-
PDF
- Split View
-
Views
-
Cite
Cite
Hani Alkhulaiwi, Faisal H Alsarrani, Alanood A Alharbi, Duodenal transection following blunt abdominal trauma: a case report and literature review, Journal of Surgical Case Reports, Volume 2022, Issue 10, October 2022, rjab610, https://doi.org/10.1093/jscr/rjab610
Close - Share Icon Share
Abstract
Isolated duodenal transection—a rare complication of abdominal trauma—is a challenging dilemma and difficult to diagnose. As blunt duodenal injuries vary from mild hematoma or perforation to complete transection or complex pancreaticoduodenal disruption. A 21-year-old male medically free victim of motor vehicle collision was admitted to our hospital and evaluated in ER according to ATLS protocol. Patient was stable with positive fast scan so we proceeded for abdomen computed tomography, which showed duodenal injury with possible pancreatic transection and active arterial extravasation. Based on that patient was taken for exploratory laparotomy and primary repair. Duodenal injuries can be a result of different mechanism. Typically, it was the result of crush injury, however, it can be due to shear or bursting forces. With its anatomical location, reaching the accurate diagnosis might be delayed, which is associated with higher mortality rate. Due to different scales of severity and different presentation, the management varies based on the location and the involved surrounding structures. Although complete duodenal transection is rare with blunt injuries, high clinical suspicion is necessary to detect such injury early. Studies have shown that the outcomes are highly dictated by early diagnosis and prompt management.
INTRODUCTION
Isolated duodenal transection (IDS)—a rare complication of abdominal trauma—it has a prevalence of <20% following blunt duodenal injuries [1–5].
It is well known that early intervention in duodenal injuries improves the overall outcomes [6]. Numerous treatment modalities and techniques have been described in the literature [7–9].
CASE REPORT
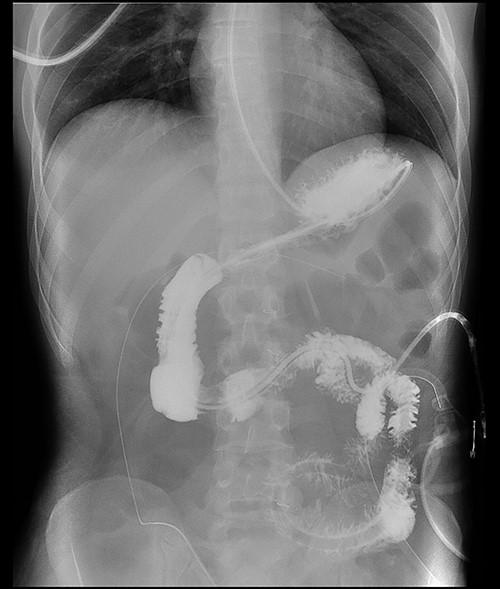
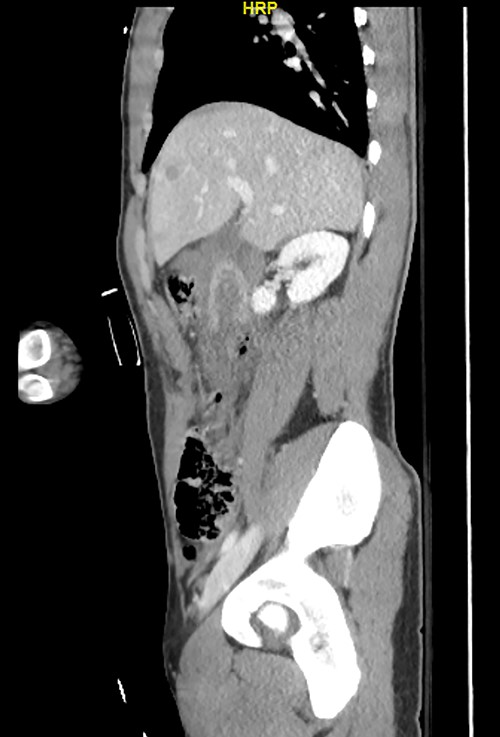
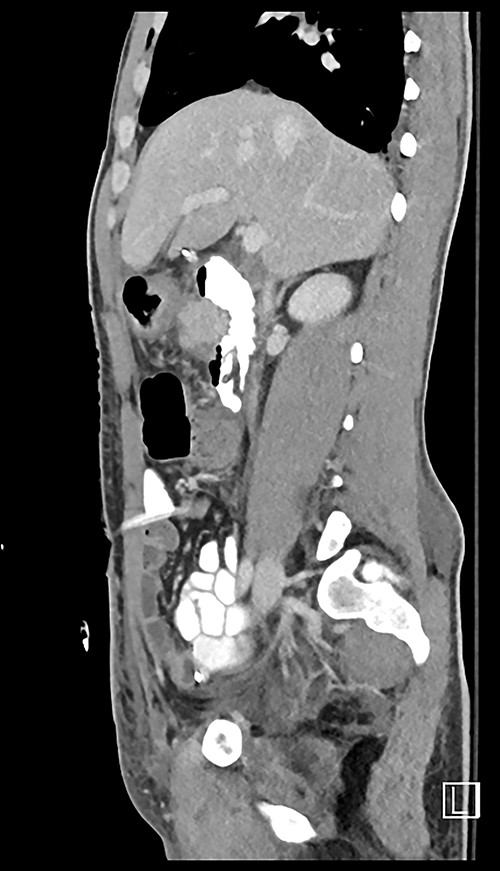
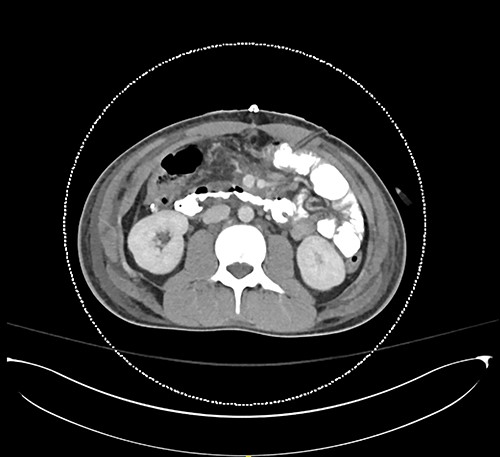
Here, we report a case of a 21-year-old man who was admitted to our hospital following a motor vehicle collision where he was a pedestrian, hit by a car and pushed against the bumper of another car. Upon arrival to the hospital, he was conscious and oriented, with normal vital signs. Abdominal examination revealed ecchymosis over the epigastric area with tenderness, however, no distention was noticed. Focused assessment with sonography for trauma result was positive in the right upper quadrant. His initial blood test results revealed a white blood cell (WBC) count of 26.5 × 109 cells/l and a hemoglobin level of 150 g/l. His serum amylase and lactic acid levels were 92 U/l and 4.53 mmol/l, respectively. His base deficit was 4.3. He underwent abdominal computed tomography (CT) with oral contrast, which showed query duodenal and possible pancreatic transection with active arterial extravasation (Figs 1–3). In addition, CT revealed a comminuted right intertrochanteric femoral fracture without associated vascular injury.

Exploratory laparotomy was performed, which revealed ~500 ml of blood in the peritoneal cavity, central retroperitoneal hematoma, peripancreatic hematoma and complete transection of the third part of the duodenum. The retroperitoneal hematoma and peripancreatic hematoma were nonexpanding. A formal end-to-end anastomosis of the third part of the duodenum was performed using 3–0 polydioxanone (PDS) in a single layer. Double decompression of the duodenum was achieved using a nasoduodenal tube (ND) and a retrograde duodenostomy tube. A jejunostomy tube was created for feeding as well.
Postoperatively, the ND and retrograde duodenostomy tubes were maintained on continuous suction. Feeding through jejunostomy tube was initiated on postoperative Day 2, and the ND tube was removed on postoperative Day 23 when oral feeding was initiated. Although postoperative CT and Gastrografin swallow confirmed good anastomosis without evidence of leaks (Figs 4–7), The prolonged hospital stay and the delays in removing ND tube and initiation of the oral intake was because of persistent sepsis and high WBC counts, which was later confirmed to be secondary to abscess in his right thigh.


His blood test results at discharge revealed a WBC count of 6.32 × 109 cells/l and a hemoglobin level of 113 g/l. His serum amylase and lactic acid levels were 85 U/l and 0.84 mmol/l, respectively.
After a few months of follow ups, he developed a mild annular duodenal stricture was successfully managed with duodenal dilation, he was seen 24 months after discharged in the clinic. He had smooth recovery with good appetite and reasonable weight gain.
DISCUSSION
Early diagnosis of duodenal injury is essential as any delay in treatment may influence morbidity and mortality. If surgical intervention is delayed beyond 24 h, the mortality rate increases from 11 to 40% [10]. The mortality rate is higher in cases of combined pancreaticoduodenal injury [2]. There are few important clues that can help in the diagnosis of duodenal injuries. These clues can be obtained by focusing on detailed history of the injury, including the mechanism of injury and a meticulous physical examination [1]. However, physical examination may be initially misleading as early manifestations of duodenal injury may be hindered by its retroperitoneal location. Certain clinical findings, such as tachycardia, fever, right upper quadrant pain and vomiting should raise suspicion of duodenal injury [4]. In the presented case, the signs and symptoms of duodenal injury were subtle on arrival to the hospital, and the patient was conscious and oriented. Furthermore, he was hemodynamically stable. The physical examination was not conclusive, except for several bruises over the epigastrium. However, the mechanism of injury and CT findings lead to early diagnosis and surgical intervention.
Despite its limitations in distinguishing between duodenal hematoma and duodenal perforation, CT with intravenous and intraluminal contrast remains the gold standard diagnostic test in stable patients with blunt abdominal trauma [1]. In the reported case, CT revealed duodenal and possible pancreatic transection with active arterial extravasation.
Many surgical techniques have been described in the literature for duodenal injuries. Primary repair with pyloric exclusion + Gastrojejunostomy to protect the repair is well known and safe option especially in the presence of contamination. There are some reported cases of primary repair with gastrostomy, cholecystostomy and decompressive duodenostomy tube. In some cases of severe pancreaticoduodenal injuries pancreaticoduodenectomy [7] might be the definitive treatment.
Based on these reports, we can understand that the majority of the patients with duodenal injury underwent exploratory laparotomy and were managed according to the severity of the injury to the duodenum and the associated injuries to other intra-abdominal organs. The surgical options for complete transection of the duodenum include formal end-to-end anastomosis with decompression or pyloric exclusion. Roux-en-Y duodenojejunostomy with closure of the distal duodenal stump is an alternative option that has not been widely accepted among surgeons [11].
Our patient was young and hemodynamically stable. He had an isolated injury to the third portion of the duodenum with complete transection (Grade 4). There was no gross contamination in the abdomen and the surgical intervention was immediate (within 24 h of the time of injury). In addition, the two edges were well-vascularized, Heathy with good blood supply. There were minimal devitalized tissues at the edges, which were debrided. The two segments of the duodenum were reasonably mobile and not under tension. Therefore, we decided to do single layer primary end-to-end anastomosis with double decompression tubes. A jejunostomy tube was created for feeding, and octreotide was administered postoperatively and continued for 2 weeks.
CONCLUSION
Early diagnosis and intervention are essential. Early proper history of the mechanism of injury, physical examination and radiological imaging modalities such as CT are of great value to detect such injuries earlier, which significantly affects the outcome in these patients.
AUTHORS’ CONTRIBUTIONS
Each author contributed to writing, reviewing the paper and agreed on submission.
CONFLICT OF INTEREST STATEMENT
None declared.
References
- computed tomography
- hematoma
- abdominal injuries
- traffic accidents
- extravasation of diagnostic and therapeutic materials
- nonpenetrating wounds
- abdomen
- diagnosis
- duodenum
- mortality
- pancreas
- crushing injuries
- focused assessment with sonography of trauma
- duodenal injuries
- laparotomy, exploratory
- advanced trauma life support
- blunt abdominal injuries
- early diagnosis
- weight measurement scales



