-
PDF
- Split View
-
Views
-
Cite
Cite
Yume Minagawa, Yasuhiro Ishiyama, Toshiyuki Fukuda, Ichitaro Mochizuki, Shingo Ito, Masataka Oneyama, Manabu Amiki, Yoshiaki Hara, Kazuhiro Narita, Yuji Tachimori, Manabu Goto, A case of sigmoid colon volvulus with transanal ileus tube placement and Sharon’s operation performed safely, Journal of Surgical Case Reports, Volume 2022, Issue 11, November 2022, rjac429, https://doi.org/10.1093/jscr/rjac429
Close - Share Icon Share
Abstract
Although endoscopic repair is often performed for sigmoid colon volvulus without intestinal necrosis, surgery is the common choice of treatment due to recurrence. With no established treatment, Hartmann’s operation or sigmoid colon resection is often performed. We report a case of a 65-year-old man with transanal ileus tube placement before surgery for sigmoid colon volvulus to prevent recurrence and achieve intestinal decompression followed by Sharon’s operation to achieve one-stage anastomosis. The patient showed good postoperative course, with no recurrence 3 months after surgery. This report discusses the usefulness of the transanal ileus tube and Sharon’s operation for sigmoid colon volvulus without intestinal necrosis along with a review of the literature.
INTRODUCTION
Colonic volvulus is the third most common cause of colonic obstruction in the world, with the sigmoid colon being the most common site of volvulus [1]. However, there is a lack of a clear consensus on the treatment of this condition.
Emergency surgery is mandatory when sigmoid colon torsion is accompanied by intestinal necrosis, and Hartmann’s operation with colostomy is the common choice according to the condition of the intestinal tract [2].
When the torsion is not accompanied by intestinal necrosis, the general choice is endoscopic repair, but this method only releases the torsion, and the recurrence rate is high [3]. Sigmoid mesenteroplasty and fixation are simple surgical procedures with low risk of complications; however, they have a high recurrence rate, and hence resection of the excess bowel and anastomosis performed simultaneously are preferable if possible [4, 5].
Although the literature reports several surgical cases of sigmoid colon volvulus [6], neither the surgical technique nor the appropriate surgical timing has been established. Sharon’s operation is a surgical method that does not require a lateral approach [7].
In this report, we describe a case of sigmoid colon volvulus that repeatedly recurred in a short period of time, for which insertion of a transanal ileus tube to decompress the colon and Sharon’s operation were performed as elective surgery, resulting in bowel anastomosis simultaneously.
CASE PRESENTATION
A 65-year-old man with a medical history of chronic obstructive pulmonary disease (COPD) and hypertension had sigmoid colon volvulus that occurred three times during 4 months. He visited our hospital for abdominal pain and distension and was admitted with a diagnosis of recurrent sigmoid colon volvulus, for which endoscopic repair was performed. However, we decided to perform surgery due to repeated recurrences in a short period of time. Preoperative blood tests and examination of physiologic functions revealed no abnormal findings.
Endoscopic examination showed that the site of torsion was near the sigmoid rectum (Fig. 1), and a computed tomography(CT) scan revealed prominent dilatation of the oral bowel (Fig. 2).
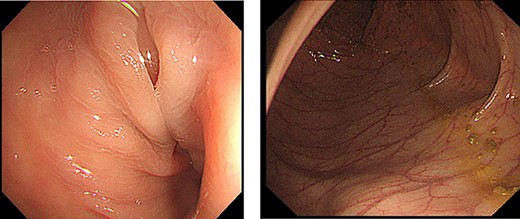
Colonoscopy findings. Torsion was observed in sigmoid rectum. No mucosal necrosis was observed.
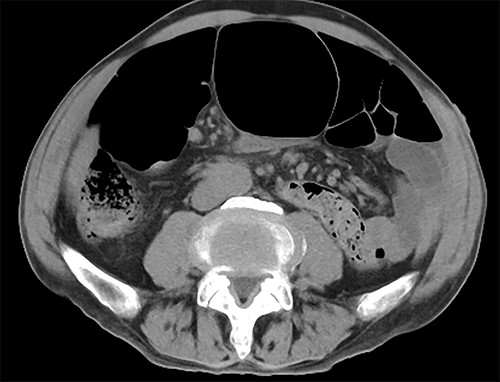
CT findings. CT showed dilation of the oral intestinal tract was observed.
The patient had recurrence during a week before surgery, which required endoscopic repair.
A transanal ileus tube was inserted, which was washed daily, and Sharon’s operation was performed.
Surgical procedure
The transanal ileus tube was removed after the introduction of anesthesia. A 12-mm port was inserted at the umbilical site and insufflated for intra-abdominal observation. An additional 5-mm port was placed in the right midline for observation (Fig. 3).

Surgical findings. Twelve millimeter port was inserted at the umbilical site and an additional 5-mm port was placed in the right midline for observation.
The sigmoid colon was elongated, and a scar was detected near the SD junction, which appeared to be a site of repeated torsion (Fig. 4). Dilation of the sigmoid colon revealed no inflammation on the serosal surface. The laparoscopic procedure was completed after confirming that the sigmoid colon was sufficiently elevated to the left lower abdomen. A 4-cm cross incision was made at the opposite of McBurney’s point, and the sigmoid colon was raised outside the wound (Fig. 5). The intestine was considered to be sufficiently decompressed to allow anastomosis. The intestinal tract was separated, and anastomotic reconstruction was performed using functional end-to-end anastomosis. The operation duration was 89 min, and the bleeding amount was 5 ml.
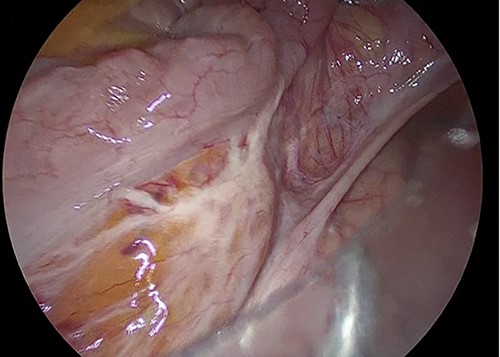
Surgical findings. Sigmoid colon was elongated and there was scar near the SD junction.
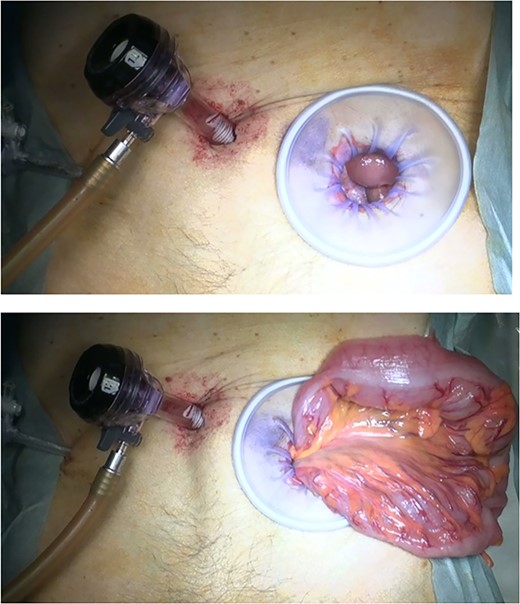
Method of Sharon operation. Sigmoid colon was raised outside the wound at the opposite of Mc Burney’s point.
The patient started drinking water on postoperative day (POD) 1 and eating on POD2. Although there was an elevated inflammatory response postoperatively, no evidence of leakage or other signs of infection was detected on imaging, and the patient was discharged on POD10 after the administration of antibacterial medication. He has progressed without recurrence to date.
DISCUSSION
In our case, the patient required surgical treatment for the sigmoid volvulus due to recurrences in a short period of time. Hartmann’s operation was an option because the intestinal edema and dilation were expected to be significant due to repeated recurrences. Nevertheless, considering the patient’s desire to avoid a colostomy for maintaining his quality of life, we decided to perform one-stage anastomosis by decompressing the intestinal tract using a transanal ileus tube before elective surgery. We performed Sharon’s operation to shorten the duration of surgery due to the patient’s past history of COPD. Considering the possible difficulty of performing intestinal anastomosis, we decided to determine the final surgical approach, including Hartmann’s operation, using intraoperative findings with laparoscopy. Consequently, we successfully achieved bowel decompression, after which we could perform bowel resection and one-stage anastomosis with little laparoscopic manipulation.
Sharon et al. reported about sigmoid colon resection through left McBurney’s incision, which is a simple surgical procedure that does not require a lateral approach [7]. However, there are limited case reports involving Sharon’s operation, partially because laparoscopic surgery is becoming more widespread and colon resection is becoming technically simplified. In the previous report of Sharon’s operation [6], the operation duration was > 90 min with no complications or recurrences.
Although some reports have demonstrated ileus tube placement for sigmoid colon volvulus [8, 9], it is not common. In several reported cases, intestinal decompression with transanal ileus tube placement was successful. In our case also, the transanal ileus tube placement itself might have contributed to the prevention of recurrence until surgery was performed. Therefore, we believe that transanal ileus tube placement for sigmoid colon volvulus without mucosal necrosis is useful.
Although we performed intraoperative laparoscopic observation to determine the degree of intestinal decompression in our patient, Sharon’s operation under spinal subarachnoid anesthesia is an option for patients who have difficulty undergoing general anesthesia due to poor respiratory function. In the present case, intestinal decompression through transanal ileus tube placement appeared to be useful for achieving successful one-stage intestinal anastomosis.
CONCLUSION
We report a case of sigmoid colon volvulus for which Sharon’s operation was performed after transanal ileus tube placement to decompress the colon.
We believe that preoperative decompression by transanal ileus tube placement is useful, especially for cases in which a one-stage anastomosis is desired.
ACKNOWLEDGEMENT
The authors would like to thank Enago (www.enago.jp) for the English language review.
CONFLICT OF INTEREST STATEMENT
None declared.



