-
PDF
- Split View
-
Views
-
Cite
Cite
Alwaleed K Alammar, Nedhal A Alqumber, Abdulrahman Alsahabi, Jamal Almadani, Fatema Alsubhi, Faisal A Alfaqeeh, Successful functional salvage of a hindfoot injury with isolated soft tissue reconstruction: a case report, Journal of Surgical Case Reports, Volume 2022, Issue 11, November 2022, rjac517, https://doi.org/10.1093/jscr/rjac517
Close - Share Icon Share
Abstract
Calcaneus has an important functional role in walking, running, gait and transferring 80% of total weight. Due to the paramount role of the calcaneus in function, there is a trend toward ‘below knee amputation’ for such heel injuries, associated with complete loss of calcaneus. Complex calcaneal defects represent a reconstructive challenge, due to few reported cases in the literatures, limited surgical options, and lack of long-term outcomes. We present a young patient regaining near normal function, weight bearing and independent walking after sustaining complex hindfoot defect that resulted in total loss of the calcaneus secondary to a landmine blast injury managed by soft tissue reconstruction only without skeletal reconstruction.
INTRODUCTION
Calcaneus bone plays an important role in transferring 80% of total body weight. Moreover, pressure is retained and conveyed through the connective tissue over the calcaneus, thus, any injury to these structures may affect the ability to walk [1].
There is a trend toward ‘below knee amputation’ for massive heel injuries associated with complete loss of calcaneus [2]. It is based on the rationale that only a soft tissue reconstruction without skeletal reconstruction would not provide a painless functional ankle [3]. Two reconstructive approaches have been described: single stage reconstruction of soft tissue and skeletal elements by osteocutaneous free tissue transfer, or staged reconstruction by providing soft tissue coverage followed by skeletal reconstruction [1,4]. Priorities would be preventing infection, obtaining durable soft tissue cover and preservation of function [4].
We present a case of blast injury of the hindfoot with exposed bone, neurovascular bundle and complete loss of the calcaneus. The patient regained full weight bearing with painless near normal gait after soft tissue reconstruction only without skeletal reconstruction of the calcaneus bone.
CASE REPORT
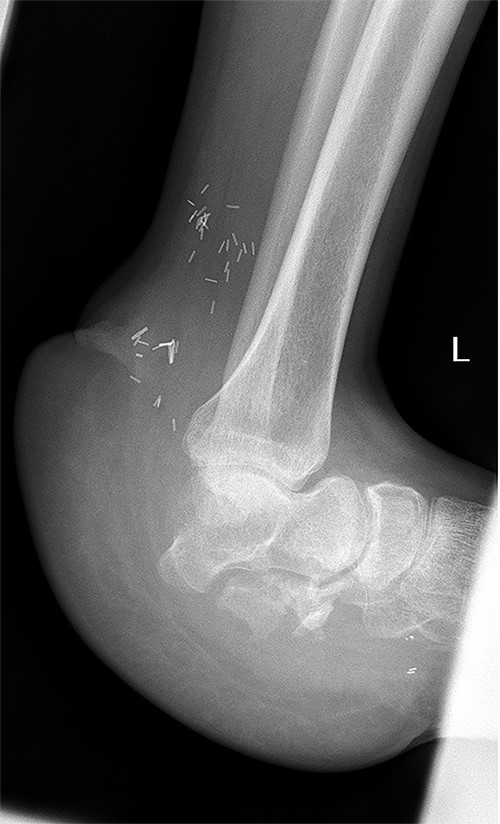
A 32-year-old male, without any known medical illnesses, presented after sustaining a blast injury to the left foot by a landmine. Upon presentation the patient was hemodynamically stable, with isolated large left hindfoot defect associated with exposed vital structures (talonavicular joint, tibial nerve and posterior tibial artery and vein), both tibial nerve and posterior tibial artery and vein where intact with intact sensation over the remaining skin of the foot; (Fig. 1). X-ray showed total calcaneus bone loss (Fig. 2), computed tomography angiogram showed intact anterior and posterior tibial arteries, fractured talus and complete loss of calcaneus bone.

Intraoperative image of the left foot depicting the extent of injury.

X-ray of the left foot showing complete loss of the calcaneus bone.
Patient was operated on the same day for wound debridement in preparation for definitive soft tissue coverage. Irrigation and surgical debridement was performed. A negative pressure wound dressing was applied and empiric antibiotic therapy initiated. Definitive reconstruction was performed 3 days later. The posterior tibial artery, vena comitants and short saphenous vein were used as recipient vessels. Contralateral Perforator fasciocutaneous tensor fascia lata flap harvested.
Microsurgical anastomosis was performed in an end-to-side fashion. Two venae comitants were anastomosed to comitants of posterior tibial and short saphenous veins in end-to-end fashion. The flap was fixed with loose sutures then light dressing was applied. Foot was immobilized with a splint. The donor site was covered by skin graft.
One week after surgery, the flap showed good healing, and the drains were removed. Two weeks after surgery, we allowed a gentle passive followed by active range of motion once the flap had demonstrated healing (Fig. 3). Full weight bearing was initiated at 1 month postoperatively; 2 months after surgery the patient started to walk independently with a painless near normal gait, walking up and down the stairs. The following parameters of movement and functionality were obtained: Plantar flexion 45-degree, Dorsiflexion 20-degree, Inversion 30-degree and Eversion 25-degree; Scoring 84 on Freiburg Ankle Score (FAS; depicted in Video 1 and Video 2).

Post-operative image of the injured left foot 3 weeks after flap coverage.
DISCUSSION
Calcaneus transfers 80% of a person’s total body weight. Many injuries, especially those caused by landmines, gunshot injuries and traffic accidents, can lead to complex defect [3], which might jeopardize walking and weight bearing.
The treatment of calcaneus fractures is a challenge because of inadequate vascularity of this region [5]. Open fractures of the calcaneus are rare, ranging between 0.8 and 10% of all calcaneal fractures, and there are only a few reports described so far [6–9]. Further complicating their management, open fractures of the calcaneus carry higher incidence rates of infection, which range from 37 to 60% [7–9]. Treatments of complex calcaneal fracture include muscle and myocutaneous flaps, partial calcanectomy, total calcanectomy and below-the-knee amputation [8]. Traditionally, amputation has been the treatment of choice for extensive involvement of the calcaneus [5,10]. Recently, muscle flaps with skin grafts have become the preferred choice when filling wounds that have osteomyelitis at the base [8]. The aim is to facilitate the initial phase (heel strike) of the gait cycle, and rearrange the distribution of pressure over foot [9]. Due to the rare occurrence of open calcaneal fractures, there is a paucity of published data on soft tissue reconstruction alone for these injuries in the orthopedic and reconstructive surgical community. Our patient had a large calcaneal bone and soft tissue defect; thus, we selected a tensor fascia lata free flap alone for reconstruction of the defect. Advantages of this flap include reliable blood supply, bulky subcutaneous tissue and fascia, which can be used to cover large defects [9]. For this flap, the vascular pedicle anatomy is more constant [11]. Other advantage of this flap is its hidden and less visible site; minimizing aesthetic concerns [8]. In our patient, weight bearing was initiated 1 month after surgery. At 18-month postoperatively, the patient had a near normal painless gait, normal plantar sensation and no difficulty climbing or descending stairs with stable talonavicular joint (Fig. 4). The patient recovered near full range of motion and complete independent mobility.
X-ray of the left foot 18 months post flap coverage showing a stable talonavicular joint.
When considering large complex defects of the hindfoot, the following issues are essential to consider: Can, and, should this foot be saved? If so, can a suitable functional recovery be achieved? Evaluation of these injuries must consider the extent of the defect, the weight-bearing status of the extremity and the presence or absence of active infection of the soft tissue or bone. The etiology of the defect, age of the patient and working activity may all lead physicians to pursue an optimum reconstructive option when the patient desires limb salvage. In this report, a soft tissue free flap provided an excellent outcome for an active patient with a complex defect. We believe that bulky soft tissue reconstruction might be sufficient for selected heel defect with complete calcaneus loss.
CONCLUSION
Calcaneus bone is vital in normal weight bearing. Free tissue transfer has become a standard option for reconstruction of complex defects of the foot and ankle. The positive result in this patient supports that a soft tissue reconstruction only without reconstructing skeletal element in selected cases can be an option for defects associated with open hindfoot and ankle injuries with partial or total calcaneus bone loss.
CONFLICT OF INTEREST STATEMENT
The authors have no financial interest in any of the methods, products or devices mentioned in this article.
FUNDING
No funding was received for this study.
References
Banerjee R, Waterman B, Nelson J, Abdelfattah A. Reconstruction of massive midfoot bone and soft tissue loss as a result of blast injury.



