-
PDF
- Split View
-
Views
-
Cite
Cite
Aishwarya Jangam, Christopher Gillespie, A rare case of colo-salpingeal fistula complicating acute sigmoid diverticulitis, Journal of Surgical Case Reports, Volume 2022, Issue 12, December 2022, rjac573, https://doi.org/10.1093/jscr/rjac573
Close - Share Icon Share
Abstract
Colo-salpingeal fistulae due to acute diverticulitis are rare entities. A 65-year-old female with a 5-day history of left iliac fossa pain, fevers and diarrhoea was seen in a metropolitan hospital. Initial computed tomography of the abdomen and pelvis characterized a left tubular adnexal structure with an air fluid level and normal-appearing colon and was reported as pyosalpingitis. Worsening sepsis despite antibiotics prompted further imaging where thickening of the sigmoid colon was noted, and the provisional diagnosis was revised to complicated acute diverticulitis with perforation into the left fallopian tube/ovary. This was managed with a laparoscopic anterior resection and en bloc left salpingo-oopherectomy, and was followed by an uneventful recovery. The presence of a gas-containing collection remains a sensitive imaging sign for the presence of an enteric fistula and a high index of suspicion should be maintained when this is encountered.
INTRODUCTION
Diverticular disease is the one of the most encountered colonic pathologies by general surgeons in Western countries. More than 50% of people aged over 60 years of age are noted to have diverticulosis with 10–25% of the population experiencing the diverticular disease in their lifetime [1]. Complications of diverticulitis include perforation, intestinal obstruction, abscess formation, fistula formation and pylephlebitis. The rate of fistula formation is around 14% after an episode of acute diverticulitis [2]; however, colosalpingeal fistulas are a rare entity with a review of the literature revealing less than 11 cases characterizing this in the literature and none previously in Australia [3–9]. The presentation of colo-salpingeal fistulae is varied and diverticulitis as the primary pathology should be kept in mind when there is concern of an adnexal fistulating process.
CASE REPORT
A 65-year-old woman was referred by her general practitioner to the gynaecology service of a metropolitan hospital with a 5-day history of abdominal pain lateralizing to the left iliac fossa, fevers, anorexia and diarrhoea. She was hemodynamically stable and the physical examination revealed marked tenderness to deep palpation and mild guarding in the left iliac fossa. Bimanual examination revealed an exquisitely tender and difficult to define adnexal mass. Her background history included a lower caesarean section, hyperlipidaemia and osteoporosis. No family history of malignancy was present. Interestingly, the initial contrast computed tomography (CT) abdomen and pelvis scan characterized a left tubular adnexal structure with an air fluid level but normal colon, and was reported as pyosalpingitis (Fig. 1). A subsequent pelvic ultrasound scan noted sigmoid thickening. Inflammatory markers were raised with a white cell count of 15.4 × 109 cells/L and CRP of 155 mg/L. Although initially afebrile, she spiked a temperature of 38.4 and commenced IV antibiotics for pelvic inflammatory disease. Given the uncommon presence of gas in the tubo-ovarian abscess and the suggestion of diverticulitis, a general surgical opinion was sought. It was agreed upon that this was most likely acute sigmoid diverticulitis complicated by a local perforation into the left salpingeal tube and ovary.
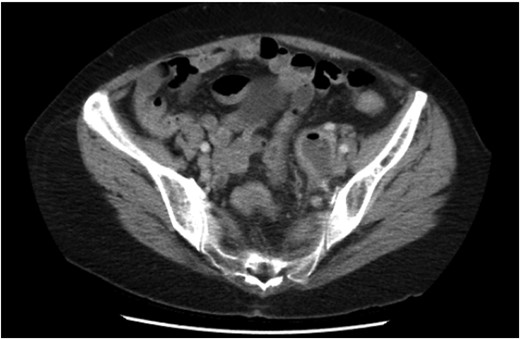
Initial CT demonstrating a gas containing the left adnexal mass and normal sigmoid colon.
Non-operative management with broad-spectrum IV antibiotics, bowel rest and fluids was trialled. Despite initial clinical improvement with a reduction in pain and down-trending inflammatory markers the patient was once again febrile on day 3 of her admission with plateauing of the inflammatory markers and ongoing pain. A progress CT scan (Fig. 2) showed an unchanged adnexal collection now with sigmoid thickening. Given the findings and lack of clinical improvement, the patient proceeded to have a laparoscopic anterior resection and en bloc left salpingo-opherectomy. Intra-operatively (Figs 3 and 4), the fistula between the sigmoid colon and the left salpinx was very clearly demarcated. Histology confirmed acute diverticulitis locally perforating into the left salpinx and ovary and forming an abscess. An uneventful recovery followed.

Repeat CT scan demonstrating thickening of the sigmoid colon adjacent to the adnexal mass.
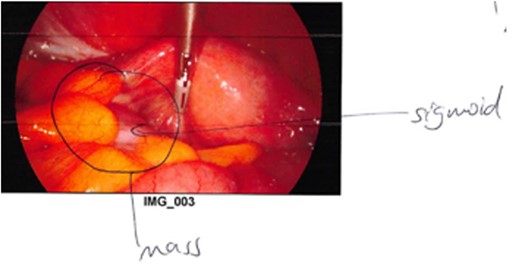
Intraoperative photograph demonstrating the colo-salpingeal fistula.

DISCUSSION
Colo-salpingeal fistulas are rare entities and have been reported to occur due to a myriad of aetiologies ranging from tuberculosis, primary salpingitis, colorectal or ovarian malignancies, appendicitis and diverticulitis [3–9]. Fistulization from a perforated diverticulum, leading to colovesicular, colovaginal or coloenteric fistulas, is more common. Of the published cases of colo-salpingeal fistulas, acute presentations in the context of diverticulitis are the anomaly – with most cases presenting with subacute or chronic symptoms [3]. Other cases have been diagnosed on hysterosalpingogram performed as part of investigation for infertility [4–6] and, historically, via barium enema[8, 9]. In the acute setting, however, given current clinical practice, a CT scan will be the most likely investigation modality for identifying this condition. The presence of a gas-containing collection remains a sensitive CT sign for the presence of an enteric fistula and a high index of suspicion should be maintained when this is encountered. En bloc resection of the sigmoid colon and the affected fallopian tube and ovary, as performed on our patient, is the mainstay of treatment in these cases.
ACKNOWLEDGEMENTS
There are no conflicts of interest or supports (financial or otherwise) to be disclosed for this case report. The authors confirm that the data supporting the findings of this study are available within the article.



