-
PDF
- Split View
-
Views
-
Cite
Cite
Kyle Smiley, David A Partrick, Kristine S Corkum, S Christopher Derderian, Torsed ectopic intra-abdominal liver rest within an adolescent female, Journal of Surgical Case Reports, Volume 2022, Issue 2, February 2022, rjac036, https://doi.org/10.1093/jscr/rjac036
Close - Share Icon Share
Abstract
Extrahepatic liver (EL) rests are rare, with a reported annual incidence of 0.24–0.47. While reports often note EL incidentally found on pathologic specimens of aberrant tissue, there has been a case report of hepatocellular carcinoma arising from one of these rests, highlighting the importance of surgical resection. EL has been reported to cause symptoms such as abdominal pain, intraperitoneal bleeding and compression of adjacent organs. Most commonly, it has been identified in the gallbladder, likely due to proximity of the gallbladder to the native liver. The paucity of diagnostic tests makes the preoperative diagnosis challenging. We present a case of a 12-year-old female presenting with severe epigastric pain secondary to incapsulated EL tissue attached to the stomach via a narrow stalk. By describing this case, we hope to improve the diagnosis and management of abdominal masses with unclear etiology.
INTRODUCTION
Extrahepatic liver (EL) rests are rare, with a reported annual incidence of 0.24–0.47 [1]. They have been confirmed pathologically in both intra- and extra-abdominal sites, with the gallbladder being the most common [2, 3]. While reports often note EL incidentally found on pathologic specimens of aberrant tissue, there has been a case report of hepatocellular carcinoma arising from one of these rests, highlighting the importance of surgical resection [4].
While EL may be discovered incidentally during a surgical procedure, it has been reported to cause symptoms such as abdominal pain, intraperitoneal bleeding and compression of adjacent organs [5]. We present a case of a 12-year-old female presenting with severe epigastric pain secondary to incapsulated EL tissue attached to the stomach via a narrow stalk. To the best of our knowledge, there are no documented cases matching this description in the literature. Previous reports of EL have been identified by pathology after resection or during autopsy [1–6].
CASE PRESENTATION
A 12-year-old female with no significant past medical history presented to her pediatrician with 1 week of severe intermittent epigastric pain and occasional bilious emesis. Neither acetaminophen nor a gastrointestinal cocktail abated these symptoms.
An abdominal ultrasound (US) demonstrated a peripancreatic cystic mass with internal debris located between the stomach and pancreas (Fig. 1). The differential diagnosis at that time included a foregut duplication cyst, an infradiaphragmatic sequestration and a pancreatic cystic lesion. Given the unclear origin of this lesion, an abdominal magnetic resonance imaging (MRI) was obtained, which identified a T1 hypointense and T2 hyperintense rim enhancing 4.3-cm mass with surrounding edema and adjacent peripancreatic inflammation (Fig. 2).

Initial abdominal US; abdominal US demonstrating hypoechoic, peri-pancreatic mass between stomach and pancreas (white box).
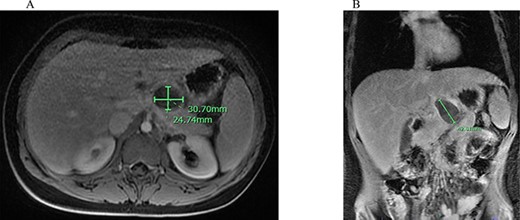
Abdominal MRI of suspicious mass; (A) axial abdominal MRI revealing 3.07 × 2.74 cm mass (green bars) posterior to the L. lobe of the liver and medial to the stomach; (B) coronal abdominal MRI demonstrating 4.26 cm mass (green bar) inferior to the liver and superior to the pancreas with peripancreatic inflammation.
Although the diagnosis remained unclear, her symptoms persisted during the workup; thus, we elected to take her to the operating room for a laparoscopic resection. During the procedure, a 4.5-cm firm, incapsulated mass was identified inferior to the left lobe of the liver, with the stalk originating from the lesser curvature of the stomach. The mass was mobilized, the stalk was stapled with an Endo GIA stapler (Medtronics, Minneapolis, MN) and removed within an Endocatch bag (Medtronics) via a 12-mm laparoscopic port.
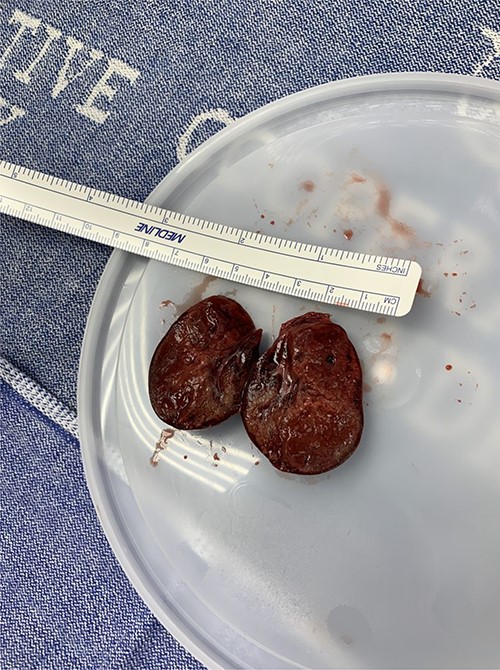
Pathological evaluation revealed infarcted heterotopic liver parenchyma, which was consistent with a torsed liver rest (Fig. 3). The patient was discharged on post-operative day 1, and at her follow-up appointment 1 month later, she was asymptomatic.
DISCUSSION
EL parenchyma is a rare diagnosis often incidentally found on a pathologic specimen. As of this writing, <100 unique cases have been published in the English literature. We present a case in which a 12-year-old child presents with epigastric pain, presumed to be secondary to intermittent torsion of EL rest, who experienced resolution of symptoms after resection. Workup included abdominal US and MRI.
Liver parenchyma appears homogenous with echogenicity similar to renal cortex and native liver on abdominal US. As an adjunct to US, liver-sequenced MRI can delineate anatomy, vascular supply and intrahepatic pathology. Healthy liver appears uniform, with T1 hypointense and T2 hyperintense signals on MRI [7]. The presence of tissue with these characteristic findings is not diagnostic for EL but may provide some preoperative insight, as was the scenario in this case. The US we obtained was non-diagnostic. Given the broad differential, we obtained an MRI that demonstrated a well-circumscribed T2 hyperintense lesion, which was consistent with an EL rest.
Histological evaluation of EL tissue generally reveals normal liver parenchyma consisting of lobules and central veins [8]. We considered endoscopic biopsy but given the severity of her symptoms, we elected to proceed with surgical resection without further workup. Moreover, biopsy risks hemorrhage and potentially malignancy seeding [9].
Ectopic liver tissue has been described in several organs [1–6]. Most commonly, it has been identified in the gallbladder, likely due to proximity of the gallbladder to the native liver [9]. It has been theorized that EL is derived from aberrant hepatic tissue migration from a foregut diverticulum during embryological development [8]. It is important for surgeons to be aware of this rare entity as it has historically been difficult to diagnosis until resection and subsequent pathological examination.
In general, EL tissue should be excised due to the increased risk of hemorrhage, pain and transformation to hepatocellular carcinoma [5]. Surgical excision is the only documented treatment modality. Alternative treatments, such as arterial embolization and pharmacologic management, have not been described. When possible, laparoscopic resection should be attempted to decrease length of hospital stay and reduce complications [10]. When completely resected, prognosis is excellent with no documented recurrence in the literature.
CONCLUSION
EL remains a rare diagnosis. The paucity of diagnostic tests makes the preoperative diagnosis challenging. Although most commonly found within other organs, our report demonstrates that EL rests can occur as independent, encapsulated masses. By describing this case, we hope to improve diagnosis and management of abdominal masses with unclear etiology.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
The authors have no financial disclosures to make.



