-
PDF
- Split View
-
Views
-
Cite
Cite
Mark Redden, Andrew Riddell, Acute presentation of multi-cystic peritoneal mesothelioma, Journal of Surgical Case Reports, Volume 2022, Issue 1, January 2022, rjab627, https://doi.org/10.1093/jscr/rjab627
Close - Share Icon Share
Abstract
Multi-cystic peritoneal mesothelioma (MCPM) is a rare intra-abdominal neoplasm that occurs most commonly in young females. The disease usually presents as an incidental finding or with sub-acute abdominal pain. The mainstay of treatment is complete excision; however, local recurrence frequently occurs and malignant transformation has been reported. We describe a unique case of MCPM that presented with acute abdominal pain.
A 32-year-old female presented with a 24-hour history of abdominal pain. Computed tomography abdomen demonstrated a low-density mass with surrounding inflammatory changes anterior to the ascending colon, which was initially thought to represent an abscess. A percutaneous drain was inserted; however, only clear fluid was aspirated and the lesion did not resolve. The patient subsequently underwent laparoscopy which identified a cystic structure overlying the ascending colon. The structure was excised whole with histology demonstrating MCPM. The patient recovered from surgery and will undergo a period of surveillance.
INTRODUCTION
MCPM is a rare neoplasm arising from the mesothelial cells of the peritoneum [1]. The pathophysiology is unclear; however, it most commonly occurs in young women and there is an association with endometriosis and previous surgery [2]. Approximately 150 cases have been reported globally [1]. MCPM usually presents with sub-acute abdominal pain or as an incidental finding and most commonly involves the pelvic peritoneum [1]. Complete excision is the mainstay of treatment but local recurrence is common [1]. Cytoreductive surgery combined with hyperthermic intra-peritoneal chemotherapy (HIPEC) may be effective in such cases [3]. A total of 1 death has been reported in a patient who declined further treatment after local recurrence [1]. We present a case of MCPM overlying the ascending colon which presented with acute abdominal pain.
CASE
A 32-year-old female presented to the emergency department with right lower quadrant abdominal pain. The pain had started suddenly 1 day prior, and there were no other associated symptoms. The patient's medical history included a laparoscopy for endmetriosis, cholecystectomy and hysterectomy. Her vital signs were normal and on examination there was abdominal tenderness in the right lower and right upper quadrants.
The white cell count was 10.5 × 109/l, C-reactive protein 6.8 mg/l, B-hCG negative, urine culture negative. Ultrasound (US) abdomen did not identify the appendix or the right ovary but noted a 102 × 43 × 52 mm complex multi-locular cyst. Computed tomography (CT) abdomen showed a focal low-density mass with adjacent inflammatory change anterior to the ascending colon measuring 43 × 55 × 54 mm (Figs 1–3). This mass appeared separate to the ovary and the appendix.

Axial CT demonstrating mass anterior to ascending colon with surrounding inflammatory changes.
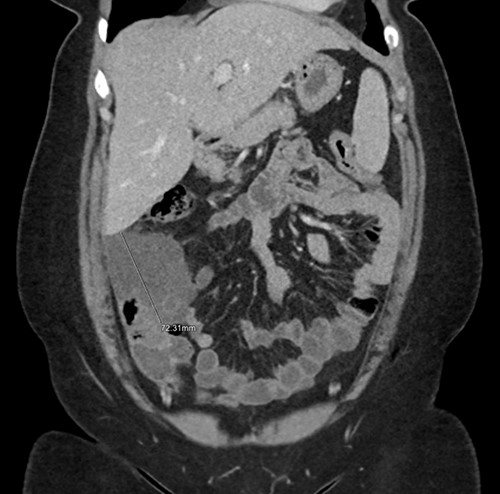
Coronal CT reconstruction measuring the largest dimension of mass.

Sagittal CT reconstruction highlighting location of mass anterior to ascending colon.
Given the inflammatory changes on imaging, it was thought that the lesion represented an abscess. A percutaneous drain was inserted under US guidance. Clear fluid was aspirated from the lesion and sent for analysis. M/C/S showed no growth. Cytology did not identify malignant cells. Tumour markers, carcinoembryonic antigen and CA19.9 were normal.
The patient’s symptoms improved, and she was discharged with outpatient follow-up. A subsequent CT abdomen 1 month later showed that the lesion remained unchanged. The patient then proceeded to diagnostic laparoscopy that revealed a multi-cystic structure overlying the distal ascending colon and hepatic flexure. The lesion was adherent to the epiploic appendages of the colon and in places was continuous with the omentum. The structure was dissected and removed whole (Fig. 4). Histology of the lesion demonstrated MCPM. The patient recovered from surgery well and will undergo a period of surveillance for return of her symptoms.

DISCUSSION
MCPM usually presents as an incidental finding or with sub-acute symptoms that are related to the mass such as abdominal discomfort and dyspareunia [2]. This case is unique due to the acuity of the presenting pain. This, combined with the inflammatory changes on imaging, presented a diagnostic challenge and suggested a more acute entity. The most likely diagnosis was an abscess related to various pathologies including appendicitis. For this reason, the lesion was initially treated with percutaneous drainage. Persistent symptoms and non-resolution of the structure on imaging then prompted surgical intervention.
MCPM has a strong association with previous surgery and endometriosis, which is consistent with this patient’s history. The association suggests that MCPM may be a reactive process secondary to chronic irritation [2]. This is further reinforced by the occasional finding of endometriosis within MCPM cyst walls [2]. Other reported pre-disposing factors include peritoneal dialysis and recurrent episodes of peritonitis [2].
Local recurrence is common after excision of MCPM, occurring in up to 50% of patients [3]. Additionally, transformation to malignant mesothelioma has been reported [4, 5]. Clearly, a period of clinical surveillance is necessary after resection. However, there is currently no consensus regarding optimum surveillance intervals and whether routine imaging should be performed.
Cytoreductive surgery with hyperthermic intraperitoneal chemotherapy (HIPEC) treatment for MCPM has been reported with some possible improvement in outcomes. Nizri et al. reported a series of 19 patients with histologically proven MCPM that underwent this treatment. With a median follow-up of 69 months, all patients were alive and only 21% had recurrence [3]. To date, there have been no randomized control trials comparing treatment modalities. Given the low prevalence of this disease, prospective trials will prove difficult to coordinate.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
FUNDING
None.



