-
PDF
- Split View
-
Views
-
Cite
Cite
Shunsuke Yamagishi, Osamu Aramaki, Nao Yoshida, Yusuke Mitsuka, Takaharu Kawai, Shintaro Yamazaki, Woodae Kang, Hisashi Nakayama, Masamichi Moriguchi, Tokio Higaki, Mitsugu Kochi, Yukiyasu Okamura, Laparoscopic-assisted modified Kugel herniorrhaphy for obturator hernia: a case report, Journal of Surgical Case Reports, Volume 2022, Issue 2, February 2022, rjac035, https://doi.org/10.1093/jscr/rjac035
Close - Share Icon Share
Abstract
Obturator hernia (OH) is a relatively rare disease and there are various surgical procedures for treating it. We report the case of a patient with an OH who underwent laparoscopic-assisted modified Kugel herniorrhaphy. The patient was a 74-year-old woman admitted to our hospital with nausea and abdominal distension. A diagnosis of intestinal obstruction was made because abdominal computed tomography revealed incarcerated right OH. No apparent strangulation findings were observed, and reduction was performed under ultrasound guidance. Laparoscopic-assisted modified Kugel herniorrhaphy for OH was performed. There were no signs of the bowel necrosis. Pneumoperitoneum was temporarily discontinued, and the OH was repaired by the modified Kugel herniorrhaphy. Laparoscopy confirmed that the direct Kugel patch was placed at the appropriate position. Laparoscopic-assisted modified Kugel herniorrhaphy is considered to be safe and useful for patients with OH and is considered as one of the treatment options.
INTRODUCTION
Obturator hernia (OH) is a relatively rare disease, accounting for 0.07–1% of intra-abdominal hernias and is reported to cause 0.2–1.6% of small intestinal ileus. OH is more common in the elderly, thin females, between 70 and 90 years of age, and is often associated with underlying medical conditions [1–4]. OH causes intestinal obstruction associated with bowel incarceration; thus, emergency surgery is often required. There are various surgical procedures for OH; however, no standard surgical procedure has been established. Laparoscopic approaches for OH have been increasingly reported in recent years; however, many patients are often elderly, and their general health condition may limit the use of laparoscopic surgery. Here, we report a case of OH treated using a laparoscopic-assisted modified Kugel herniorrhaphy.
CASE REPORT
The patient was a 74-year-old woman who presented to our institution with nausea and abdominal distension. She had a history of restrictive lung disease, pulmonary hypertension, and appendicitis. Her height was 161 cm and weight 34.4 kg. She had a body mass index of 13.8 kg/m2. Physical examinations revealed abdominal distension and mild tenderness in the lower abdomen but no apparent signs of peritonitis. C-reactive protein was mildly elevated at 1.15 mg/dl, while the other laboratory blood test parameters were normal. An abdominal computed tomography (CT) demonstrated that the small intestine was incarcerated in the right obturator foramen and showed intestinal obstruction. A part of the bladder was impacted in the left OH (Fig. 1). A manual reduction of the incarcerated right OH was performed under ultrasound (US) guidance because there were no apparent necrotic bowel findings. Elective surgery was subsequently performed.

Abdominal CT scan revealed that the small bowel was incarcerated in the right obturator foramen and part of the bladder was impacted in the left obturator foramen.
The patient was placed in the supine position under general anesthesia and the surgery was performed. A 12-mm-sized trocar was inserted into the abdominal cavity through an open incision on the umbilicus, and the intra-abdominal pressure was 6 mmHg. The intra-abdominal pressure was set at a lower pressure than usual. A 5-mm-sized trocar was inserted from the left flank and the head of the patient was lowered. Laparoscopic examination revealed bilateral OH and there was no evidence of ischemia or necrosis in the small intestine. Pneumoperitoneum was temporarily discontinued, and the right OH was repaired by the modified Kugel herniorrhaphy. Laparoscopy confirmed that the direct Kugel patch was placed at the appropriate position. Subsequently, the left OH was repaired similarly (Fig. 2). The operation time was 175 min, pneumoperitoneum time was 15 min and the volume of blood loss was 10 g. The patient recovered without post-operative complications.
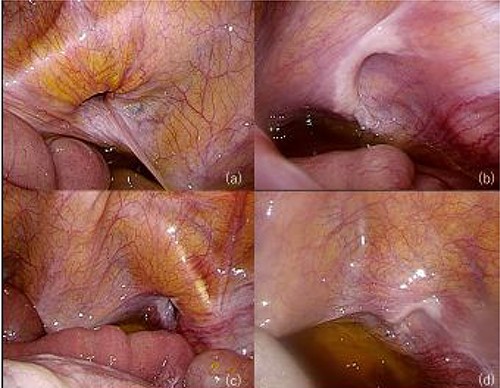
Laparoscopic view of the mesh placement; (a) right OH; (b) after repairing the right OH; (c) left OH; (d) after repairing the left OH.
DISCUSSION AND CONCLUSION
OH is generally diagnosed as intestinal obstruction due to incarcerated intestine and is often an emergency operation. In recent years, when ischemia or perforation of the intestine is not observed in incarcerated OH, the US-guided manual reduction has been reported to be useful for symptom relief and for avoiding emergency surgery [5]. This patient had a history of restrictive lung disease and pulmonary hypertension. If no intestinal necrosis or perforation was observed, it was considered to be safe to avoid emergency surgery and to perform elective surgery after assessing the general condition. Because intestinal necrosis was excluded through several examinations, US-guided manual reduction of incarcerated OH was performed.
Surgical procedures for this condition include open, laparoscopic (transabdominal preperitoneal and totally extraperitoneal) and inguinal approaches [6–8], which have not yet been standardized. Laparoscopic surgery has been increasingly reported recently. The advantages of laparoscopic surgery include (i) ease of observing the abdominal cavity and the intestinal tract and (ii) feasibility of observing the obturator foramen, contralateral side and presence or absence of other hernial complications. Compared to open surgery, laparoscopic surgery is less invasive, has fewer post-operative complications and requires a shorter hospital stay [5]. The inguinal method has the advantages of not requiring pneumoperitoneum, shorter operation time than laparoscopic surgery and a general procedure. This patient had a history of restrictive lung disease and pulmonary hypertension. Therefore, we avoided long pneumoperitoneum and surgery time in this patient by performing laparoscopy within the shortest possible time with low intra-abdominal pressure to verify the intestine and the obturator foramen. Subsequently, OH repair was performed using the modified Kugel herniorrhaphy, and laparoscopy confirmed that the direct Kugel patch was placed at the appropriate position.
The methods of closure of hernia orifices include (i) simple suture of the obturator peritoneum; (ii) suturing adjacent organs such as the uterus, ovaries and omentum to the hernia orifice; (iii) direct suturing of the periosteum and obturator of the suprapubic; and (iv) mesh repair. For untreated hernial sacs, recurrence is reported in 10% of cases [7, 9, 10].
OH is a relatively rare disease, and even experienced surgeons may not have much expertise on this. OH is often operated on urgently; thus, each hospital needs to be familiar with this pathology and repair procedures. In selecting the surgical procedure, emphasis was placed on (i) observation of the hernia (contralateral, accompanied by other hernias), (ii) observation of the intestinal tract, (iii) post-operative recurrence, (iv) mesh infection and (v) generality.
This procedure adds the benefits of a laparoscope to the general inguinal approach and is thought to be able to observe hernias and intestinal tracts from the abdominal cavity, identify the location of the mesh and reduce recurrence. If intestinal necrosis is observed, it can be removed with a small-incision laparotomy, and the risk of mesh infection can be reduced by placing the mesh from outside the peritoneum. In addition, the modified Kugel herniorrhaphy is a common method and may be possible during emergencies.
This procedure is considered to be safe and useful for patients with OH and is considered as one of the treatment options.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
CONSENT FOR PUBLICATION
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.



