-
PDF
- Split View
-
Views
-
Cite
Cite
Suresh Ujjal, Rasmus Kroijer, A rare case of a herniated acute appendicitis, Journal of Surgical Case Reports, Volume 2022, Issue 2, February 2022, rjac029, https://doi.org/10.1093/jscr/rjac029
Close - Share Icon Share
Abstract
Acute appendicitis (AA) is the most common cause of acute abdomen worldwide and untreated it can lead to abscess formation, purulent or faeculent peritonitis, sepsis and death. This paper presents a rare case of an AA herniated in a retro-psoas muscle defect, which has not previously been reported in the literature. Our patient’s diagnosis and management was delayed due to the unusual presentation. This case emphasizes the importance to utilize AA scoring algorithms to aid decision-making as they have shown to reduce admissions, optimize the use of diagnostic imaging and reduce negative surgical explorations.
INTRODUCTION
Acute appendicitis (AA) is the most common cause of acute abdomen worldwide and untreated it can lead abscess formation, purulent or faeculent peritonitis, sepsis and death [1].
Diagnosis of AA can be challenging due to its anatomy. The attachment of the base of the appendix to the caecum is fixed, whereas the position of the head of the appendix, although often in the retro-caecal position, is variable [2, 3]. This can lead to patients presenting with differing signs and symptoms than those of classic appendicitis, reflecting the anatomical position of the appendix, causing a potential delay in diagnosis and management.
We describe a rare case of an AA herniated in a retro-psoas muscle defect, which has not previously been reported in the literature.
CASE REPORT
A 48-year-old male, under investigation for chronic fatigue and with no previous surgical history, presented to the Emergency Department with a 1 day history of fever (38.5°C), nausea, vomiting and non-specific abdominal pain, which was described as sudden onset and localized bilaterally to the flanks and to the lower abdomen.
Laboratory tests revealed elevated white blood cells (15.9 × 10/9 L) with a normal C-reactive protein. Urine dipstick was negative for blood. The patient responded well to paracetamol and was discharged pain free the same day by the medical team, after a period of observation with the suspicion of gastroenteritis. The patient was contacted the next day, as blood cultures were positive for streptococcus constellatus. The patient reported that he remained febrile and the abdominal pain had worsened and was now localized to the right side of the abdomen.
The patient was re-admitted and examination revealed a soft abdomen with localized rebound tenderness in the right iliac fossa. A computed tomography (CT) abdomen was requested and a referral made to the surgical team. The CT scan illustrated AA with the appendix located posterior to the ileo-psoas muscle (Figs 1–3). A diagnostic laparoscopy was performed, which revealed the head of the inflamed appendix herniated posterior to the psoas muscle in a cavity, (~25 mm deep and 10 mm in diameter) that could not be dissected laparoscopically (Fig. 2). Therefore, an uncomplicated open appendectomy was performed and the patient was admitted for post-operative observation. Recovery was uneventful and the patient was discharged without follow-up.

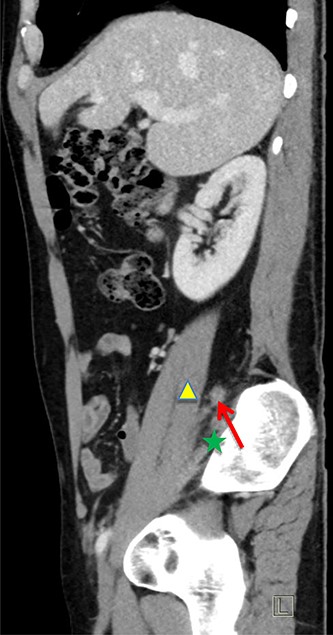
Sagittal CT image. Inflamed appendix (red arrow) positioned between psoas (yellow triangle) and iliacus muscles (green star).
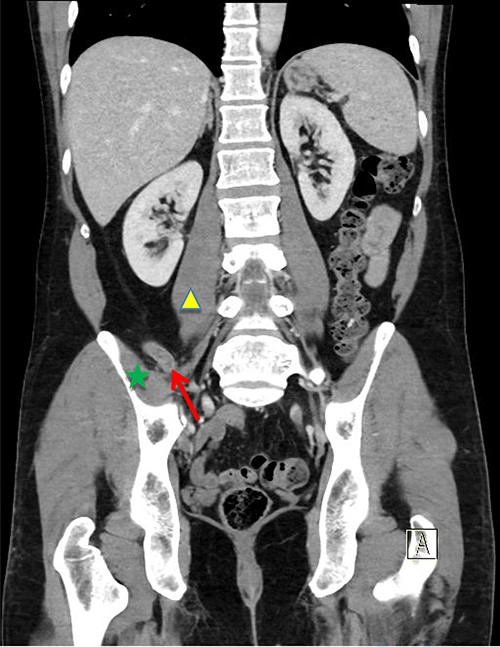
Coronal CT image. Inflamed appendix (red arrow) positioned between psoas (yellow triangle) and iliacus muscles (green star).
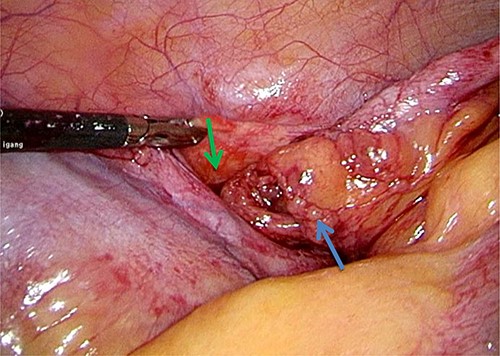
Laparoscopic image of inflamed appendix (blue arrow) herniated in retro-psoas muscle defect (green arrow).
DISCUSSION
Diagnosing AA can be challenging, as in our patient’s case, due to anatomically different locations of the appendix.
In utero, the caecum is initially located in the sub-hepatic region and migrates caudally into the right iliac fossa as the ascending colon forms. The distal and proximal portions of the caecum develop at different speeds, giving rise to the caecum and appendix, respectively. Therefore, the determining factors for the position of the appendix are embryonic caecal migration and development and appendiceal length [4]. This is further evidenced by documented geographical differences in the location of the appendix [5]. Previous surgeries causing adhesions, body habitus and pregnancy status also play a role [4, 6]. The different locations of the appendix can be categorized using the Gladstone and Wakeley classification: retro-caecal (posterior and superior to the caecum), para-caecal (lateral to the caecum), sub-caecal (inferior to the caecum), pelvic (directed inferiorly into the pelvis over the psoas muscle tip), pre-ileal (anterior and superior to the distal ileum), post-ileal (posterior and superior to the distal ileum) and ectopic (a location that does not meet any of the previous descriptions) [7].
There are several published case reports of ectopic appendixes: lateral pouch, mesocolic, left sided, lumbar, sub-hepatic, intra-caecal, intra-hernia and intra-thoracic. However, this is the first report of an AA herniated in a retro-psoas muscle defect. Rousan et al. published a case report of an appendix in a similar location but this was an incidental finding from a trauma CT of a non-inflammed appendix that did not require any intervention [6].
Due to the unusual location, the patient presented with non-classical symptoms of AA and this led to a delay in diagnosis and management, as there were other diagnoses to rule out, namely urolithiasis and gastroenteritis. Current guidelines from the World Journal of Emergency Surgery recommend using the Adult Appendicitis Score (score ≥ 11, sensitivity 94.7%, specificity 60.2%) or Appendicitis Inflammatory Response (92% sensitivity, 63% specificity) scoring algorithms as clinical predictors of AA. These two scoring systems risk stratify patients and have been shown to reduce admissions, optimize the use of diagnostic imaging and reduce negative surgical explorations [8–10].
A point of possible contention that should be addressed is our decision not to close the retro-psoas muscle defect. This was not performed primarily because of the high risk of infection and abscess formation as it had contained an infected organ and also due to its size, it was judged to be inconsequential. It was assumed the defect would close due to scar formation.
CONCLUSION
Cases of ectopic appendixes are a rare occurrence and therefore we aim to expand the current literature. Moreover it is of utmost importance to be aware of unusual presentations of appendicitis and to utilize scoring systems to avoid delays in diagnosis and treatment, as to prevent complications.
ACKNOWLEDGMENTS
We would like to thank Ivana Jevtic, Senior Registrar in Radiology at the Hospital for Southwest Jutland for providing us with CT images.



