-
PDF
- Split View
-
Views
-
Cite
Cite
Tayseer M Shamaa, Ahmed Elsabbagh, Atsushi Yoshida, Shunji Nagai, Joe H Patton, Marwan Abouljoud, Small bowel obstruction due to Roux-en-Y enterolith 13 years following deceased donor liver transplantation: a case report, Journal of Surgical Case Reports, Volume 2022, Issue 3, March 2022, rjac090, https://doi.org/10.1093/jscr/rjac090
Close - Share Icon Share
Abstract
Primary sclerosing cholangitis (PSC) is a progressive, cholestatic liver disease, and liver transplantation (LT) is considered the only therapeutic option for patients with end-stage liver disease secondary to PSC. Intestinal obstruction in adults after LT surgery is a rare complication with diverse clinical presentations. The most common etiology is intestinal adhesions, but this can also result from other rare causes such as enterolith. We describe the first case report of small bowel obstruction secondary to biliary stone formation in the common limb of Roux-en-Y hepaticojejunostomy 13 years after the deceased donor LT. The patient failed initial conservative management and developed peritonitis, requiring urgent surgical exploration to remove the enterolith and resect the involved small bowel. In conclusion, small bowel obstructions due to enteroliths are unusual clinical complications following LT, which require a high degree of suspicion in patients who develop a bowel obstruction in the setting of a previous hepaticojejunostomy.
INTRODUCTION
Primary sclerosing cholangitis (PSC) is a progressive, cholestatic liver disease with unknown cause and unclear pathogenesis [1]. Liver transplantation (LT) is considered as the only therapeutic option for patients with end-stage liver disease secondary to PSC [1]. Biliary complications lead to a significant amount of morbidity after LT [2]. According to the literature, patients who undergo LT for PSC are more predisposed to biliary complications, with strictures occurring in up to 16% of patients in a large series [3]. Intestinal obstruction in adults after liver transplant surgery is a rare complication with diverse clinical presentations. The most common etiology is due to intestinal adhesions, but various other rare causes of intestinal obstruction include intussusception, neoplasms and internal hernias [4]. One potential consequence of biliary stricture following liver transplant is biliary stone formation upstream [2]. Enterolith- or biliary stone-induced small bowel obstruction is a rare complication of living-donor LT, and only a few case reports been published to date [5–7]. This is the first case report to our knowledge of small bowel obstruction secondary to biliary stone formation in the common limb of Roux-en-Y hepaticojejunostomy 13 years after the deceased donor liver transplant.
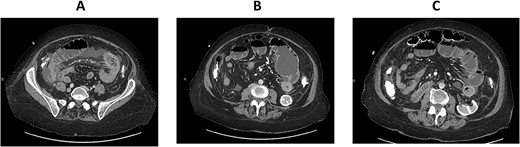
CT enterography: axial views demonstrating dilatation of the bowel loops in the left lower quadrant associated with bowel thickening and collapsed small bowel loops distally.
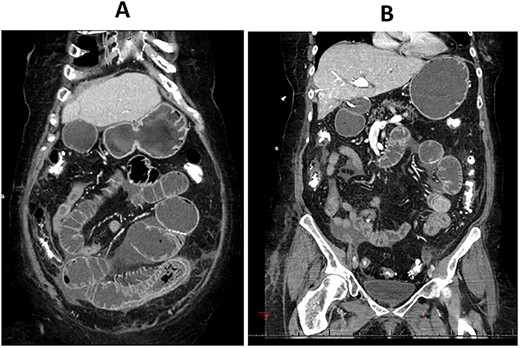
CT enterography: coronal views demonstrating dilatation of the bowel loops in the left lower quadrant associated with bowel thickening and collapsed small bowel loops distally.
CASE DESCRIPTION
The patient is a 71-year-old white female with a past medical history of PSC who underwent orthotopic deceased donor liver transplant in 2006 with a Roux-en-Y hepaticojejunostomy biliary anastomosis. Cholecystectomy was performed to the donor liver. Her course has been complicated over the years by recurrent cholangitis requiring a permanent percutaneous biliary drainage tube. The patient had a liver biopsy in 2011 which showed recurrent PSC, but the patient refused any further liver transplants. Her daily immunosuppressive regimen consisted of cyclosporine 25 mg. Thirteen years after the deceased donor liver transplant, the patient presented to our emergency department with abdominal pain for a week which was associated with abdominal distention and nausea. Her liver function tests and complete blood count were normal on admission. Computed tomography (CT) scan of her abdomen and pelvis with intravenous contrast demonstrated focal dilatation of proximal jejunal bowel loop at the site of anastomosis with air-fluid/debris level (Supplementary Figure 1). She was admitted to the hospital and was initially managed conservatively with nasogastric tube suction, bowel rest and intravenous fluid hydration. A small-bowel follow-through study was obtained which revealed contrast within the colon with no radiographic evidence of bowel obstruction. The patient’s clinical condition improved on her second day after admission and a trial of diet was performed, but the patient had worsening symptoms and subsequently developed peritonitis on her fourth hospital day. CT enterography was obtained which revealed dilatation of the proximal small bowel loops proximal to the small bowel anastomosis in the left mid-abdomen with mild wall thickening of the small bowel in the left lower quadrant without definitive obstructing cause or evidence of pneumatosis (Figs 1A–C and 2A,B). The patient was taken emergently to the operating room for an exploratory laparotomy. The jejunojejunostomy was intact and dilated with dilated proximal Roux limb. Approximately, 50 cm distal to the jejunojejunostomy in the common limb, a firm, round mass was palpated in a segment of bowel which was very edematous, friable, inflamed, with a focus of necrosis without obvious perforation. The remainder of the small bowel was normal. Given the state of the small bowel with the focus of necrosis, the decision was made to perform a small bowel resection with a hand-sewn anastomosis. The resected small bowel was opened off the field, and an impacted bezoar was found with small circular yellowish objects thought to possibly be gallstones mixed with other fibrous content. The resected small bowel pathology showed focal mucosal ulceration, transmural hemorrhage and acute serositis. The patient had an uneventful post-operative course and was discharged home 7 days after surgery. She was seen in clinic for a follow-up appointment a month after the surgery and was found to be doing great, tolerating her diet and having regular bowel function.
DISCUSSION
Intestinal obstruction in liver transplant recipients is a rare but serious complication. Thirteen cases of intestinal obstruction secondary to enteroliths following small bowel surgery have been described in a recent case series [7]. There has been one previously reported case in the literature of enterolith formation causing bowel obstruction following living-donor liver transplant in adults [8] and one in children [9]. To our knowledge, late small bowel obstructions due to an enterolith following a deceased donor liver transplant have not been previously reported.
Biliary stones, sludging and casts can develop late after transplantation most commonly manifest as cholangitis [10]. In our case, the stone was likely formed proximally in either the efferent jejunal loop or intrahepatic ducts because of pre-existing enterobiliary strictures. The two critical components that predispose to the formation of enteroliths include mechanical factors, such as bowel hypomobility and stasis, and chemical factors, such as acidic conditions [11]. Manometric studies have shown delayed transit time in patients with Roux-en-Y hepaticojejunostomy compared to healthy controls, which can result in bacterial overgrowth which accelerates bile salt deconjugation [12]. Cyclosporin has also been reported to be associated with biliary stone formation by enhancing small bowel bacterial overgrowth, resulting in deconjugation of bile acids and in the formation of an enterolith [13]. In our case, the patient was on daily cyclosporine for immunosuppression and developed recurrent cholangitis because of recurrence of her PSC based on repeat liver biopsies. These all placed her at a higher risk for developing enterolithiasis.
Several different modalities exist for the management of obstruction of the Roux limb by an enterolith, including minimally invasive approaches for enterolith removal [14]. Surgical treatment remains the gold standard by milking and removal of the enterolith through an enterotomy laparoscopically or with an open laparotomy [15]. In our case, the patient developed peritonitis, eliminating the ability to utilize any endoscopic tools for enterolith extraction.
In conclusion, small bowel obstructions due to enteroliths are unusual clinical complications following LT, which require a high degree of suspicion in patients who develop a bowel obstruction in the setting of a previous hepaticojejunostomy.
CONFLICT OF INTEREST STATEMENT
The authors have no relevant financial disclosures related to this manuscript.
FUNDING
There was no funding received for conducting this study and the preparation of the manuscript.
References
Khalaf H, Al-Suhaibani H, Al-Mehaidib A, Shabib S, Bhuiyan J, Khuroo MS, et al.
Quillin RC 3rd, Bongu A, Kasper V, Vittorio JM, Martinez M, Lobritto SJ, et al.
Duron JJ, Silva NJ, du Montcel ST, Berger A, Muscari F, Hennet H, et al.
Cao S, Cox K, So SS, Berquist W, Lee SP, Haigh WG, et al.
Yamamoto H, Sekine Y, Sato Y, Higashizawa T, Miyata T, Lino S, et al.
- small bowel obstruction
- cholestasis
- end stage liver disease
- biliary calculi
- adult
- roux-en-y anastomosis
- sclerosing cholangitis
- limb
- intestinal obstruction
- intestine, small
- liver transplantation
- peritonitis
- surgical procedures, operative
- surgery specialty
- intestinal adhesions
- hepaticojejunostomy
- gastric bypass, roux-en-y
- roux-en-y hepaticojejunostomy
- causality
- donors
- deceased donor liver transplantation



