-
PDF
- Split View
-
Views
-
Cite
Cite
Alex Guachilema Ribadeneira, Mauricio Palacios Gordon, Sandra Morocho, Edwin Guillermo Bahamonde, Andrea Daniela Basantes, Estefanía Parra Valverde, Left-sided gallbladder ‘sinistroposition’ associated with an anatomical variant of cystic duct insertion: case report, Journal of Surgical Case Reports, Volume 2022, Issue 11, November 2022, rjac510, https://doi.org/10.1093/jscr/rjac510
Close - Share Icon Share
Abstract
True left-sided gallbladder (LSGB) is a rare congenital anomaly with an incidence of 0.1–1.2%. It is more common in women than in men at a ratio of 5:1. Its etiology is unknown, although several theories have been proposed. The symptoms are similar to those of a normal gallbladder, which makes the preoperative diagnosis difficult despite imaging studies. In most cases, the diagnosis is achieved intraoperatively. LSGB is associated with biliary anomalies, and the incidence of biliary tract lesions is high. Four-port laparoscopic cholecystectomy is a safe procedure for LSGB. Surgical technique varies according to each case. Preoperative imaging studies have low sensitivity for diagnosis, and the surgeon should be familiar with ductal and vascular anatomical variants in addition to possessing the ability to change the conventional surgical technique to optimize the exposure and minimize the risk of bile duct injury.
INTRODUCTION
Left-sided gallbladder (LSGB) or sinistroposition in the absence of situs inversus is an infrequent anatomical anomaly with an incidence of 0.04–1.1%, which is associated with extrahepatic biliary tract alterations [1, 2].
The gallbladder is defined as left-sided when it is located to the left of the falciform ligament between Segments III and IV [3]. There are three recognized variants of LSGB as follows: (i) associated with situs inversus, (ii) true LSGB and (iii) a gallbladder located to the left of an anomalous round ligament [1].
This anomaly is not always detected by imaging studies, and its identification is often incidental during surgery. Bile duct lesions can be present because of the association between LSGB and anatomical variants of the extrahepatic biliary tract.
The present report describes the case of a female patient aged 17 years with true LSGB, which was not reported in the preoperative imaging studies, that was detected intraoperatively and associated with an anatomical variant of the cystic duct.
CLINICAL CASE PRESENTATION
We present the case of a 17-year-old woman with no previous medical history who presented to our center with abdominal colicky-type pain of moderate intensity in the right hypochondriac region radiating to the subscapular region on the same side accompanied by nausea and general malaise. Clinical examination revealed scleral icterus, a soft, depressible abdomen and a positive Murphy’s sign.
Laboratory tests, including blood count, glucose, urea and creatinine, were normal. Liver function tests were abnormal, with elevated liver enzymes and bilirubin; amylase and lipase were normal. Abdominal ultrasound (US) showed thickening of the gallbladder wall with an image casting a posterior acoustic shadow and a 0.9-mm dilatation of the common bile duct. Magnetic resonance cholangiogram showed a ductus hepatocholedochus measuring 3.9 mm and a distal hypointense area suggestive of gallstones, and no alteration of the bile ducts was reported; however, an image suggestive of cystic duct insertion variation was visualized (Fig. 1). The patient underwent endoscopic retrograde cholangiopancreatography (ERCP), which revealed an edematous swollen and congested papilla with a papillary pore that appeared damaged, hepatocholedochus of 8 mm, with no endoluminal images suggesting calculus.
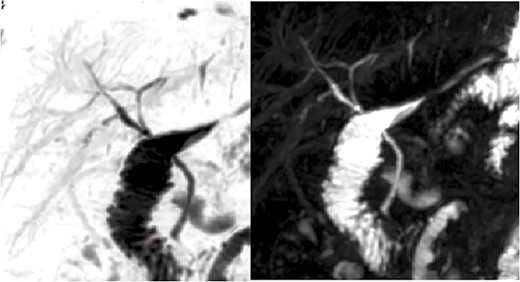
Colangio-magnetic resonance imaging with suspected variation of cystic duct insertion.
The patient was scheduled for laparoscopic cholecystectomy the day after the ERCP. The cholecystectomy was performed using four ports (conventional technique), an 11-mm transumbilical port, a 10-mm subxiphoid port and two 5-mm ports at the right midclavicular line and right anterior axillary line. The initial laparoscopy showed that the gallbladder was located to the left of the falciform ligament on hepatic segment III (Fig. 2). The gallbladder was retracted to the right side while applying cephalic traction (Fig. 3). The anterior fold of the cholecystoduodenal ligament was exposed to allow the careful dissection of Calot’s triangle. However, because adequate identification of the critical safety path was not achieved, anterograde cholecystectomy was performed. The findings included dilatation of the bile duct, a posterior cystic artery that was ligated using a titanium clip and an anatomical variant of cystic duct implantation causing drainage into the right hepatic duct. A hem-o-lok was placed proximally, and the duct was cut and divided (Figs 4–6). The operation time was 120 min. The patient was transferred to the recovery room and was discharged post-operatively.
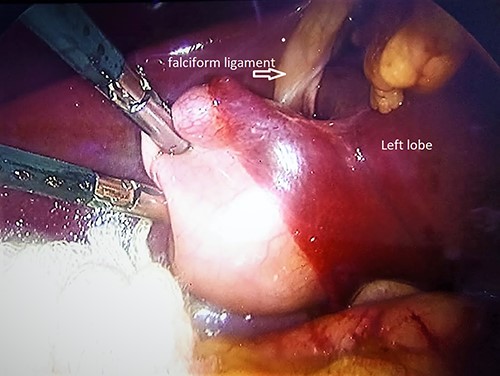
Intraoperative findings; gallbladder to the left of the falciform ligament in the left lobe.
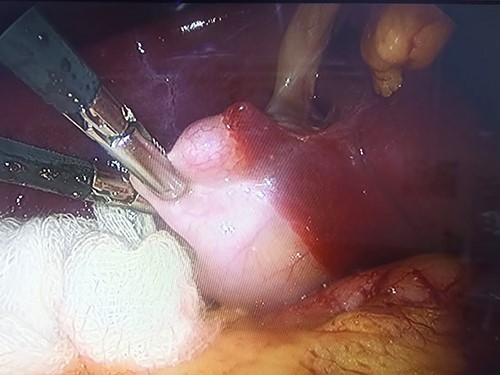
Traction of the gallbladder fundus toward the right of the falciform ligament.
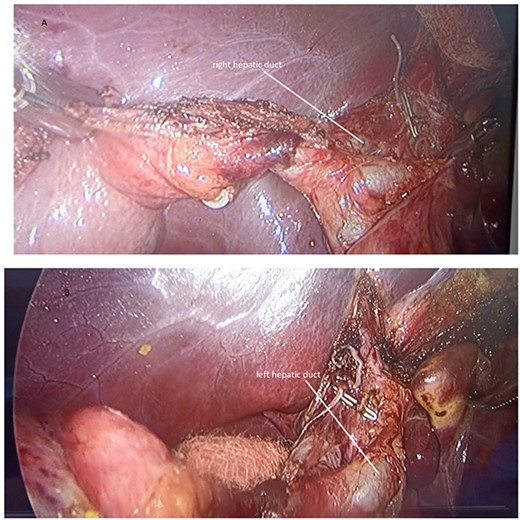
(A) Anterograde cholecystectomy, posterior cystic artery with a titanium clip; (B) Exposure of the extrahepatic biliary duct revealing anatomical variant.

Placement of the Hem-o-lok proximal and distal to the cystic duct and its division.
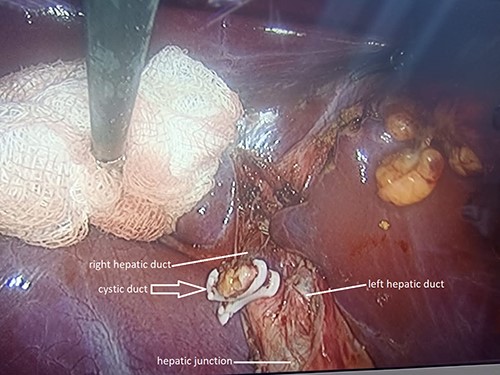
Anatomical variant of the cystic duct; drainage into the right hepatic duct.
DISCUSSION
True LSGB is a rare anatomical anomaly with an incidence rate of 0.1–1.2% and a rate of 0.07–0.08% in patients undergoing cholecystectomy. It occurs more frequently in women than in men at a ratio of 5:1 [2, 4].
The etiology of LSGB is unknown, although several theories have been proposed. According to one theory, the gallbladder arises from the hepatic diverticulum in the normal site; however, its attachment to the developing left lobe results in the migration of the gallbladder to the left lobe. Another theory proposes that the gallbladder develops directly from the left hepatic duct with regression of the main gallbladder [1].
LSGB can present with the typical right-sided symptoms of a normally positioned gallbladder. Abongwa reviewed 55 patients with true LSGB, and 75% of them presented with pain in the right superior quadrant, which was explained as failure of the visceral nerve fibers to transpose along with the gallbladder [1].
Advances in imaging techniques have resulted in an increase in the number of reports of left gallbladder; however, routine studies fail to diagnose it in most cases. According to Pereira et al., LSGB is detected in 29.6% of imaging studies. Computed tomography shows the highest predictive value, whereas US shows the lowest predictive value at 2.7%. In 81.1% of patients with symptomatic gallstones, LSGB was detected during surgery [5].
Anatomical variations of the biliary tree are present in 42–58% of patients [6]. Biliary duct lesions associated with LSGB are present in 7.3% of patients [1]. Abnormal drainage of the cystic duct into the right hepatic duct, as observed in the present case, is extremely rare, occurring in ~0.3–0.4% of patients [7]. Surgeons need to be aware of the ductal and vascular variations, especially in patients with an anomaly such as LSGB.
There are several modifications of the laparoscopic cholecystectomy technique for LSGB. Among these, the use of fluorescence cholangiography, intraoperative cholangiography, changes in the position of the subxiphoid trocar to the left of the round ligament, the use of left subcostal and left anterior axillary line ports, retraction of the falciform ligament and anterograde dissection to facilitate visualization of the anatomical structures and prevent bile duct injury have been described. Lee et al. reported that the median surgery time is 50 min (range, 35–160 min), which is less than that indicated by Jung et al., who reported an operation time of 103 min (range, 65–240 min) [2, 4, 5, 8].
In the present case, we performed laparoscopic cholecystectomy using four ports placed in conventional locations. Anterograde dissection of the gallbladder was performed to facilitate its removal and thus avoid damage to the bile duct; because an adequate identification of the critical safety path could not be achieved, intraoperative cholangiography was not performed and is not available in our center. Variations in the technique can be applied, and if necessary, conversion to open surgery is possible.
In conclusion, true LSGB is a rare entity that is detected intraoperatively in most cases. Imaging studies have low sensitivity for preoperative diagnosis. It is associated with anomalies of the biliary tree, which requires the surgeon to be prepared and possess anatomical knowledge of ductal variants. The identification of points of reference is essential to ensure that laparoscopic cholecystectomy is performed effectively and safely by experienced surgeons.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None



