-
PDF
- Split View
-
Views
-
Cite
Cite
Masashi Ishikawa, Hiroyuki Ishikawa, Tetsuya Fukui, Masaki Ikeda, Kazuo Ono, An extremely rare case of anterior mediastinal leiomyosarcoma: a case report, Journal of Surgical Case Reports, Volume 2022, Issue 11, November 2022, rjac513, https://doi.org/10.1093/jscr/rjac513
Close - Share Icon Share
Abstract
We herein report an extremely rare case of leiomyosarcoma found in the anterior mediastinum. A 79-year-old man presented to our hospital with an anterior mediastinal mass incidentally found by chest computed tomography (CT) scan. Percutaneous needle biopsy revealed the presence of an undifferentiated sarcoma. Transsternal resection of the tumor with adjacent left mediastinal pleura was performed, and pathological analysis revealed a leiomyosarcoma, which was 11 cm in diameter, with bare margins. He was followed up on an outpatient basis with no adjuvant therapy. Although mediastinal lymph node recurrence was suspected on chest CT scan 18 months after surgery, the patient remained asymptomatic and rejected any additional antitumor treatments. He died of respiratory failure after incidental traumatic spinal injury about 30 months after tumor resection.
INTRODUCTION
Primary mediastinal leiomyosarcomas (LMS) arising in the anterior mediastinum are rare. The origin is estimated to be soft tissues or smooth muscles of mediastinal vessels. In this report, we present the case of a successfully resected primary LMS of the anterior mediastinum. Mediastinal lymph node recurrence was suspected on chest computed tomography (CT) scan after 18 months. However, no further intervention was administered due to the patient’s preference. The patient died of respiratory failure after traumatic cervical spine injury 30 months after surgery, which was unrelated to the tumor.
CASE REPORT
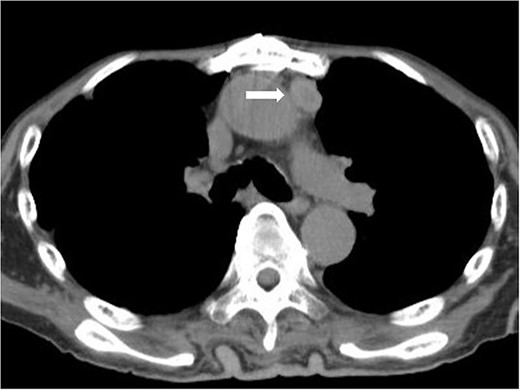
A 79-year-old man was referred to our hospital with an abnormal shadow on chest X-ray. He had a history of light smoking (3 pack-years) with no major past medical history. Physical examinations and laboratory tests, including tumor markers, were unremarkable. The chest CT revealed the presence of an anterior mediastinal mass, which had its longest diameter being 11 cm. The mass compressed adjacent great vessels and the heart posteriorly. On contrast-enhanced magnetic resonance imaging scan, the tumor presented as a well-demarcated, homogenously enhanced mass, and the direct invasion into surrounding structures was not apparent. Positron emission tomography (PET)-CT scan revealed a slight uptake of fluorodeoxyglucose (FDG) by the tumor (standardized uptake value [SUV] max = 3.32) and no signs of metastases (Fig. 1). Thymoma, thymic cancer, thymic neuroendocrine tumor or malignant lymphoma was suspected. However, ultrasound-guided percutaneous needle biopsy through the anterior chest wall revealed an undifferentiated sarcoma.
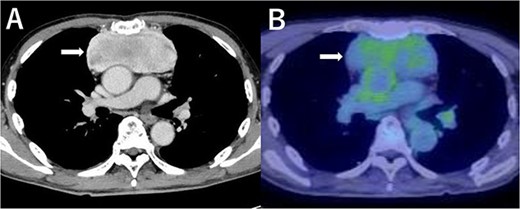
Contrast-enhanced chest CT scan (A) and FDG-PET scan (B) of the tumor (SUVmax = 3.32).
The patient underwent tumor resection by median sternotomy ~1 month after the first visit to our hospital. The patient was under general anesthesia with mechanical ventilation during the median sternotomy. Although an electric sternal saw for splitting the sternum required extra power and left an impression on the anterior surface of the tumor (Fig. 2), the tumor was successfully resected along with adjacent left mediastinal pleura. Operation time was 303 minutes, and intraoperative bleeding volume was 825 ml. The postoperative clinical course was uneventful. The patient was discharged on postoperative day 9.
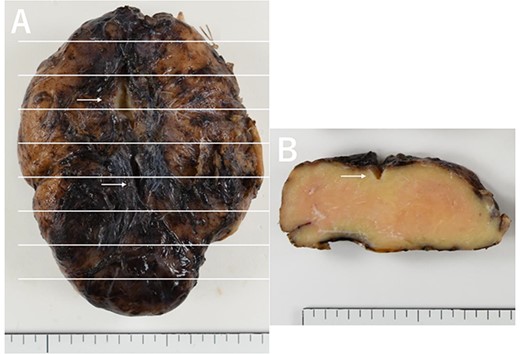
Macroscopic view (A) and cut surface (B) of the tumor. Impression of the sternal saw at the time of median sternotomy can be observed (white arrows).
The resected tumor was 11.0 × 9.0 × 3.0 cm in size and elastically hard. Its cut surface had a homogenously faint camel-to-pink color. Histological evaluation revealed that the tumor was composed of large, polygonal or spindle malignant cells, typical of an undifferentiated sarcoma or liposarcoma (Fig. 3). Additionally, 3–5 mitotic figures per 10 high-power fields and associated necrosis were observed. The tumor was unencapsulated and exposed to surrounding tissues (pleura, adipose tissue and thymus). Immunohistochemical staining was positive for p16, desmin, muscle-specific antigen and α-smooth muscle actin (Fig. 4), but negative for myoglobin, caldesmon, cytokeratin AE1/3, CD34, S100, MDM2, neurofilament and CD57. The final pathological diagnosis was primary mediastinal leiomyosarcoma.
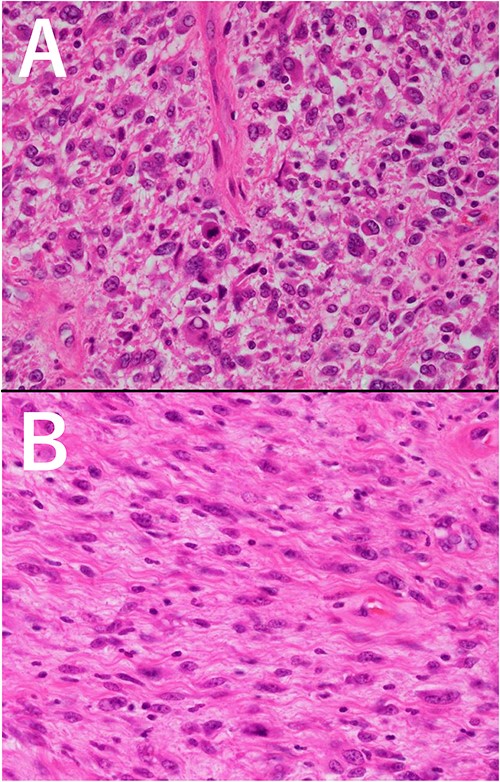
Microscopic view of the tumor (HE staining, ×200 magnification). (A) pleomorphic area, (B) spindle cell area.
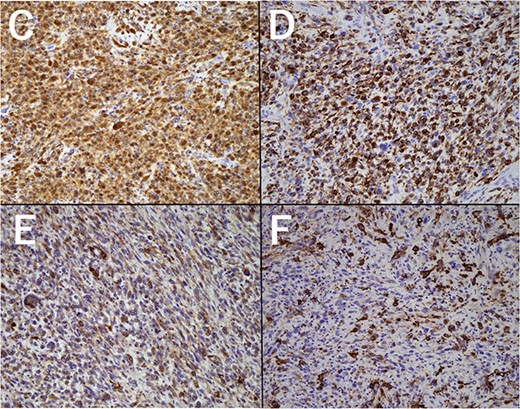
Immunohistochemical staining of the tumor (×200 magnification). (C) p16, (D) Desmin, (E) Muscle-specific antigen, (F) α-smooth muscle actin.
The patient was followed-up on an outpatient basis, without any additional chemotherapy or radiotherapy. On routine chest CT checkup after 18 months, lymphadenopathies were observed in the anterior mediastinum (Fig. 5), but no further investigation nor clinical intervention was intended on patient’s will. Twelve months later, he was diagnosed with nephrotic syndrome after he presented with sudden edema of the lower limbs. Although he recovered from the nephrotic syndrome after administration of corticosteroids, he suffered a traumatic spinal injury due to an accidental fall from the hospital bed. He finally died at home from respiratory failure 30 months after the surgery.
Chest CT scan 18 months after surgery. Mediastinal lymph node recurrence was suspected.
DISCUSSION
Primary LMS located in the anterior mediastinum are sufficiently rare. Thus far, only eight cases have been reported in the English literature since 2000 [1–8]. The clinicopathological features of the reported and current cases are summarized in Table 1. They seem to have an equal sexual distribution and mostly occur in middle-to-old age. Although the average tumor size was relatively large (83.3 ± 50.1 mm), no distant metastasis has been reported.
Characteristics of previously reported and present cases of anterior mediastinal LMS since 2000
| References | Age/ Gender | Symptoms | Maximum tumor size (mm) | SUV max | Needle biopsy | Interventions | Operative approach | Resected site along with tumor | Recurrence | Prognosis |
| [1] | 85F | CXR abnormality | 14 | 3.41 | Not performed | Surgery | VATS | Pericardium | no | Alive/5 M |
| [2] | 82F | Chest pain | 65 | 10.9 | Not performed | Surgery | MS | LUL | Yes | Alive/24 M |
| [3] | 61 M | CXR abnormality | 52 | n/a | Not performed | Surgery | Unknown | RUL | Unknown | Lost-follow |
| [4] | 76F | Dyspnea | 114 | n/a | Low-grade leiomyosarcoma | Unknown | Unknown | Unknown | Unknown | Details unknown |
| [5] | 51 M | Dyspnea/Dysphagia/Edema | 40 | n/a | Not performed | Surgery (×2) + RT | MS | SVC | No | Alive/10 M |
| [6] | 66 M | Hoarseness | 65 | 12.33 | Vascular leiomyosarcoma | RT + Surgery | MS | Aortic arch | Yes (resected) | Alive/16 M |
| [7] | 55F | Chest pain/Cough | 180 | n/a | Mesenchymal tumor | Surgery + Chemotherapy/RT | Thoracotomy | Pericardium/ RML | no | Alive/10 M |
| [8] | 45 M | Chest pain/Dyspnea | 110 | n/a | Mesenchymal tumor | Surgery + RT | Thoracotomy | Med pleura | no | Alive/8 M |
| present case | 79 M | CXR abnormality | 110 | 3.32 | Sarcoma, unclassified | Surgery | MS | Med pleura | Yes | Dead/30 M (non-tumor death) |
| References | Age/ Gender | Symptoms | Maximum tumor size (mm) | SUV max | Needle biopsy | Interventions | Operative approach | Resected site along with tumor | Recurrence | Prognosis |
| [1] | 85F | CXR abnormality | 14 | 3.41 | Not performed | Surgery | VATS | Pericardium | no | Alive/5 M |
| [2] | 82F | Chest pain | 65 | 10.9 | Not performed | Surgery | MS | LUL | Yes | Alive/24 M |
| [3] | 61 M | CXR abnormality | 52 | n/a | Not performed | Surgery | Unknown | RUL | Unknown | Lost-follow |
| [4] | 76F | Dyspnea | 114 | n/a | Low-grade leiomyosarcoma | Unknown | Unknown | Unknown | Unknown | Details unknown |
| [5] | 51 M | Dyspnea/Dysphagia/Edema | 40 | n/a | Not performed | Surgery (×2) + RT | MS | SVC | No | Alive/10 M |
| [6] | 66 M | Hoarseness | 65 | 12.33 | Vascular leiomyosarcoma | RT + Surgery | MS | Aortic arch | Yes (resected) | Alive/16 M |
| [7] | 55F | Chest pain/Cough | 180 | n/a | Mesenchymal tumor | Surgery + Chemotherapy/RT | Thoracotomy | Pericardium/ RML | no | Alive/10 M |
| [8] | 45 M | Chest pain/Dyspnea | 110 | n/a | Mesenchymal tumor | Surgery + RT | Thoracotomy | Med pleura | no | Alive/8 M |
| present case | 79 M | CXR abnormality | 110 | 3.32 | Sarcoma, unclassified | Surgery | MS | Med pleura | Yes | Dead/30 M (non-tumor death) |
n/a: not applicable, CXR: chest X-ray, RT: radiotherapy, VATS: video-assisted thoracoscopic surgery, MS: median sternotomy, LUL: left upper lobe, RUL: right upper lobe, RML: right middle lobe, Med pleura: mediastinal pleura
Characteristics of previously reported and present cases of anterior mediastinal LMS since 2000
| References | Age/ Gender | Symptoms | Maximum tumor size (mm) | SUV max | Needle biopsy | Interventions | Operative approach | Resected site along with tumor | Recurrence | Prognosis |
| [1] | 85F | CXR abnormality | 14 | 3.41 | Not performed | Surgery | VATS | Pericardium | no | Alive/5 M |
| [2] | 82F | Chest pain | 65 | 10.9 | Not performed | Surgery | MS | LUL | Yes | Alive/24 M |
| [3] | 61 M | CXR abnormality | 52 | n/a | Not performed | Surgery | Unknown | RUL | Unknown | Lost-follow |
| [4] | 76F | Dyspnea | 114 | n/a | Low-grade leiomyosarcoma | Unknown | Unknown | Unknown | Unknown | Details unknown |
| [5] | 51 M | Dyspnea/Dysphagia/Edema | 40 | n/a | Not performed | Surgery (×2) + RT | MS | SVC | No | Alive/10 M |
| [6] | 66 M | Hoarseness | 65 | 12.33 | Vascular leiomyosarcoma | RT + Surgery | MS | Aortic arch | Yes (resected) | Alive/16 M |
| [7] | 55F | Chest pain/Cough | 180 | n/a | Mesenchymal tumor | Surgery + Chemotherapy/RT | Thoracotomy | Pericardium/ RML | no | Alive/10 M |
| [8] | 45 M | Chest pain/Dyspnea | 110 | n/a | Mesenchymal tumor | Surgery + RT | Thoracotomy | Med pleura | no | Alive/8 M |
| present case | 79 M | CXR abnormality | 110 | 3.32 | Sarcoma, unclassified | Surgery | MS | Med pleura | Yes | Dead/30 M (non-tumor death) |
| References | Age/ Gender | Symptoms | Maximum tumor size (mm) | SUV max | Needle biopsy | Interventions | Operative approach | Resected site along with tumor | Recurrence | Prognosis |
| [1] | 85F | CXR abnormality | 14 | 3.41 | Not performed | Surgery | VATS | Pericardium | no | Alive/5 M |
| [2] | 82F | Chest pain | 65 | 10.9 | Not performed | Surgery | MS | LUL | Yes | Alive/24 M |
| [3] | 61 M | CXR abnormality | 52 | n/a | Not performed | Surgery | Unknown | RUL | Unknown | Lost-follow |
| [4] | 76F | Dyspnea | 114 | n/a | Low-grade leiomyosarcoma | Unknown | Unknown | Unknown | Unknown | Details unknown |
| [5] | 51 M | Dyspnea/Dysphagia/Edema | 40 | n/a | Not performed | Surgery (×2) + RT | MS | SVC | No | Alive/10 M |
| [6] | 66 M | Hoarseness | 65 | 12.33 | Vascular leiomyosarcoma | RT + Surgery | MS | Aortic arch | Yes (resected) | Alive/16 M |
| [7] | 55F | Chest pain/Cough | 180 | n/a | Mesenchymal tumor | Surgery + Chemotherapy/RT | Thoracotomy | Pericardium/ RML | no | Alive/10 M |
| [8] | 45 M | Chest pain/Dyspnea | 110 | n/a | Mesenchymal tumor | Surgery + RT | Thoracotomy | Med pleura | no | Alive/8 M |
| present case | 79 M | CXR abnormality | 110 | 3.32 | Sarcoma, unclassified | Surgery | MS | Med pleura | Yes | Dead/30 M (non-tumor death) |
n/a: not applicable, CXR: chest X-ray, RT: radiotherapy, VATS: video-assisted thoracoscopic surgery, MS: median sternotomy, LUL: left upper lobe, RUL: right upper lobe, RML: right middle lobe, Med pleura: mediastinal pleura
Based on radiological findings, LMS in the anterior mediastinum on contrast-enhanced CT is characterized as a well-defined, heterogeneously enhanced soft tissue mass, sometimes with calcification, showing obvious space-occupying effects on surrounding structures [3]. Similar to the current case, three other cases reported findings from PET-CT scan, which showed variable FDG uptake (SUV max = 3.3–12.3) [1, 2, 6]. Percutaneous needle biopsies performed in the current case and four other cases revealed three sarcomas [4, 6] and two mesenchymal tumors [7, 8]. Although the potential risk of tumor implantation might be of concern, histological diagnosis before surgery should be recommended, especially to exclude chemo-sensitive tumors, such as lymphomas and germ cell tumors.
Preoperative radiotherapy was administered in only one case with superior vena cava (SVC) syndrome [6], with no substantial effect on tumor regression. Operative approaches include thoracoscopy, thoracotomy and median sternotomy, depending on the location, size and invasiveness of the tumor. All tumors that underwent surgery were successfully resected with surrounding mediastinal structures, including parietal pleura, pericardium, great vessels (SVC, aorta) and parts of the right/left upper lobes. Considering the generally low sensitivity to chemotherapy or radiotherapy of sarcomas, complete surgical resection could be the treatment of choice, if possible.
Although three cases (including the current case) recorded tumor recurrence after surgery, no apparent deaths due to local recurrence were ascertained [2, 6], and no distant metastases were reported. This fact might reflect the rather indolent nature of primary anterior LMS.
In conclusion, we report an extremely rare case of primary LMS arising from the anterior mediastinum. Despite the bare tumor margins after tumor resection and suspected local recurrence without any therapies, the patient remained asymptomatic 30 months until his death resulting from other incidental medical conditions. Accumulation of similar cases is necessary to confirm the suspected rather indolent nature and recommended therapeutic approach for this tumor.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



