-
PDF
- Split View
-
Views
-
Cite
Cite
Wejdan A Alghamdi, Alaa A Roublah, Jaudah Almaghrabi, Haytham H Alabbas, Appendix diverticulosis in a patient diagnosed on pathology after laparoscopic appendectomy for appendicular mucinous mass—case report and literature review, Journal of Surgical Case Reports, Volume 2022, Issue 4, April 2022, rjac094, https://doi.org/10.1093/jscr/rjac094
Close - Share Icon Share
Abstract
Diverticulum of the appendix is uncommon cause of right iliac fossa pain and inflammation with delayed diagnosis and high risk of complications, as it mimics acute appendicitis. Here we present a case of an elderly male patient who had lung cancer post-treatment. During the follow-up, appendicle lesion was discovered and suspected to be mucinous appendix. The pathology reported after appendectomy as appendicular diverticulosis without evidence of malignancy. As appendicular diverticulum is best confirmed by pathology, still its clinical presentation is difficult to be distinguished from other appendicular diseases. It is frequently linked to increased risk of cancer, particularly carcinoid tumors and mucinous adenomas.
INTRODUCTION
Appendicular diverticulum (AD) is considered as one of the rare entities, which was firstly reported in 1893 by Kelynack, and its reporting incidence is up to 2% [1]. Despite that AD is a pathological diagnosis, clinically and radiologically it can mimic acute appendicitis (AA) [1, 2]. Toh et al. [3] has reported a remarkable increase of malignancy rate and complications such as perforation in association of the AD. Here we report a case of AD initially diagnosed as a case of appendicular mucocele in elderly patient with background of malignancy in preoperative work-up.
CASE PRESENTATION
This is a known case, of a 60-year-old Saudi male patient, of non-small cell carcinoma of the left lung, status post left upper lobectomy in 2015 followed by adjuvant chemotherapy. Since then, the patient was healthy and asymptomatic on regular follow-ups.
In 2019, during his surveillance visit, he underwent computer tomography (CT) of the abdomen, which showed incidental finding of distended appendix (Fig. 1) with subtle wall thickening suggestive of mucinous appendix. Colonoscopy examination showed small mass at the appendix with scattered colonic diverticulosis; no biopsy was taken.
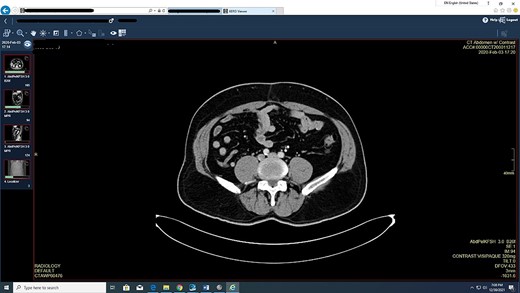
Appendix slightly enlarged especially at the base measuring 11 mm with dilated tip measures 7 mm, but no evidence of adjacent inflammatory stranding or abnormal fluid collection.
Case was discussed in multi-disciplinary teams meeting and planned for laparoscopic appendectomy, which was performed in January 2021. Intraoperative finding was remarkable for chronic inflamed appendix with no signs of mucinous or masses. Post-operation pathology reported as appendiceal diverticulosis, negative for malignancy (Fig. 2).
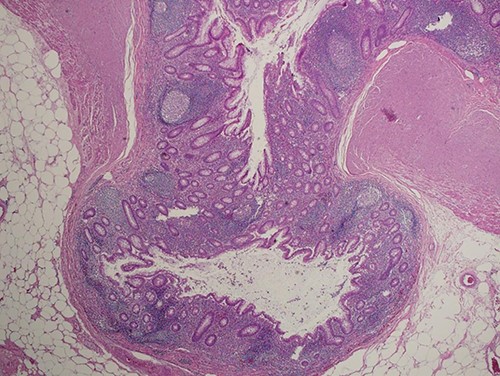
Section shows herniation of mucosa and muscularis mucosa through wall of the appendix without inflammation or dysplastic changes (hematoxylin and eosin, ×100).
DISCUSSION
Appendix diverticulosis can be congenital or acquired, true or pseudo-diverticula based on its protrusion through the mucosal layers and can be differ in pathological types: Type 1 is diverticulitis with a normal appendix; Type 2 is diverticulitis with appendicitis; Type 3 is a non-inflamed diverticulum with associated appendicitis and lastly; Type 4 is a non-inflamed diverticulum with a normal appendix, as in our case [4]. The etiology of the AD is not clear, but several studies revealed some factors in developing AD as: male gender, elder age group and some diseases as cystic fibrosis and Hirschprung’s disorder [5].
The association between AD and epithelial neoplasm is well established as one of the major complications of the diverticula, Lim et al [6] published a recent systematic review which found 26.9% neoplastic changes within the AD specimens, 50% were low-grade mucinous neoplasm. Appendicular mucocele is a wide terminology, which is a morphological description of lumen filled with mucinous fluid that can be either benign in nature or malignant.
Benign mucocele could be resulted from either hyperplasia of the appendiceal mucosal layer or simple enlarged cyst due to lumen obstruction by stricture or fecalith material and their diameter usually <2 cm. In contrast to the malignant mucocele which caused by neoplastic changes as in: mucinous cystadenomas and mucinous cystadenocarcinomas that more likely to be larger in diameter with high risk of rupture in case they exceed 6 cm [7].
In reference to Peritoneal Surface Oncology Group (PSOG), mucinous appendicular neoplasm (MAN) is graded into: adenoma, low-grade appendiceal mucinous neoplasms, high-grade appendiceal mucinous neoplasms, and mucinous adenocarcinoma is based on: cryptologic grade (low or high), tumor cellularity, presence of signet ring cells and elements of invasion [8].
Appendicular mucocele most likely to be in elderly women with variable presentations, which differ from AD that tends to be asymptomatic in male patient unless they present with inflammatory changes [9]. Images might help in the differentiation between AD and MAN; the classical CT abdomen finding of AD is: appendiceal diverticulum with hyperdense pericaecal fat [2] compared with a thin capsulated cystic mass in the right lower quadrant with low attenuation and wall calcification for MAN [10]. Colonoscopy also has some ability in identifying appendicular mucocele if the appendiceal orifice is seen at the center of the mound, which is known as ‘Volcano sign’ [11].
The revolution in the management of appendicular diseases has been toward less invasion. Mucocele has been more detailed in the resection plan depends on the presence of neoplastic changes, PSOG type and perforation during the operation. Appendectomy is still the ideal treatment for both symptomatic and asymptomatic AD as it can be done in emergency sitting in case of diagnosis uncertainty as in AA or electively for prophylactic measure if diagnosed incidentally [12]. For the mucocele, Abreu Filho et al. [13] proposed in 2011 a surgical algorithm summarized as: appendectomy with excision of the mesoappendix and surrounding lymph nodes if the base was not involved by 2 cm, if the base was part of the mass, then a frozen section is advised to rule out malignancy as the later indicates formal oncological resection of the right colon. It’s crucial to maintain the mucocele wall integrity during the resection to avoid developing pseudomyxoma peritonei, which is a devastating complication of ruptured malignant mucocele [8].
The overall prognosis of the AD and appendicular mucocele is related to the pathological report post resection; for simple mucocele, non-neoplastic mucocele, cystadenoma and non-invading cystadenocarcinoma they have excellent 5-year survival year reaching >90% [14].
CONCLUSION
The differentiation between the AD and appendicular mucocele is not fully amiable prior confirmation with pathology due to the similarity in the clinical presentation, physical examination and different modalities of investigations. We recommend resection of both mentioned findings once suspected as they carry high risk of complications including: perforation and neoplastic transformation, especially in patients with history of malignancy.



