-
PDF
- Split View
-
Views
-
Cite
Cite
Anzel Jansen van Rensburg, Kasra Raufian, A case report of ectopic pancreatic tissue in the gallbladder, Journal of Surgical Case Reports, Volume 2022, Issue 3, March 2022, rjac098, https://doi.org/10.1093/jscr/rjac098
Close - Share Icon Share
Abstract
Heterotropic pancreatic tissue is a rare entity where aberrant pancreatic tissue is located without any anatomical connection to the pancreas. It is usually reported to be found in stomach, duodenum, jejunum and spleen. Rare locations include lung, mediastinum, liver, mesentery, ileum, meckels diverticulum and gallbladder [1, 2]. This anomaly is often an incidental finding during laparotomy or autopsy. We describe a case of an elective laparoscopic cholecystectomy with the histology of the gallbladder showing focal ectopic pancreatic acinar tissue.
INTRODUCTION
Heterotropic pancreatic tissue is a rare entity. It refers to aberrant pancreatic tissue located without anatomical or vascular connection to the pancreas. The tissue can be found in the stomach, duodenim, jejunum and spleen. Rare locations include lung mediastinum, liver, mesentery, ileum, meckels diverticulum and gallbladder [1, 2]. Most patients are asymptomatic, and this is an incidental finding at time of histological examination. The incidence in the literature varies from 0.55% to 13.7% at autopsy and the incidence during surgery is reported to be 0.2% [3, 4]. Malignant transformation of this tissue is very rare, however, it is an important entity for pathologist to be aware of to ensure no sinister pathology is present once found.
CASE REPORT
A 31-year-old female was referred to the outpatient department with biliary colic. She reported symptoms of right upper quadrant pain, fevers and vomiting for a week 3 months prior to her review. At the time of the pain, she presented to the emergency department and was discharged after her symptoms settled. Her General Practitioner completed an ultrasound scan which demonstrated a 6 mm stone impacted in the gallbladder neck and a 7 mm gallbladder wall with mild intrahepatic biliary dilatation. She was also noted to have a mass in segment 7 of the liver which a computer tomography (CT) scan revealed to be a cavernous haemangioma. Her blood tests showed a bilirubin of 20, ALP 61, GGT 12, ALT 20, AST 15. She reported symptoms of intermittent RUQ pain following fatty meals for the weeks following this first severe episode. Her background included a previous peptic ulcer at age 17 and a caesarean section. She did not take any regular medication and was a non-smoker.
She proceeded to an elective laparoscopic cholecystectomy. At the time of her procedure, she was found to have features suggestive of chronic cholecystitis with peritoneal adhesions. Her procedure was straightforward and intraoperative cholangiogram showed a spiral cystic duct with the trifurcation of intrahepatic ducts. Her common bile duct appeared mildly dilated however tapered at the lower end and showed filling of the duodenum with no filling defects. The histology from the gallbladder showed variable fibromuscular thickening of the wall with intramural cystic Rokitansky-Aschoff sinuses, but no significant inflammation. Focal ectopic pancreatic acinar tissue (1 mm) within the gallbladder was found (Figs 1–3). There was no evidence of intestinal metaplasia, dysplasia or malignancy.
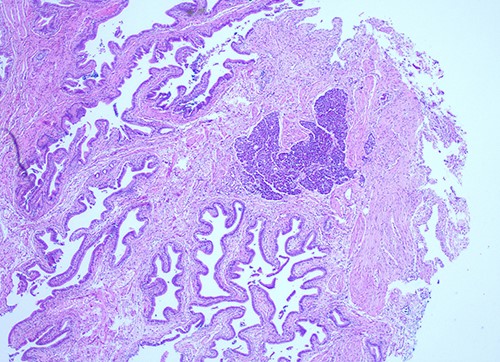
Histological examination of gallbladder ×20 showing island of ectopic pancreatic tissue adjacent to the mucosa of the gallbladder neck.
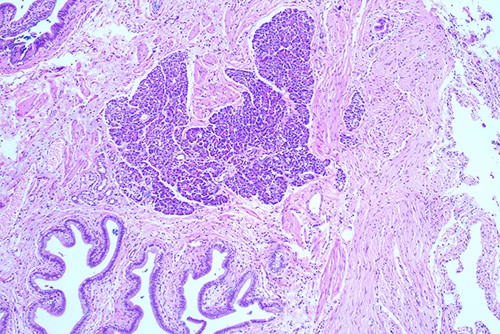
Histological examination of gallbladder ×40 showing island of ectopic pancreatic tissue adjacent to the mucosa of the gallbladder neck.

Histological examination ×100 showing ectopic tissue consisting of pancreatic acini and small ducts. No islets are seen.
This was an elective case, and the patient was discharged the same day.
DISCUSSION
Heterotropic pancreas has been described in the stomach, duodenum, jejunum and spleen. Rare locations include lung, mediastinum, liver, mesentery, ileum, meckels diverticulum and gallbladder [1, 2]. The exact origin of heterotropic pancreas has not been established and theories exist in the literature. The hypothesis most widely accepted is that this occurs during the rotation of the gastrointestinal tract. The developing pancreases has areas of tissue that become separated from the main body of the pancreas [1, 5]. In the literature <40 cases have been described [6]. Jean Schultz first described heterotropic pancreas in the 18th century, however, the first classification was made by Heinrich et al. This was later modified by Fuentes in 1973 which included four types [7]:
i) Type 1—Resembles the normal pancreatic tissue with the presence of ducts, acini and endocrine islets.
ii) Type 2—Canalicular variant with pancreatic ducts.
iii) Type 3—Exocrine pancreas only.
iv) Type 4—Endocrine pancreas only.
Macroscopically these ectopic pieces of tissue can appear as a nodule or polyp, however, having pancreatic tissue in the gallbladder is a very rare entity [2]. These lesions can measure between a few millimetres to 4 cm. Heterotropic pancreatic tissue can be found in any age group, however, appear to be more common in patients between 40 and 60 years of age [3]. The literature does appear to report a slightly higher prevalence in females, although this may be related to females having higher cholelithiasis related cholecystectomies [7].
Most presentations are asymptomatic and normally this is only discovered histologically. However, in some instances it can be symptomatic depending on the location. Symptoms can include jaundice if causing obstruction in bile ducts or biliary colic like symptoms [1, 8].
Although heterotropic pancreatic tissue is often an incidental finding, it does still have the potential to develop complication including malignant transformation, pancreatitis, cyst formation and calcification [1–3].
Preoperative diagnosis using ultrasound or CT is not often helpful in identifying heterotropic pancreatic tissue and is therefore only diagnosed by pathologist on histological examination. Although malignant transformation of this tissue is rare, it is important for pathologist to be aware of this presentation to ensure careful examination for sinister findings.



