned to their jobs before the final follow-up.
DISCUSSION
Lateral end clavicle fracture, especially Neer’s type II, needs special mention because of its unstable pattern. The constant pull of the muscle force proximally by the trapezius and distally by the weight of the arm on the shoulder girdle makes this fracture unsuitable for conservative management. Solid evidence-based guidelines regarding its management are not available. Conservative treatment of the distal end clavicle fracture with detachment of the coraco-clavicular ligament in adults does not yield satisfactory results and may necessitate delayed surgical intervention because of symptomatic non-union [3, 4].
The surgical techniques described in literature broadly constitute three groups: tension band and/or trans articular K-wire fixation through acromioclavicular joint (ACJ), direct osteosynthesis using distal clavicle plates (±CC ligament augmentation) or hook plates and indirect reduction using CC ligament reconstruction (TightRope or Dog Bone technique, Surgilig, parachute technique, etc.) ± direct ligament repair [2].
Although locking plate fixation is a stable fixation method with a high rate of union, it is of no avail if the distal fragment is small or comminuted. Vaishya et al. [6], Lee et al. [7] and Shin et al. [8] achieved clinical union in all cases using locking plate, with a few complications such as superficial infection and malunion. Shoulder function at the end of the follow-up was good to excellent irrespective of the coraco-clavicular distance restoration [7, 8]. Augmenting the CC ligament with suture anchor or endobutton in addition to the locking plate obviates the absolute need for implant removal with no inferior clinical, radiological or functional outcomes [13, 14].
Hook plate is another popular option for lateral end clavicle fracture; however, it is not favoured nowadays because of the higher risk of major complications such as reoperation and implant failure when compared with intramedullary fixation and sutures [28, 29]. Among the various complications of the hook plate, those requiring mention are subacromial space inflammation, rotator cuff impingement, hook cut-out, acromion osteolysis and fractures [2, 15].
CC stabilization is an indirect and flexible type of fracture fixation that was first described by Neer in 1990. This stabilization can be achieved by sutures only, suture anchors, fibre tape, suture button devices or a combination of the above-mentioned materials. Biomechanical evaluation of the different fixation methods for distal clavicle fracture revealed the lack of significant difference in the load to failure under tension among the locking plate, hook plate and coraco-clavicular suture systems [17]. Moreover, a recent study by Yagnik et al. [18] has highlighted the advantages of coraco-clavicular button fixation, namely, 75% greater strength than the traditional locking plate and lower hardware-related complications.
CC stabilization using various types of absorbable and non-absorbable sutures (Vicryl tape, Mersilene tape, PDS No, 1) [9, 16, 25, 27] with a fairly consistent technique of under the coracoid around the clavicle suture passage yielded encouraging results. According to a meta-analysis, the union rate of these techniques is ~98% [28, 29]. The observed complications were knot slippage, loss of reduction, knot prominence and coracoid fracture. Although CC stabilization using cannulated screw resulted in a union rate of 100%, screw loosening, mandatory implant removal and interference with the range of shoulder motion are some of the reported drawbacks [11].
The use of suture anchors, double button and continuous loop techniques are mere modifications of the aforesaid suture-only technique for CC stabilization [10, 12, 14]. Our study was mainly inspired by the encouraging results of Robinson et al. in their 16 cases using open reduction and CC stabilization with double endobutton and Orthocod suture. They had one case of asymptomatic fibrous union. The Mean Constant score was 87.1, and the median Disabilities of the Arm, Shoulder and Hand score was 3.3 at 1-year follow-up [26]. The double endobutton technique requires minimal soft tissue dissection and causes negligible skin irritation by the metal implant [2, 20, 29]. We used two loose buttons and a fiber tape of 2 mm, which makes our construct quite economical. A slightly modified technique of bidirectional clavicular loop fixation using two endobuttons over the clavicle showed enlargement of the clavicular drill hole on long-term follow-up, but migration of the endobutton was not noticed [19]. Struhl et al. [30] used an expensive, readymade closed-loop double endobutton for CC stabilization and obtained encouraging results. According to them, passing cerclage wire through the drill hole in the coracoid instead of under the coracoid prevents anterior overreduction of the fracture as well as late fracture due to bone erosion [30]. TightRope, which is a suture button device of adjustable length, prevents knot fixation and anatomically restores the coraco-clavicular interval. Its usage as a CC stabilizer resulted in a union rate of ~95%, but a few complications such as non-union, malunion, intra-operative coracoid fracture and shoulder stiffness were observed. However, up to the 1-year follow-up, we did not note any complications in our case series [12].
A few comparison studies are worth mentioning here. Comparing suture anchor and hook plate in the treatment of distal clavicle fracture found that none is superior to the other [12]. A similar study comparing the coraco-clavicular loop technique with the hook plate concluded that despite significantly better functional outcome and lower complication rate in the coraco-clavicular loop group at the final follow-up, the radiologic non-union rate failed to show any significant differences between the two groups [21].
Arthroscopic coraco-clavicular fixation for lateral end clavicle fracture is now the emerging concept. It has a steep learning curve, with the disadvantage of being costly and time-consuming. However, our technique is very easy to learn and practice and is economical. Less post-operative pain, minimal wound complication and the ability to simultaneously address the shoulder pathology are some the advantages of arthroscopic CC stabilization [22–24]. Further studies involving a larger number of patients with uniformity of the fixation technique are the need of the hour to draw a firm conclusion in case of technically demanding procedures such as arthroscopic CC fixation.
CONCLUSION
Open double endobutton with fiber tape fixation of the displaced Neer’s type II lateral clavicular fracture is a safe, reproducible and technically less demanding surgical procedure with satisfactory radiological and short-term clinical outcomes. Shortened surgery time as well as hospital stay and minimal complications strongly indicate that the fire tape and endobutton device is a promising option for the fixation of unstable lateral end clavicle fracture.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



