-
PDF
- Split View
-
Views
-
Cite
Cite
Emerson Leonardo Monteiro, Julian Ramin Andresen, Johannes Schmid, Hans Jörg Mischinger, Peter Kornprat, A rare case of internal hernia through the foramen of Winslow, Journal of Surgical Case Reports, Volume 2022, Issue 3, March 2022, rjac065, https://doi.org/10.1093/jscr/rjac065
Close - Share Icon Share
Abstract
Internal hernia is a rare cause of intestinal obstruction. The risk of internal herniation is higher in some patients after abdominal surgery or with certain anatomical anomalies. Here, we present a case of an 80-year-old patient with incarcerated internal hernia through the foramen of Winslow due to an anatomical abnormality.
INTRODUCTION
An internal hernia is the protrusion of tissue into congenital or acquired openings in the abdominal cavity. Internal hernias cause 4% of mechanical intestinal obstructions. The most frequent types of internal hernias are paraduodenal hernias, ileocecal hernias, hernias through the foramen of Winslow, mesosigmoid hernia, mesenteric defects, broad ligament hernia, supravesical hernia and post-operative hernias [1]. Bowel obstruction caused by entrapment of the intestine in the lesser sac through the foramen of Winslow represents 8% of internal hernias, with a mortality of up to 49% with late therapy [2].
CASE REPORT
An 80-year-old patient was referred to the surgical emergency room from the internal emergency department for further therapy of abdominal pain, where the patient presented with constipation for 10 days and brownish coffee-grounds-like vomiting. At the time of presentation at the Surgical Emergency Department, the patient was already somnolent and hypotonic with a blood pressure of 90/50 mmHg, which is why further collecting of medical history was not possible. The patient was flinching during palpatory examination of the abdomen and showed signs of involuntary abdominal guarding. The laboratory blood tests at admission showed increased lactate (4.0 mmol/l) and increased inflammatory parameters such as leukocytes (50.04 · 109/l) and CRP (205.8 mg/l). The computed tomography (CT) showed a closed loop obstruction due to an internal herniation of the terminal ileum, cecum and ascending colon through the omental foramen into the lesser sac with signs of ischemic bowel injury (Fig. 1, Supplementary Video 1). The hepatoduodenal ligament was ventrally displaced with slit-like compression of the portal vein and dilation of the common bile duct. The proximal ileum loops were dilated, the downstream colon was collapsed. The clinical condition of the patient demanded an immediate transfer to the operating room. In general anesthesia, a median laparotomy was performed. After opening of the peritoneal cavity, a large hernia in the lesser sac was seen in the area of the foramen of Winslow (Fig. 2). The incarcerated right hemi-colon and about 2 m of small intestine was already necrotic due to long-term vascular occlusion. During the attempt to release the incarcerated intestines, bowel perforation occurred due to the fragility of the necrotic intestinal wall, and the intestinal content leaked to the abdominal cavity. After diligent abdominal washout procedure, a right-sided hemicolectomy and ileum partial resection with a side-to-side ileocolic anastomosis was performed. The post-operative course was without surgical complications. The patient aspirated during the initiation of anesthesia and developed pneumonia post-operatively, which needed antibiotic therapy with CPAP ventilation in the intensive care unit. This caused a transient delirious state of the patient. After psychiatric therapy adjustment and continuation of antibiotic treatment the patient’s condition improved so that the patient could be transferred to the normal ward and later on could be discharged to home care.
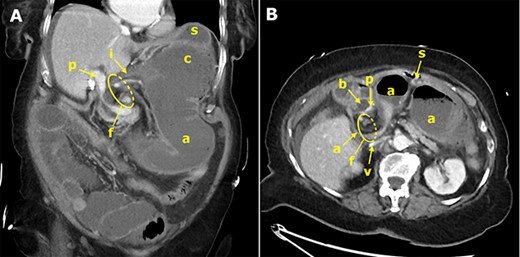
Contrast-enhanced CT of the abdomen; the coronal slice (A) demonstrates the terminal ileum (i), dilated cecum (c) and ascending colon (a), which are abnormally positioned upside down in the lesser sac, herniated through the omental foramen (f); the portal vein (p) is compressed; the stomach (s) is displaced ventrally and cranially; the axial slice (B) shows the ascending colon (a) exiting the hernial orifice (f), which is located between the ventrally displaced common bile duct (b) and the inferior vena cava (v).

DISCUSSION
Our case vividly illustrates the rare internal hernia through the foramen of Winslow with the typical consequences of closed loop obstruction with intestinal necrosis. It highlights the non-specific clinical presentation and underlines the importance of preoperative CT diagnostics and rapid acute surgical care. Foramen of Winslow is an entrance into the omental bursa that is bounded ventral by hepatoduodenal ligament, dorsal by inferior vena cava, cranial by caudate lobe of liver and caudal by duodenum. Herniation into the lesser sac by the foramen Winslow is more common in patients with anatomical abnormalities such as (i) abnormally large foramen of Winslow, (ii) presence of an extremely long thin intestine mesentery or persistence of ascendent mesocolon, (iii) an elongated right liver lobe that could direct the movable intestinal loop into the foramen, (iv) a lack of fusion between the ascending cecum or ascendent colon and the parietal peritoneum, (v) malformation of the hepatogastric ligament l and (vi) incomplete intestinal rotation or malrotation [3]. In this case, a lack of fixation of the right hemi-colon on the parietal peritoneum led to the hernia. This predisposes to herniation of the cecum and ascending colon, as described in some previous case reports [3–7]. Similarly, isolated parts of the small intestine [8, 9] or parts of the transverse colon [10] can also herniate into the foramen of Winslow. An early diagnosis is crucial for prognosis. Despite very rapid management with only a few hours between presentation and surgery, intestinal necrosis occurred due to the late presentation of our patient.
CONCLUSION
Although internal hernia is not the most common cause of bowel obstruction, the possibility should always be considered, especially in patients after certain operations, such as Petersen hernia after gastric bypass surgery [11], or in patients with anatomical predispositions (as described in our case report). Internal herniation is frequently accompanied by vascular occlusion of the pinched section of the intestine, causing bowel necrosis and subsequent perforation with peritonitis, which is why rapid surgical management is crucial.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



