-
PDF
- Split View
-
Views
-
Cite
Cite
Margot Kelly-Hedrick, Jason M Frerich, Emily M Peairs, Diana M Cardona, Rohith Arcot, Brandon Smith, Michael Abern, Chad Miller, Muhammad M Abd-El-Barr, Retroperitoneal dermoid cyst presenting with radiculopathy symptoms: a case report, Journal of Surgical Case Reports, Volume 2022, Issue 12, December 2022, rjac588, https://doi.org/10.1093/jscr/rjac588
Close - Share Icon Share
Abstract
Dermoid cysts rarely present in the retroperitoneal space or during adulthood. In this case report, we describe the clinical presentation, operative and post-operative course of a 31-year old with a retroperitoneal dermoid cyst. The patient presented with buttock and leg pain/paresthesia found to have a retroperitoneal mass between the psoas muscle and L5/S1 disk space. We describe the operative approach, including intra-operative images, of the resection by a team of urologists and neurosurgeons. The histology is also presented. Finally, we discuss the benefits of use of intra-operative ultrasound and neuromonitoring.
INTRODUCTION
Dermoid cysts are a germ cell tumor comprised of two of the three germ cell layers (ectoderm, mesoderm, endoderm), typically presenting in the gonads [1]. Extragonadal teratomas usually present in midline structures such as the mediastinum or sacrococcygeal region [2]. Dermoid cysts are rarely present in the retroperitoneal space and, when present, are usually diagnosed in infancy [1]. Occasionally dermoid cysts are discovered in adulthood, usually incidentally in young women who are asymptomatic, though several case reports exist with abdominal or pelvic pain as the presenting symptom [1, 3, 4–6].
Retroperitoneal dermoid cysts have a 25% chance of malignancy and can be difficult to diagnose on imaging alone [2, 7]. For this reason, surgical resection is considered the best diagnostic and therapeutic option [2].
We report the case of a 31-year-old woman presenting with right buttock and leg pain/paresthesia. Magnetic resonance imaging (MRI) imaging demonstrated a retroperitoneal mass between the psoas muscle and L5/S1 disk space, associated with the descending right L4/L5 nerve roots and lumbosacral plexus. We report the operative approach of the mass resection, which was determined to be a dermoid cyst on post-operative pathology. A retroperitoneal dermoid cyst with radiculopathy has not previously been described.
CASE REPORT
The patient is a 31-year-old female who was first admitted to a spine clinic for right buttock and posterior thigh pain with intermittent pain, paresthesia and weakness in the right lower leg and foot. She had a history of a duplex dysplastic kidney on the right side at birth, and had undergone nephrectomy in the remote past.
Her initial MRI of the lumbar spine revealed a partially cystic and solid mass measuring 2.5 cm along the medial edge of the right psoas muscle and near the right L4 and L5 nerve roots (Fig. 1). A percutaneous biopsy was inconclusive, showing benign adipose tissue. Conservative management (physical therapy and medications) failed to adequately control her symptoms.
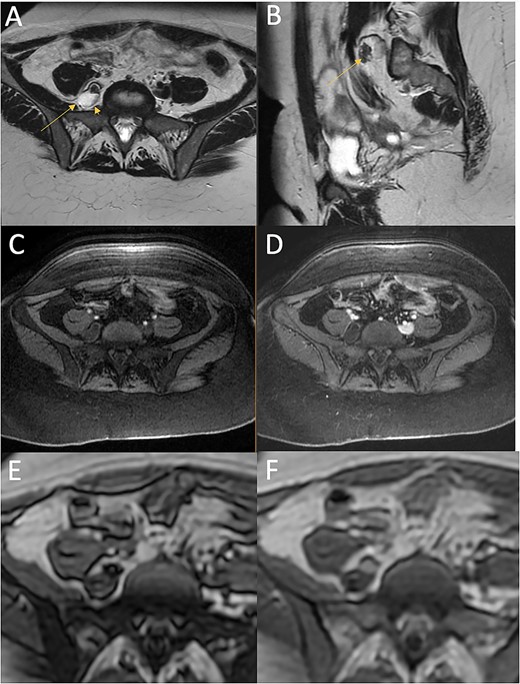
T2 (A, axial; B, sagittal) and T1-weighted with fat saturation (C, axial pre-contrast; D, axial post-contrast), T1 dixon (E, axial in-phase; F, axial out-of-phase) images from the MRI of the pelvis at presentation. The heterogeneous complex cystic mass (arrow) is located lateral to the vertebral body and posterior and medial to the psoas muscle. It is characterised by predominantly high T2 signal, with a region of dark T2 signal anteriorly, low T1 signal on fat-saturated images. The anterior T2 dark component shows drop out on the out-of-phase imaging compared with the in-phase imaging indicating a component of fat. It abuts the right L5 nerve root (arrowhead).
On presentation to our center, her neurological exam was insignificant except for lumber region tenderness to palpation and antalgic gait favoring the right. Her symptoms were significantly limiting the quality of her life; she estimated she was able to complete 0% of her normal daily living activities. Her baseline ODI score was 54 [8].
An MRI of the pelvis showed a multilobulated lesion medial to the right psoas muscle measuring 2.6 cm × 1.7 cm, similar to her previous MRI 4 months earlier (Fig. 1). Based on the imaging, the differential diagnosis included hematoma, lymphatic structure, nerve sheath tumor or myxoma. Given her persistent and debilitating symptoms, the patient elected to undergo surgery for resection and diagnosis of the retroperitoneal mass.
The patient was placed supine on a flat Jackson Table and given general anesthesia. After a midline incision, the peritoneal compartment was mobilised medially and the retroperitoneal space was entered. The common, external and internal iliac arteries and iliac vein were identified and carefully dissected and mobilised.
We began the resection of the mass with an operative microscope. Ultrasound was utilised to aid in the localisation of the lesion and guide resection in both cranial and caudal directions to find the poles of the lesion. Throughout this process, neuromonitoring remained quiet and stimulation did identify motor nerves. The lesion was internally debunked to aid in resection and was found to contain a gray ‘snowflake’-like material, then dissected out and removed (for intra-operative imaging, see Fig. 2). Intra-operative frozen section consultation revealed an epithelial-lined cyst.

Intra-operative pictures. Direct electrical stimulation of lesion (L) when first reached (A) located between and posterior to the iliac artery (ia) and iliac vein (iv). Lesion contained both fatty (B) and pearly appearing flakes (C).
After the mass was removed, the incision was closed, covered and anesthesia placed a regional block at the T10 level. The blood loss was less than 50 mL.
Gross examination in the pathology lab demonstrated aggregates of yellow-tan, lobulated adipose and fibrous soft tissue. Histology of the revealed a cystic structure lined by stratified squamous epithelium, associated adnexal structures (hair follicle and sebaceous glands), haphazardly arranged nerve twigs, fibrosis and adipose tissue (Fig. 3). Immunohistochemistry for CD117, DOG1, CD34 and S100 in the more fibrotic, spindle cell areas, were negative. Additionally, molecular testing for MDM2 gene amplification was performed and the result was negative, excluding the possibility of a retroperitoneal liposarcoma. Overall, the morphologic findings were consistent with a dermoid cyst (cystic teratoma).
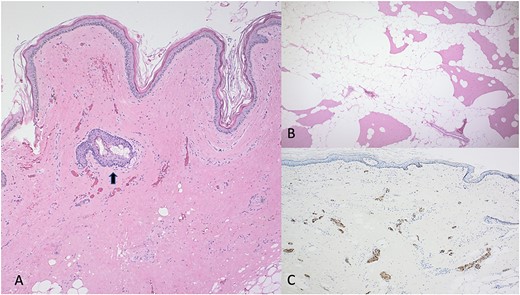
(A) Dermoid cyst (H&E; 40×). The cystic structure is lined by squamous epithelium. In the surrounding dense fibrosis, there is a hair follicle and an associated sebaceous gland (arrow). (B) Surrounding the cystic lesion these is adipose tissue, reminiscent of an intramuscular lipoma (H&E; 40×). (C) Within the dense fibrous soft tissue of the cyst, there are numerous small nerve twigs (S100 protein; 40×).
The patient began ambulation on post-op day 1 and pain was adequately controlled on oral pain medications. She was discharged home on post-op day 6. Unfortunately, the patient had to be hospitalised several days later for post-operative ileus, which was managed conservatively; she was discharged 6 days later.
At her 6-week visit, the patient reported she had started in-home physical therapy, and was able to drive and do basic daily activities. Her pain was improved compared with pre-operatively. By her three-month follow-up appointment, her pain was a 3/10 and her ODI was 28 [8].
DISCUSSION
In this case report, we describe the clinical presentation, operative and post-operative course of a 31-year-old with a retroperitoneal dermoid cyst. Retroperitoneal cysts are rare to find in patients older than 30 and very few case reports describe neurological symptoms as the presenting symptom [2, 3, 9]. In the case of our patient, the mechanism for her buttock and leg pain is unclear, though it is favored to be secondary to mass effect on the nearby right L5 nerve root. To our knowledge, there is not consensus on the follow-up after resection, particularly for an adult with an atypical dermoid cyst location.
A multidisciplinary team and the use of intra-operative technology—both neuromonitoring and ultrasound—was central to the success of the resection. Urologists are comfortable navigating the retroperitoneal space using an anterior approach and neurosurgeons are able to resect lesions close to nervous structures. Somatosensory evoked potentials, motor evoke potentials, and free-running electromyography helped ensure we did not damage nerves within or around the mass. Intra-operative ultrasound helped guide the resection—an inexpensive and easy to use tool that is particularly useful for soft tissue visualisation with cystic components [10, 11].
We report the operative case of a 31-year-old with radiculopathy and a rare retroperitoneal dermoid cyst that was successfully resected by a multidisciplinary team, aided by intra-operative ultrasound and neuromonitoring.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
CONSENT
The patient consented to her case to be published in the scientific literature.
DATA AVAILABILITY
This manuscript presents a case report and therefore the data is not available publicly or upon request to protect the privacy and identity of the patient.



