-
PDF
- Split View
-
Views
-
Cite
Cite
Jeong Hee Han, Byoung Chul Lee, Young Mok Park, Hyuk Jae Jung, Jung Bum Choi, Huge adrenal schwannoma: a rare type of adrenal tumor, misconceived as adrenocortical carcinoma, Journal of Surgical Case Reports, Volume 2022, Issue 12, December 2022, rjac562, https://doi.org/10.1093/jscr/rjac562
Close - Share Icon Share
Abstract
Schwannoma is a benign and uncommon neoplasm arising from the neural crest cells. The most common tumor sites are the skin and subcutaneous tissue of the head and neck. Retroperitoneal schwannomas account for 1–3% of all schwannomas and are predominantly female. In particular, adrenal schwannoma is very rare, and due to its large size at the time of diagnosis, adrenal schwannoma is frequently misdiagnosed as adrenocortical carcinoma or pheochromocytoma. Adrenal schwannoma is difficult to distinguish it from other adrenal diseases based on imaging findings alone. In this report, we introduce the case of a huge left adrenal schwannoma.
INTRODUCTION
Schwannoma is a benign and uncommon neoplasm arising from the neural crest cells. The most common tumor sites are the skin and subcutaneous tissue of the head and neck, but sometimes schwannoma originates from the pancreas, stomach, kidney and liver [1]. Retroperitoneal schwannomas account for 1–3% of all schwannomas and are predominantly female [2]. In particular, adrenal schwannoma is very rare, and due to its large size at the time of diagnosis, adrenal schwannoma is frequently misdiagnosed as adrenocortical carcinoma or pheochromocytoma [3]. Adrenal schwannoma is classically well-encapsulated, hypervascular and heterogeneous, so it is difficult to distinguish it from other adrenal diseases based on imaging findings alone. Histopathological and immunohistochemical studies of surgically removed specimens are the only and essential means of confirming the diagnosis [2, 4].
In this report, we introduce the case of left huge adrenal schwannoma in an 87-year-old woman who presented with abdominal pain and discomfort.
CASE REPORT
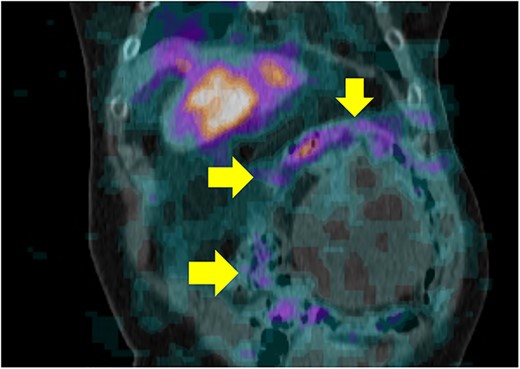
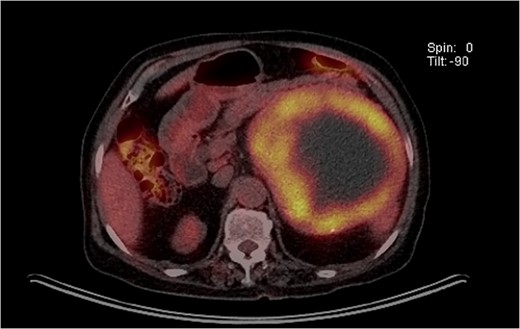
An 87-year-old female, with no past medical history, was admitted to the emergency center in our tertiary institution with a 1-month history of abdominal pain and discomfort. Initial workup using abdomino-pelvic computed tomography (APCT) presented a 16-cm-sized heterogeneous tumor in the left adrenal gland (Fig. 1). She was referred to the endocrine department for further evaluation. The results of laboratory tests, including those for measuring plasma levels of adrenocorticotrophic hormone, cortisol, aldosterone, epinephrine, norepinephrine, metanephrine, dehydroepiandrosterone sulfate as well as urine levels of epinephrine, norepinephrine, metanephrine, vanillylmandelic acid and homovanillic acid were within normal limits. Plasma renin activity was also normal. The levels of serum markers for carcinoma were within normal limits radiolabeled metaiodobenzylguanidine single photon emission computed tomography (I-123 MIBG SPECT) presented a huge mass with mild peripheral uptake of the left adrenal gland (Fig. 2). Finally, positron emission tomography (PET) was done for evaluation of distant metastasis. PET showed the accumulation of fluorodeoxyglucose (FDG) in the left adrenal tumor with [maximum standardized uptake value (SUVmax: 7.4)] and lymph nodes in the para-aortic area (SUVmax: 2.4; Fig. 3). We initially expected adrenocortical carcinoma with lymph nodes metastasis.

APCT showed a 16-cm-sized heterogeneous tumor in the left adrenal gland.
I-123 MIBG SPECT showed huge mass with mild peripheral uptake of the left adrenal gland.
PET showed the accumulation of FDG in the left adrenal tumor and lymph nodes in the para-aortic area.
Radical adrenalectomy with para-aortic lymph nodes dissection was performed with the patient’s consensus. Grossly, a well-demarcated and solid mass measuring 16.8 × 11.8 × 11.5 cm was seen in the left adrenal gland (Fig. 4).

A well-demarcated and solid mass measuring 16.8 × 11.8 × 11.5 cm.
The final pathologic result of the tumor at the left adrenal gland was 16.8-cm-sized cellular schwannoma. Histologically, the mass mostly consisted of an interlacing arrangement of spindle cells (Fig. 5A). Immunohistochemical analysis of the tumor revealed that the tumor cells were diffusely strong positive for S100 protein (Fig. 5B) with weakly positive for smooth muscle actin (SMA), EMA and negative for PANCK, desmin, human melanoma black-45 (HMB45), p53 and CD34. The Ki-67 labeling index was 2%.
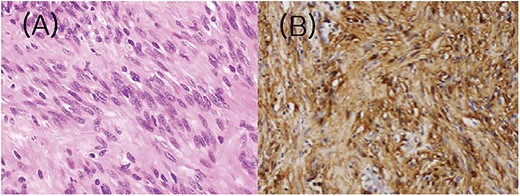
Histologic and immunohistochemical features of the tumor. (A) Spindle cells are arranged in fascicles with intervening stroma. (B) Cells showed strong S100 immunoreactivity.
The postoperative course was uneventful and the patient was discharged on the 15th postoperative day. She is free of disease 5-month post-surgery. The Institutional Review Board of Pusan National University Hospital approved this study and waived the informed consent requirement.
DISCUSSION
In our case, we treated the patient with a 16-cm huge left adrenal schwannoma. Schwannomas arise from the Schwan cells surrounding the peripheral nerves and mostly they originate from the nerves of the head and neck or the peripheral extremities [2, 5]. They are rarely found in the retroperitoneum; <3% of benign schwannomas are seen in a retroperitoneal site [6]. Also, only ~6% of primary retroperitoneal tumors are found to be schwannomas [7]. With only ~80 cases reported worldwide, adrenal schwannoma is a very rare disease [3, 8]. A recent study reported 33 cases of adrenal schwannomas with a median patient age of 49-year old, median tumor size of 5.5 cm and a predominance in women [9]. Some studies reported that schwannoma is more common in old women, with an approximate male-to-female ratio of 2:3 [4, 10], which is a consistent report with our case. The risk factors of adrenal schwannoma were not known well because of its rarity, but some studies reported that adrenal schwannoma is associated with neurofibromatosis and prior ionizing radiation is the only known risk factor [4]. In our case, the patient had no such medical history.
Adrenal schwannoma is usually asymptomatic and is found incidentally with large size using imaging studies [11]. Because of the slow-glowing nature of the tumor, patients are often asymptomatic until it grows large enough to cause mass effects including abdominal pain or discomfort [12]. For this reason, adrenal schwannoma is mostly diagnosed in a large size and it is very rare to be diagnosed in a small size with any symptoms. In our case, the patient was asymptomatic for a long time and complained of abdominal pain and discomfort as its size grew to 16 cm.
Due to the degeneration, cystic change, hemorrhage and calcification within adrenal schwannoma, it often appears heterogeneous on delayed-phase CT and magnetic resonance imaging (MRI). For this reason, adrenal schwannoma is often misdiagnosed for the tumors of the retroperitoneum such as adrenocortical carcinoma, pheochromocytoma, ganglioneuroma, neuroblastoma and adrenal metastatic lesion. In our case, adrenocortical carcinoma was strongly suspected due to suspicious para-aortic lymph nodes seen on PET-CT. Shen et al. suggested that schwannoma can be ruled out through the arterial phase of CT scan showing necrosis and minimal degree of tumor enhancement [13]. But because schwannomas have non-specific or uncommon findings in imaging studies, the definitive diagnosis must be determined through histologic and immunohistochemical methods. The histology of schwannoma shows spindle-shaped cells having elongated to wavy nuclei with alternating hypercellular and hypocellular regions called Antoni A and Antoni B, respectively [14] and immunohistochemically, schwannomas have positive S-100 antibodies [5]. These findings were consistent with our case.
Adrenal schwannoma is usually diagnosed in very large size. For this reason, Adrenal schwannoma sometimes causes significant displacement of nearby structures. Petrucciani et al. reported that adrenal schwannoma can present in close to the great vessels and with several feeding vessels draining from the tumor into the vena cava [15]. Also, some studies reported that tumor can displace the recto-sigmoid colon, ureter, uterus and psoas muscle [11]. In our case, the tumor presented many large feeding arteries arising from aorta. Because of too many feeding arteries, there was a large amount of bleeding in the para-aortic area after tumor removal, and meticulous hemostasis was required.
Adrenal schwannoma is typically benign tumor and has a good prognosis with complete surgical resection. Zhou et al. concluded that the patient had favorable survival with no evidence of recurrences after follow-up from 7 to 115 months [3]. Our patient has a good outcome with no specific complication after surgery and is free of disease 5-month post-surgery. In conclusion, despite adrenal schwannoma being a rare and typically benign tumor, since it cannot be distinguished from other malignant diseases on preoperative imaging, it should always be considered in any adrenal tumors.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None reported.



