-
PDF
- Split View
-
Views
-
Cite
Cite
Junepill Seok, Postoperative submuscular emphysema due to air leakage from the residual screw holes after plate removal in a patient who had undergone surgical stabilization of flail chest, Journal of Surgical Case Reports, Volume 2022, Issue 10, October 2022, rjac459, https://doi.org/10.1093/jscr/rjac459
Close - Share Icon Share
Abstract
Many studies have reported indications and complications of surgical stabilization of rib fractures. However, data about the postoperative complications after the removal of the plates are still lacking. The author reports a rare complication after plate removal, postoperative submuscular emphysema, due to air leakage from the residual screw hole. A 68-year-old male with a flail chest was successfully treated by surgical rib fixation. A few months later, the patient wanted his implants removed due to chest irritation. The removal operation was completed, and postoperative courses were not unusual. However, a large amount of submuscular emphysema was found in the follow-up period. The patient was successfully managed by applying a submuscular thoracic drainage catheter. Although postoperative subcutaneous emphysema due to residual screw holes after plate removal is rare, we need to pay more attention when selecting the proper length of screws during surgical rib fixation.
INTRODUCTION
Many studies have reported indications and complications of surgical stabilization of rib fractures (SSRF) [1–5]. However, data about the postoperative complications after the removal of the plates are still lacking. The author reports a rare complication after plate removal, postoperative submuscular emphysema, due to air leakage from the residual screw hole.
CASE REPORT
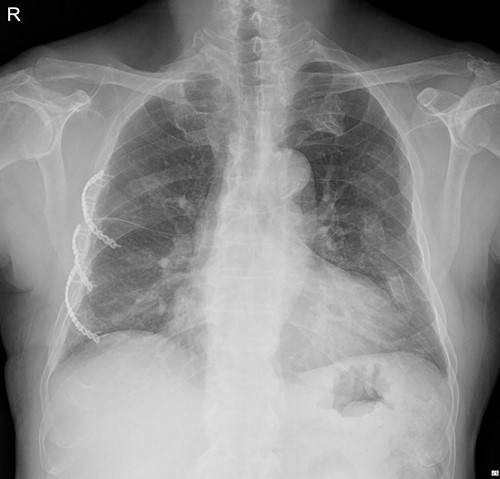
On 25 November 2021, a 68-year-old male, a victim of a motor vehicle accident, presented with multiple rib fractures and hemopneumothorax in the right hemithorax. On hospital Day 2, oxygen saturation gradually dropped under 90% despite proper support, and the patient’s right chest wall showed a newly occurred flail motion. We decided to stabilize rib fractures emergently. The operation was performed routinely, with bicortical screw fixation after exploration of the thoracic cavity. There were no specific intraoperative or postoperative events, and the patient was safely discharged from the hospital with stitches removed on hospital Day 17 (Fig. 1.).
The outpatient course was not unusual. Like many other patients who underwent SSRF, the patient complained of mild chest irritation related to the SSRF. To reduce the patient’s discomfort, we decided to remove the implants at least 3 months after the operation day of SSRF, when bony healing would be sufficiently achieved.
The patient underwent plate removal surgery on 24 February 2022. The operation was performed routinely. Under general anesthesia, a small incision was made on the previous operation scar. After sufficiently dissecting surrounding tissues and muscles, we skimmed implants off the rib cage. Then, a seven-French sizes (FR) drainage catheter was placed below the serratus anterior muscle (SAM) to manage potential minor complications. Because we usually do not invade the rib cage during plate removal operations, there was no need to be concerned about lung injury. The patient was discharged on hospital Day 2 with the submuscular drainage catheter removed (Fig. 2.).

Immediate postoperative chest X-ray after plates removal (24 February 2022).
The patient visited the outpatient clinic on 07 March 2022, for stitches removal, complaining of mild discomfort on the operation site (Fig. 3.). Chest X-ray showed a large, localized submuscular emphysema between the rib cage and the SAM. The surgical wound was clear. Stitches were removed as planned, and the patient was asked to revisit the outpatient clinic 3 days later.
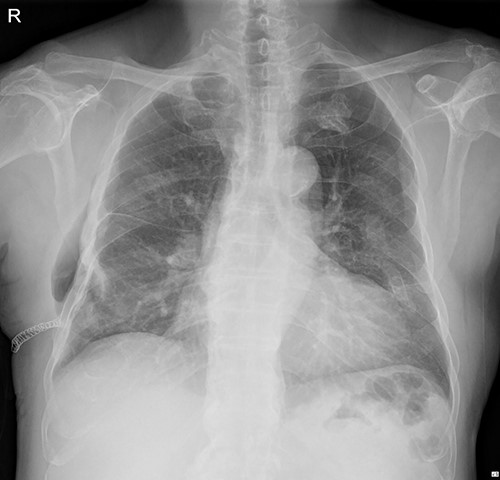
The submuscular emphysema, however, was increased in size, and the patient was eventually re-hospitalized. A small incision was made beneath the surgical wound under local anesthesia, and a 10 FR thoracic drainage catheter was carefully placed into the submuscular layer (Fig. 4.). Under 2 L of oxygen supplement, the submuscular emphysema gradually decreased over several days, and the patient was finally discharged on hospital Day 6 (Fig. 5). Since his last readmission, there have not been any more complications.

Chest X-ray after applying a 10 FR drainage thoracic catheter into the submuscular layer (11 March 2022).

DISCUSSION
Only a few studies mentioned postoperative complications after plate removal [4], and only one study compared which technique would be superior between unicortical and bicortical screw fixation during SSRF. However, the study was carried out with fully frozen cadaveric ribs [6]. Most patients who underwent SSRF face a harsh situation right after the surgery. They must keep moving their surgically fixated ribs to breathe without external supports such as splints or braces. Because surgically fixated ribs have to maintain relative stability in the bone-healing period [7], frozen and stiffed ribs are not acceptable in this situation.
Screw fixation techniques are relatively well-standardized in orthopedic medicine. However, those during SSRF are not standardized and primarily dependent on the surgeon’s experiences due to a lack of rationale. Our principles are not much different from a former report [8]. We mostly prefer bicortical screw fixation and try to maintain the relative stability of the fractured ribs by emptying two holes adjacent to the fracture line. The proper length of the screw is selected before screwing so that the protruding screw tip would not exceed 1 mm. In this way, we have minimized potential risks and never experienced complications related to the bicortical technique before this case report. At the hospital with which the author is currently affiliated, 41 patients with flail chest underwent SSRF from January 2021 to August 2022. None of them had suffered ‘theoretically possible’ complications from protruding screw tips by the bicortical screw fixation technique. In this period, 13 removal operations were performed. Except for this case report, none had experienced complications after removal operations.
In this case, there had been no unexpected intraoperative event such as penetrating the chest wall with a driver while removing screws or lung exposure by accident. Also, postoperative wound management was faultless. However, the patient complained of an enlarging mass on the operation site after removing plates and screws. The submuscular emphysema – in other words, pneumothorax – did not have any chance that it originated outside the chest wall. The author concluded that the only possible scenario was that there might be a minor air leakage through the residual screw holes after the removal of screws. To avoid re-open the operation scar, the author decided to apply a thoracic drainage catheter into the submuscular later. As a result, the patient was successfully treated and discharged.
Despite this case report, we do not consider changing surgical principles from bicortical to unicortical screw fixation. A recent study reported that among 103 patients who underwent SSRF, 48 (48%) patients complained of chest wall discomforts, and 9 (9%) patients had removed their implants [4]. The author has experienced >200 cases of SSRF over 10 years, and about 30% of them had removed their plates and screws. Few of them had suffered from minor postoperative hematoma or wound dehiscence, but none had shown this kind of complication.
In conclusion, postoperative subcutaneous emphysema due to residual screw holes after plates and screws removal is extremely rare, and it would be easily managed. Theoretically, the unicortical screw fixation technique may reduce potential complications compared with the bicortical approach, but the data are insufficient. Although this complication is not common, we need to pay more attention when selecting a proper length of screws during SSRF, especially when bicortical screw fixation.
ACKNOWLEDGMENTS
Junepill Seok is the sole author and has worked with faculty in the admission and care of this patient.
CONFLICT OF INTEREST STATEMENT
The author declares no conflict of interest.
FUNDING
The author declares that this report has received no financial support.



