-
PDF
- Split View
-
Views
-
Cite
Cite
Alexandra C Skoczek, Dennis L Fernandez, Xanthogranulomatous appendicitis diagnosed on routine PET scan: a case report, Journal of Surgical Case Reports, Volume 2022, Issue 10, October 2022, rjac482, https://doi.org/10.1093/jscr/rjac482
Close - Share Icon Share
Abstract
Xanthogranulomatous appendicitis (XGA) is a rare process affecting the appendix vermiformis. Due to the atypical presentation of XGA, it is most commonly diagnosed post operatively on surgical pathology and is associated with interval appendectomies. Here, we describe a rare case of XGA diagnosed on pathology after acute appendicitis was found on routine Positron emission tomography scan for a minimally symptomatic patient with stage IV adenocarcinoma of the lung. Further prospective studies are required to evaluate the atypical presentation of XGA and the use of interval appendectomies following acute appendicitis diagnosis.
INTRODUCTION
Xanthogranulomatous inflammation (XGI) is a rare inflammatory response that appears on histology as foamy macrophages with activated plasma cells, lymphocytes, neutrophils and other multinucleated giant cells [1]. Although the most common organs to be affected by XGI are the kidney and gallbladder, XGI has been seen in the appendix, stomach, colon and other gastrointestinal organs [1, 2]. Although acute appendicitis is relatively common, xanthogranulomatous appendicitis (XGA) is uncommon and rarely reported in literature. XGA presents a diagnostic challenge due to the lack of radiographic ways to diagnose XGA and is diagnosed on pathology post appendectomy [2, 3].
Chemotherapy-induced peripheral neuropathy (CIPN) can further complicate an appendicitis diagnosis due to delayed presentation secondary to reduced pain sensation. CIPN is most often induced by platinum-based antineoplastic agents, vinca alkaloids, taxanes, epothilones, kinase inhibitors (KIs), proteasome inhibitors and thalidomide [4–6]. In the following case, we describe a presentation of asymptomatic acute appendicitis that was found on routine Positron emission tomography (PET) scan for a patient undergoing cancer treatment with Alectinib and Denosumab that on post operative pathology was found to be XGA.
CASE REPORT
A 56-year-old male with a medical history of stage IV metastatic adenocarcinoma of the lung presented to the emergency department with acute appendicitis found on routine PET scan. The patient had a routine PET scan done that morning that showed new intense activity in the right lower quadrant (RLQ) inseparable from the cecum and appendix which was worrisome for acute appendicitis (Fig. 1). The patient reported minimal nausea and mild achy abdominal pain for the last 10 days; however, he had not sought treatment due to the mild nature of the pain. The patient denied any other symptoms including vomiting, fever, anorexia or bowel changes. The patient was taking Alectinib and Denosumab for cancer treatment and was known to have metastases to the axial and appendicular skeleton.
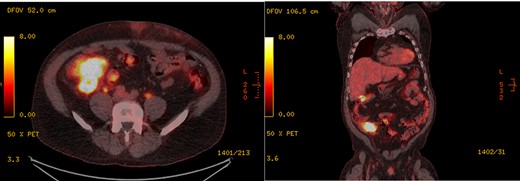
PET scan showing intense activity in the RLQ inseparable from the cecum and appendix, found to be acute appendicitis with XGI on histopathology of appendix specimen, in (left) axial section and (right) coronal section.
On presentation to the emergency department, the patient was in no acute distress with vitals all within normal limits. Abdominal exam was unremarkable except a potential mass found on deep palpation of the RLQ. There was negative McBurney’s point tenderness and Rosving’s sign was negative. White cell count was 11.2 × 109 cells/L and electrolytes were within normal limits. The patient was admitted to the hospital and started on IV Piperacillin/Tazobactam and surgery was planned for the following day.
The patient was taken to the operating room the following day for a laparoscopic appendectomy. Intraoperative findings included a notable phlegmon along the right pericolic gutter in the area of the proximal cecum and the terminal ileum. There was significant induration to the cecum and terminal ileum making dissection difficult so the decision to convert to an open procedure was made. Due to the phlegmon and significant induration, the appendix, cecum and a portion of the terminal ileum were resected, and an anastomosis created. Histopathology of the appendix demonstrated abscess formation and reactive fibrosis with XGI. The patient was subsequently discharged from the hospital and had no post operative complications.
DISCUSSION
XGI is a rare inflammatory disease that can elicited by any activation of the immune response such as phlegmon, abscess, hemorrhage or necrosis. Chronic XGI on histology demonstrates lipid laden macrophages and acute and chronic inflammatory cells [1]. A 10-year study by Laishram et al. determined that XGI has a total incidence of 1% with a 0.25% incidence of XGA [7].
Clinically and radiographically XGA can mimic neoplastic and other inflammatory processes and presents a diagnostic challenge to practitioners [2, 3]. XGI of the lower gastrointestinal tract usually presents with nausea, anorexia, fever, bowel changes and abdominal pain [8]. In the present case, majority of these symptoms were not seen on presentation to the emergency department. Noninvasive diagnostic testing revealed an area of new intensity in the RLQ which was assumed to be acute appendicitis; however, due to the patient’s history of metastatic cancer, a neoplastic mass must be ruled out. Therefore, an appropriate surgical approach followed by pathologic diagnosis is required.
In patients who present with appendiceal phlegmon or abscess, there is a debate between interval appendectomy or immediate surgery [9]. Recent recommendations suggest non-operative management with antibiotics and percutaneous drainage when laparoscopic surgery is not available [9]. In this case, abscess formation and chronic inflammation may have led to XGI.
It must also be noted that the patient in this present case was undergoing cancer treatment with Alectinib and Denosumab, which have been shown to cause CIPN [4–6]. CIPN can affect large and small fiber nerves, sensory and/or motor nerves, demyelinating axonal nerves and autonomic nerves [6]. Small Aδ-fiber nerves are responsible for the visceral pain sensation that would be felt in acute appendicitis [10]. The patient’s chemotherapy regimen could have decreased their pain sensation and clinical presentation, causing a delay in treatment, which led to chronic inflammatory changes.
In summary, we present a rare case of XGA that was found on routine noninvasive imaging. Chemotherapy may have played a role in delayed acute appendicitis treatment leading to a chronic inflammatory response. There are limited data and reporting on XGA is therefore unclear if the delayed presentation led to the progression to XGA. There is also a debate on the use of interval appendectomies for acute appendicitis and further studies will be required to establish a link between delaying surgery and chronic inflammatory complications.
ACKNOWLEDGEMENTS
Special thank you to Crestwood Medical Center and Dr Dennis Fernandez, MD, for providing the opportunity to work on this case and create a case report on this rare and interesting pathology.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



