-
PDF
- Split View
-
Views
-
Cite
Cite
Wan Amir Wan Hassan, Vignesh Narasimhan, Asiri Arachchi, Thomas Manolitsas, William Teoh, Small bowel evisceration from vagina, Journal of Surgical Case Reports, Volume 2021, Issue 8, August 2021, rjab343, https://doi.org/10.1093/jscr/rjab343
Close - Share Icon Share
Abstract
Vaginal evisceration is a rare condition where abdominal contents herniate through a vaginal wall defect. The estimated incidence is 0.032–1.2% after hysterectomy, trachelectomy or upper vaginectomy. We present a 78-year-old lady who developed vaginal evisceration 2 years after radical cystectomy and hysterectomy for bladder cancer. It is rare surgical emergency that requires prompt recognition and damage control with bowel reduction and packing. We discuss the initial management and surgical options for definitive repair.
INTRODUCTION
Vaginal evisceration is a rare surgical emergency. We present a 78-year-old lady who developed vaginal evisceration 2 years after radical cystectomy and hysterectomy for locally advanced bladder cancer.
CASE REPORT
A 78-year-old lady developed sudden onset severe vaginal pain during her morning walk. On self-examination, she noted some vaginal bleeding and loops of bowel protruding out from her vagina. She was taken to the local emergency department, where the bowel prolapse was reduced with vaginal packing (Fig. 1). She was given intravenous antibiotics and subsequently emergently transferred to a tertiary centre.

Vagina introitus with packing material reducing the small bowel evisceration.
Her past history was significant for a locally advanced bladder cancer treated with a radical cystectomy, hysterectomy and ileal conduit 2 years ago, with subsequent adjuvant chemoradiation. Following her surgery, she had known vaginal prolapse that had recurred despite treatment with a pessary. She was currently on immunotherapy treatment for stable, low-volume lung and liver metastases.
On examination, she was haemodynamically stable and had generalized mild abdominal pain. She had not passed any flatus or opened her bowels for 24 h, which was when the bowel evisceration occurred. Laboratory findings revealed mild leucocytosis of 11.9 × 109/L (normal 4.0–11.0), elevated C-reactive protein of 31 mg/L (normal <5) and a normal lactate of 0.4 mmol/L (normal <0.5).
Computed tomography scan of the abdomen revealed small volume of free fluid and inflammatory fat stranding in the pelvis with loops of thick-walled distal small bowel. Packing material was seen in the vaginal vault (Fig. 2a and b).
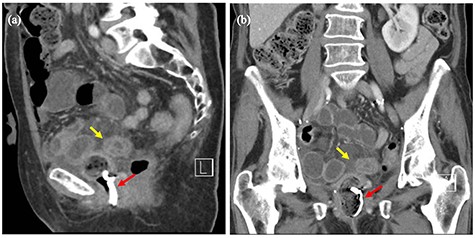
(a and b) Computed tomography images of the pelvis before surgery. Red arrows showing packing material in the vaginal vault. Yellow arrows showing loops of thick-walled distal small bowel.
At operation, the vaginal packs were removed and the bowel had been successfully reduced. There was a palpable defect in the superior vaginal vault, just posterior to the pubis, which prolapsed out easily, bringing the vaginal defect into view (Fig. 3a). There was a small amount of simple serous fluid, with no evidence of blood stained or purulent fluid. As tissue quality was good, the defect was primarily repaired with continuous 0 Vicryl (Fig. 3b).
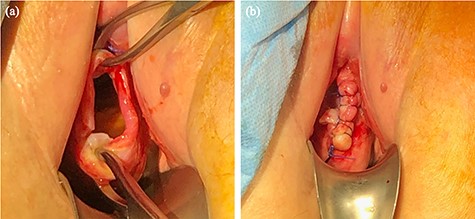
(a) Vagina introitus after removal of packing material. A prolapsed vaginal vault with a defect demonstrated. (b) Vaginal vault defect repaired with continuous 0 Vicryl.
Her post-operative course was unremarkable, and she was discharged home after return of normal bowel function with regular topical oestrogen cream. She is due to follow-up with gynaecology to discuss other options to treat her vaginal prolapse.
DISCUSSION
Vaginal evisceration is a rare condition where abdominal contents herniate through a vaginal wall defect. The estimated incidence is 0.032–1.2% after hysterectomy, trachelectomy or upper vaginectomy [1–3]. Predisposing risk factors include hypo-oestrogenic state in post-menopausal women, known vaginal prolapse, previous vaginal surgery, and prior pelvic radiation [1, 3, 4].
Although the most frequently prolapsed organ is the distal ileum, there have also been reports of omentum, appendix and fallopian tube being involved. Early intervention is critical, as up to a third of small bowel evisceration cases may be complicated by bowel ischaemia.
The key principle of early management involves an attempt to gently reduce the bowel into the peritoneal cavity, and packing the vagina with moistened gauze. If the bowel is unable to be reduced, it should be covered with moist gauze before definitive surgery [1, 3].
Given the rarity of this condition, there is no consensus on the optimal operative approach for vaginal cuff dehiscence and each case should be treated on its own merits [2–4]. Surgical treatment can be transabdominal, transvaginal or both based largely on the expertise available and the clinical situation of the patient.
Transvaginal approach is generally believed to be the least morbid, with primary closure of the vaginal vault if the tissue is healthy. Transabdominal assessment can be via laparoscopy or laparotomy, with repair of the vaginal vault essential to prevent recurrence [1–3, 5]. The use of mesh or omental flap to re-enforce the vaginal vault can be utilized based on the clinical situation [6, 7].
As our patient did not present with overt signs of bowel ischaemia, we opted for a transvaginal repair with the aim to proceed to laparotomy if unsuccessful. It is likely that a combination of the various risk factors led to her vaginal cuff breakdown. Despite the previous pelvic radiation, she had very good quality tissue, and hence a robust primary closure was performed.
This case highlights a rare surgical emergency that requires prompt recognition and damage control with bowel reduction and packing. Definitive repair can then be performed once appropriate expertise is available.
CONFLICT OF INTEREST STATEMENT
None declared.
CONSENT
Patient has provided informed consent for this case to be published.



