-
PDF
- Split View
-
Views
-
Cite
Cite
Carlos R Arriaza, Edgar Javier Salguero, Andres Cobar Bustamante, Percutaneous CT-guided resection of acetabular osteoid osteoma: a case report, Journal of Surgical Case Reports, Volume 2022, Issue 2, February 2022, rjac019, https://doi.org/10.1093/jscr/rjac019
Close - Share Icon Share
Abstract
Osteoid osteoma located on the hip joint presents with atypical symptoms that can be misdiagnosed or missed. Multiple image studies can be made for diagnosis but OO should be suspected to properly choose the right one. Percutaneous resection with CT guidance is a reproducible and accurate technique with the appropriate tools and a specialist team to obtain optimal results.
INTRODUCTION
Osteoid osteoma (OO) is a small, discrete and benign bone lesion that consist of 10% of all bone tumor [1]. It usually occurs on male patients <25 years [1, 2]. The most common site is metaphysis or diaphysis of femur and tibia, but can be found throughout the body. OO on the pelvic region accounts for 1–3% and 14% are in the acetabulum [3].
The most common symptom is pain at night (80%) [2]. OO on joints may present with atypical symptoms and have been reported on the hip joint with synovitis, joint effusion, decreased range of motion (ROM) and muscle atrophy that can make diagnosis confusing [3].
The treatment of OO can be nonsurgical. Oral nonsteroidal anti-inflammatory drugs (NSAIDS) for prolonged administration relieves pain but take 2–15 years to resolve spontaneously [1–4]. Surgical treatment for acetabular OO include: open surgical with bone block excision, curettage of the lesion or hip arthroscopy depending on the localization of the lesion [1, 5]. A more accurate way to approach the OO is with computed tomography (CT) guidance. A percutaneous technique using a cannulated drilling system, radio frequency (RFA) ablation or chemical destruction of the nidus have advantages over the open technique with fewer complications and high rate success [6, 7].
CASE REPORT
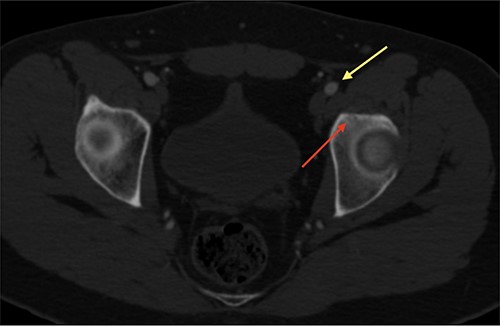
An 18-year-old male with 18 months of left hip pain was referred to an orthopedic surgeon for evaluation. Pain occurred with all hip movements, predominantly at night. Physical examination of the hip showed pain with deep palpation on the groin and positive test for flexion adduction and internal rotation and Patrick test. X-rays were obtained and femoroacetabular impingement (FAI) with labral tear was suspected (Fig. 1). A magnetic resonance imaging (MRI) showed no hip labrum or chondral defect. Measurements for bone deformities of cam and pincer were normal. Physical therapy and nonsteroidal anti-inflammatory drugs were prescribed with some pain relief especially at night. After no improvement of symptoms he was evaluated by a hip surgeon. Intra-articular hip injection with steroids was given and pain disappeared but nocturnal pain recurred after 24 h. Due to the clinical setting and poor response to pain management, an OO was suspected and (CT) was ordered where a 6 mm sclerotic bone tumor with a nidus in the anterior rim of the left acetabulum was identified and corresponded with the pain localization (Fig. 2).


CT scan of the left hip showing a 6-mm extra-articular OO on the anterior rim of the acetabulum (yellow arrow).
The OO was <10 mm and was near the neurovascular structures so percutaneous CT guided curettage was considered the best option.
The procedure was made with general anesthesia and in supine position. A 1-cm incision was made for an anterior approach over the hip joint. Careful blunt dissection was done. Percutaneous technique was used with the guidance of a 64 slice Somatom sensation CT scanner (Siemens AG Munich, Germany) with interval cuts of 2 mm to locate the OO. Intravenous contrast was administered to identify the vascular structures at risk (Fig. 3). A 13G × 100 mm bone marrow biopsy needle was used. Image guidance was performed by a senior radiologist (ES). Once the OO was located, accurate insertion of the needle was monitored, and drilling was done manually to help precision in depth (Fig. 4). Multiple bone fragments were obtained and sampled. Immediate image verification showed a space missing the nidus OO. To avoid leaving remnant nidus, curettage was added on the edges and the deep margin of the tumor. Bone samples were sent to histological evaluation and OO diagnosis was confirmed. Wound pain management was administered for 2 weeks and night symptoms disappeared immediately. Complete relief was achieved 3 weeks later. A 12-month follow-up post treatment reported no recurrence of pain and no complications with wound management. ROM and athletic activities are painless. No soft tissue complications were reported.
CT with intravenous contrast showing the femoral vessel (yellow arrow) before the procedure to obtain proper approach (red arrow showing the OO).
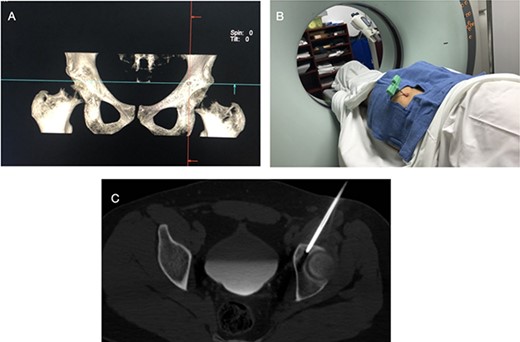
CT showing the precise site for needle insertion (A), CT control of the needle insertion (B,C).
DISCUSSION
OO cases with atypical symptoms may be challenging to diagnose. The average time of diagnosis of a hip joint OO is 6–24 months after pain onset [5]. The most common presenting symptoms were groin pain and are also the most common symptoms in FAI. This overlap of symptoms is the reason hip joint OO is misdiagnosed or missed [3].
Diagnostic imaging is helpful to confirm the right diagnosis. Pelvis X-rays are the initial examination of choice [1, 4]. The oval radiolucency of the nidus may be seen on cortical lesion, but when the OO is located in the bone marrow or areas difficult to assess with X-rays, the lesion is difficult to identify. CT is the recommended study for these cases, and the OO can be located easily with a thin slice scan [1]. It is particularly useful when the nidus is located intra-articular. The MRI for OO detection is controversial. The presence of associated soft tissue changes and bone marrow edema may result in diagnostic errors. The MRI helps to assess hip and groin pain when FAI is suspected, and the diagnostic accuracy for OO is not as reliable as with CT and these only identify them in 29% of the patients. Only OO of >4 mm in size can be identified on an MRI scan [1, 3].
In this case the OO had an extra-articular location on the anterior acetabular rim that was not evident on plain X-rays. CT was not considered as one of the initial studies and an MRI was chosen instead. The MRI did not show associated FAI and no bone marrow edema or soft tissue changes. When OO was suspected the CT was done and revealed a 6-mm lesion with a nidus and was surrounded with sclerosis which made it easy to identify.
Multiple treatments options for OO have been described. Nonsurgical management consists mainly in alleviating pain. Oral salicylates NSAIDs have been used effectively to relieve and control pain and may spontaneously heal after years [1–4]. Chronic use of NSAIDS has potential detrimental side effects and not always resolves the problem, so surgical management is often preferred. Our patient had been self-administering NSAIDS for over a year with partial relief in his symptoms.
Open excision was the first technique described that consisted in “en bloc” resection of the OO [1, 6]. This could be challenging due to the complex anatomical location and the difficulty in identifying a small lesion. Hospital days and the recovery period were prolonged. Percutaneous techniques reduce surgical time, hospital stay, recovery time and complications [6, 7]. CT guidance aids for an accurate localization of the tumor. RFA with CT guidance has a high rate success after ablation of the OO and is the current preferred method. The disadvantage of this technique is the expensive system it requires. Cannulated drill and curettage with CT guidance are an excellent option to excise the OO and obtain histological proof. This technique is an accessible option with high success rates with the support of radiologist to lower the probabilities of missing the OO. This was the technique chosen with a successfull outcome.
In conclusion, hip joint OO is rare and difficult to diagnose if there is an inadequate history and physical evaluation. Suspicion should be aroused when patient characteristic match with an OO. Percutaneous excision and curettage with CT guidance are an excellent alternative treatment that is simple, reproducible and accessible.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest whatsoever arising out of the publication of this article.
FUNDING
Authors have not received any funding for this study.



