-
PDF
- Split View
-
Views
-
Cite
Cite
Carolina Arró Ortiz, Victoria Hughes, Darío Ramallo, Gastric perforation after blunt abdominal trauma: first case report in Argentina, Journal of Surgical Case Reports, Volume 2022, Issue 11, November 2022, rjac394, https://doi.org/10.1093/jscr/rjac394
Close - Share Icon Share
Abstract
We report the case of a 18-year-old male with gastric perforation due to blunt abdominal trauma as a result of a vehicular collision. An exploratory laparotomy with suturing of the lesion and an omental patch is performed. The post-operative outcome was favorable. Traumatic injury is a frequent cause of hospital admission to the emergency department in Argentina, and vehicle collisions are the first cause of death and permanent disability in young adults. Isolated gastric perforations following blunt abdominal are an uncommon finding, and there are only a few published cases in the literature. It is interesting to discuss the type of surgical approach.
INTRODUCTION
Traumatic injury is a frequent cause of hospital admission to the emergency department in Argentina, and motor vehicle accidents are the first cause of death and permanent disability in young adults [1]. In blunt abdominal trauma, the most frequently involved intra-abdominal organs are the spleen, kidney and liver; the involvement of the gastrointestinal tract is rare. Gastric perforation is very rare, accounting for <1.7% of all blunt abdominal trauma [2].
Herein, we report a case of a 18-year-old male with gastric perforations due to blunt abdominal trauma.
CASE REPORT
A 18-year-old male without relevant past medical history was admitted to the emergency department 2 hours after a motor vehicular collision. At admission, we evaluated according to the Advanced Trauma Life Support algorithm. The airway was permeable and the respiratory physical examination was normal. The patient presented tachycardia and reported severe generalized abdominal pain. Abdominal inspection revealed an abrasion zone measuring 5 × 6 cm in the left hypochondrium without active bleeding. On palpation, the abdomen was tender and guarded. He was conscious, with a Glasgow coma score of 15/15. Laboratory tests revealed hemoglobin of 14 g%. Chest X-rays were normal. Computed tomography (CT) of the abdomen revealed pneumoperitoneum with a moderate amount of intraperitoneal free fluid and discontinuity of the stomach wall, suggesting full thickness perforation at this level (Fig. 1).
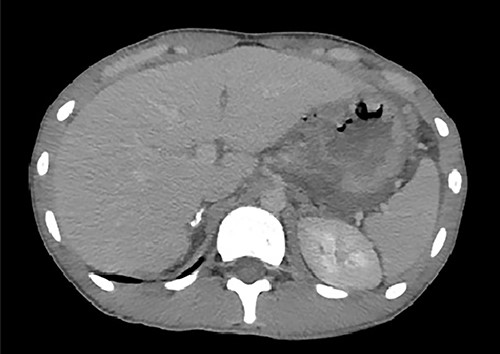
An axial image from the abdominal CT scan demonstrates discontinuity of the stomach wall and a connection with the free air, suggesting perforation at this level.
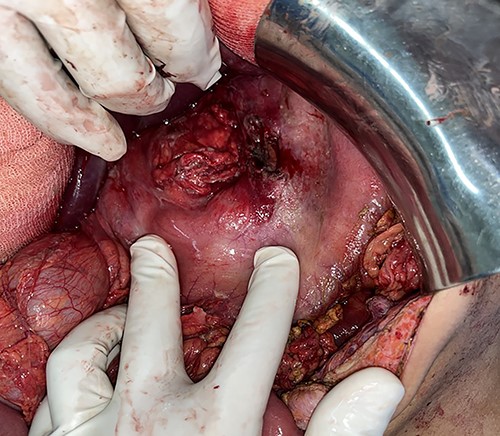
An emergency exploratory laparotomy was performed, finding serosanguinous fluid with undigested food particles. A transverse full-thickness laceration on the lesser curvature of the stomach was observed, measuring ~4 × 2 cm in length in the anterior wall (Fig. 2) and another similar lesion of the gastric body on the posterior wall (Fig. 3). The rest of the examination was normal without other associated organ injuries. Therefore, we performed a primary repair of the perforated stomach with an omental patch. The patient was sent to the intensive care unit with restriction of oral intake, fluid resuscitation, broad-spectrum antibiotics and adequate pain management without any ionotropic support.

Intraoperative findings: full thickness perforation on the lesser curvature of the stomach measuring 4 × 2 cm in length in the anterior wall.
Intraoperative findings: perforation lesion along the posterior gastric wall measuring 1 × 1 cm.
The post-operative outcome was uneventful. The patient was discharged from the hospital on the eighth day.
DISCUSSION
The first case of blunt gastric rupture was described in 1922 [3]; from that moment on, only a few more cases have been described, and this is mainly because it is a very rare pathology and it occurs in <1.7% of all abdominal trauma [3].
Several factors have been described which increase the risk of stomach rupture, the most studied being a history of full stomach or recent food and a high-velocity trauma to the left side of the body [2]. Regarding the mechanisms of injury to the stomach, they are the same as those described for visceral injuries, the sudden increase in intraluminal pressure, due to a direct blow or compression against solid structures or sudden deceleration [4]. The walls of the stomach are thick, so it is relatively resistant to a blunt injury, and its injury is usually associated with major trauma and consequently also with other injuries, both abdominal (splenic and hepatic) and thoracic [3].
According to the few cases published in the literature, it can be deduced that the most frequently affected area by gastric injury due to blunt abdominal trauma is the anterior wall, although injuries can occur in any part of the stomach [5]. Stomach injuries usually present as a single lesion, although there have been reports where they have ruptured in multiple sites.
The clinical manifestations of gastric perforations are usually a challenge for the treating multidisciplinary team, and many of these patients have an altered state of consciousness, or are intoxicated patients [6]. Sometimes, in turn, they can present associated lesions that could divert the focus of attention. The typical manifestations of hollow viscus injury are usually abdominal pain, and the abdomen may present tense and with peritonism and it may also present with shock [7]. Other tests related to gastric injury are traces of blood through the nasogastric tube or hematemesis. When these signs and symptoms are not present, complementary studies play a leading role in reaching the diagnosis. The most characteristic radiographic sign is the pneumoperitoneum. In the ultrasound examination, we can observe free liquid. CT is currently the gold standard for gastric injuries [8]. CT may show discontinuities in the stomach wall, including extravasation of luminal contents and any free gas bubbles; other signs include focal thickening, abnormal enhancement of the gastric wall, gastric wall hematoma, fatty infiltration and abscesses surrounding [8, 9]. However, CT may be negative in up to 13% of patients [9].
In the management of gastric injury, a primary suture is usually adequate and feasible in most injuries unless there is devascularization of the stomach where a gastrectomy must be performed, which is an extremely infrequent gesture [5, 10]. None of these surgical procedures can be performed in severe trauma where damage limitation surgery is aimed at hemorrhage control and limiting the soiling of the peritoneum is of the essence. If we take into account the reports on the primary closure of perforated gastric ulcers, post-operative mortality increases concerning the diameter of the lesion, being 12% in <10 mm and 24% in >10 mm [11]. However, the choice of operative technique will depend on the position and size of the ulcer and the age and fitness of the patient.
Regarding the type of surgical approach, the publications that refer to the management of gastric ulcers report that the raffia and the omental patching performed by laparoscopy is feasible and safe and had comparable results to open surgery with less post-operative discomfort and infection. A meta-analysis showed 85% success [11, 12]. In the laparoscopy approach, there was an increased rate of re-operation for leakage. This may be due to difficulty in the laparoscopic suturing procedure and the learning curve required.
In conclusion, when traumatic gastric injuries occur, accurate diagnosis and timely surgical intervention are crucial to improve the prognosis of these patients. The delay in the approach to patients with traumatic gastric injuries increases morbidity and mortality, which can reach up to 66% [11].
CONFLICT OF INTEREST STATEMENT
All authors declare no personal, professional or financial conflicts of interest. Patient consent was obtained for publication of the case details.
FUNDING
No funding/support was present in this case report.



