-
PDF
- Split View
-
Views
-
Cite
Cite
Koji Matsushita, Nobumi Tagaya, Ryuichirou Nakajima, Masayuki Yagi, Yuichi Obana, Yuhei Nakano, Junpei Suzuki, Masako Mizoguchi, Yukino Yoshimura, Takashi Arai, Yako Hasegawa, Junichi Suzuki, Kyokun Haku, Toshifumi Arai, Tetsuya Kurosaki, Kazuyuki Saito, Three millimeter needlescopic splenectomy using three-port technique: report of three cases, Journal of Surgical Case Reports, Volume 2021, Issue 8, August 2021, rjab305, https://doi.org/10.1093/jscr/rjab305
Close - Share Icon Share
Abstract
We report our experience with needlescopic splenectomy (NS) for the surgical treatment of idiopathic thrombocytopenic purpura using a 3-mm needlescope with three ports. One patient was male and two were females, and their mean age was 58 years. The patient was placed in the right lateral decubitus position. The first 12-mm port was introduced through the lateral margin of the left rectus abdominis muscle, and the other two 3-mm ports were inserted in the left upper quadrant. NS was performed by a standard technique under the observation of 3.3-mm needlescope. The surgical procedure was successfully completed in all the patients. The mean duration of surgery, intra-operative bleeding volume and post-operative hospital stay were 176 min, 70 ml and 4.7 days, respectively. There were no particular peri-operative complications in spite of dense adhesions or simultaneous laparoscopic procedures. Our method is safe and feasible with low morbidity and without impairing cosmetic benefits.
INTRODUCTION
A laparoscopic approach is often used for the surgical treatment of idiopathic thrombocytopenic purpura (ITP) to improve the cosmetic result and post-operative quality of life of the patients. Furthermore, needlescopic splenectomy (NS) [1] has developed as a result of advancements in minimally invasive surgery. However, 2-mm needlescopic procedures have not been widely adopted because of some instrument features such as easy bending of the shaft, poor scope visualization and weak manipulation [2]. Therefore, we introduced 3-mm needlescopic devices to perform laparoscopic splenectomy. The indications for which the patients underwent splenectomy included no response to medical therapy, discontinuation of corticosteroid due to adverse effects, planning for pregnancy and absence of splenomegaly. Patients with high risk for general anesthesia and those with splenomegaly due to a high risk of splenic injury were excluded from the study. Platelet or gamma globulin was transfused pre-operatively to patients who had a platelet count of <5 × 104/ul. We report here that three cases of NS in whom a 3-mm needlescope with a three-port technique was used, and a detailed literature review.
CASE REPORT
Case 1
A 24-year-old female patient in whom ITP was diagnosed in March 2008, presented at our hospital. She had received a steroid pulse therapy; however, she did not respond to the treatment. The treatment was changed to oral prednisolone (30 mg per day). However, her platelet count remained unstable ranging from 1 to 4.8 × 104/ul. She was transfused with gamma globulin pre-operatively and underwent a NS in October 2013. The duration of surgery was 96 min and intra-operative blood loss was 80 ml. There were no peri-operative complications. She was discharged on post-operative day 3. The weight of the resected specimen was 110 g. Her post-operative platelet count was stable between 20 and 25 × 104/ul during 74 months after surgery.
Case 2
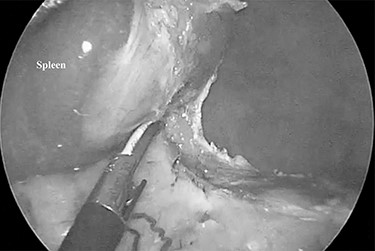
A 79-year-old female patient who had been diagnosed with chronic ITP in September 2014 presented at our hospital. She had received a combined therapy comprising prednisolone and thrombopoietin receptor agonist; however, her platelet count ranged from 0.5 to 59.9 × 104/ul and could not be controlled with oral therapy. Furthermore, she had comorbidities including hypertension, dyslipidemia and diabetes mellitus induced by pre-dnisolone, and a past history of cholecystectomy with an upper abdominal incision. She underwent NS in October 2015, and there were dense adhesions around the spleen supposing to the previous upper abdominal surgery (Fig. 1). The duration of surgery was 163 min and an intra-operative blood loss was 10 ml. Post-operative CT showed a low volume of ascites, which did not require further treatment. She was discharged on the post-operative day 9 with an extremely high her platelet count (135.2 × 104/ul). The weight of the resected specimen was 135 g. Her post-operative platelet count settled at around 45 × 104/ul during 54 months after surgery.

Dense adhesions around the spleen were divided under 3-mm needlescope.
Case 3
A 71-year-old male patient who had been diagnosed with ITP in August 2012 presented at our hospital. His past history included hemorroidectomy, varicose vein surgery and surgery for retinal detachment. He received pre-dnisolone therapy; however, the platelet count ranged between 1.6 and 23.9 × 104/ul. He underwent NS and cholecystectomy for a gallbladder stone in October 2015. One accessory spleen was also resected. Cholecystectomy was performed through a single-incision from the umbilicus. The duration of surgery was 269 min and an intra-operative blood loss was 120 ml. There were no peri-operative complications. He was discharged on post-operative day 5. The weight of the resected specimen was 115 g. His post-operative platelet count was stable at around 20 × 104/ul. Three months after surgery, he presented high fever and gait disorder, and several investigations revealed an Aspergillus infection and brainstem infarction. However, his symptoms deteriorated after readmission, and he developed pneumonia with pulmonary dysfunction and died from disseminated intravascular coagulation due to pneumonia 5 months after surgery.
Table 1 shows the summary of characteristics and surgical outcomes of the above three cases.
| No . | Age . | Gender . | Operation time (min) . | Blood loss (ml) . | Complication . | POHS (day) . | Follow-up (month) . | Outcome . | Other . |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 24 | F | 96 | 80 | none | 3 | 91 | Alive | |
| 2 | 79 | F | 163 | 10 | none | 9 | 71 | Alive | Previous upper abdominal surgery (cholecystectomy) |
| 3 | 71 | M | 269 | 120 | none | 5 | 5 | Dead (pneumonia) | Simultaneous cholecystectomy |
| No . | Age . | Gender . | Operation time (min) . | Blood loss (ml) . | Complication . | POHS (day) . | Follow-up (month) . | Outcome . | Other . |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 24 | F | 96 | 80 | none | 3 | 91 | Alive | |
| 2 | 79 | F | 163 | 10 | none | 9 | 71 | Alive | Previous upper abdominal surgery (cholecystectomy) |
| 3 | 71 | M | 269 | 120 | none | 5 | 5 | Dead (pneumonia) | Simultaneous cholecystectomy |
POHS: postoperative hospital stay
| No . | Age . | Gender . | Operation time (min) . | Blood loss (ml) . | Complication . | POHS (day) . | Follow-up (month) . | Outcome . | Other . |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 24 | F | 96 | 80 | none | 3 | 91 | Alive | |
| 2 | 79 | F | 163 | 10 | none | 9 | 71 | Alive | Previous upper abdominal surgery (cholecystectomy) |
| 3 | 71 | M | 269 | 120 | none | 5 | 5 | Dead (pneumonia) | Simultaneous cholecystectomy |
| No . | Age . | Gender . | Operation time (min) . | Blood loss (ml) . | Complication . | POHS (day) . | Follow-up (month) . | Outcome . | Other . |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 24 | F | 96 | 80 | none | 3 | 91 | Alive | |
| 2 | 79 | F | 163 | 10 | none | 9 | 71 | Alive | Previous upper abdominal surgery (cholecystectomy) |
| 3 | 71 | M | 269 | 120 | none | 5 | 5 | Dead (pneumonia) | Simultaneous cholecystectomy |
POHS: postoperative hospital stay
Surgical procedure of splenectomy
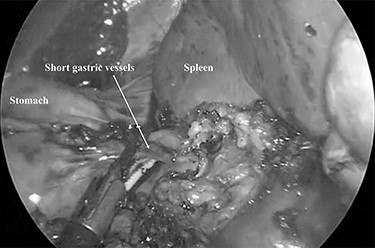
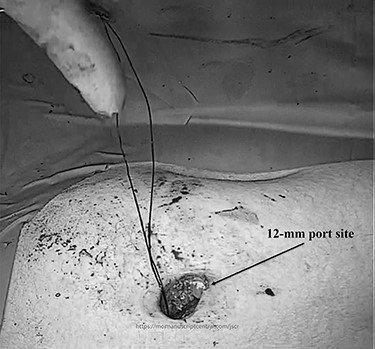
The patient was placed in the right lateral decubitus position. The standing positions of the surgeon and the assistant were on the right or left of the patient depending on the surgical site. Initially, a 12-mm port was introduced through the lateral margin of the left rectus abdominis muscle at the level of the umbilicus. After establishment of pneumoperitoneum with an intra-abdominal pressure of 10 mmHg, two 3-mm ports were inserted in the left upper quadrant at the subxiphoid and left subcostal margin along the mid-axillary line. The accessory spleen was carefully explored through the abdomen. The spleen was mobilized from the lower to upper direction. The initial dissection involved release of the lower pole of the spleen with dissection of the splenocolic ligament, and the spleen was freed from the splenorenal ligament toward the posterior aspect of the splenic hilus using laparoscopic coagulating shears under the guidance of a 3.3-mm needlescope (Karl Storz SE & Co. KG) (Fig. 2). Subsequently, short gastric vessels (Fig. 3) were divided, and the upper pole of the spleen was mobilized with the division of the splenophrenic ligament. Then, the splenic hilus was divided using a linear stapler (Fig. 4). The isolated spleen was then placed in an impermeable bag (Endo-Catch II; Covidien Co. Ltd.) and extracted via a 12-mm port after morcellation using the placenta forceps without extending the initial 12-mm incision (Fig. 5). After irrigation with normal saline and confirmation of hemostasis around the resected area without inserting a suction drain, only the 12-mm port site was only closed, and the 3-mm port sites were left open.
The spleen was freed from the splenorenal ligament using laparoscopic coagulating shears.
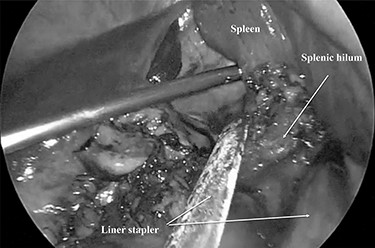
The splenic hilum was divided using an Endo-GIA linear stapler.
DISCUSSION
Minimally invasive abdominal surgery performed with needlescopic instruments leads to minimal surgical trauma to the abdominal wall, improved cosmetic result, reduced postoperative pain, lower incidence of wound complication, no risk of port site hernia and earlier recovery. Initially, we used of 2-mm needlescopic instruments for laparoscopic splenectomy (LS); however, the shaft easily bent when manipulating the organs, and there is a high frequency of a butting between the 2-mm needlescope and another forceps due to close proximity to the organs, with a narrow angle of surgical view [2]. Therefore, we utilized 3-mm instruments to overcome the restriction of surgical optics and maneuverability and provide better convenience for the surgeons. However, the risk of tissue damage by the pointed ends of fine graspers or splenosis [3] due to the capsular disruption of the spleen still remains. The dense intra-abdominal adhesions due to previous upper abdominal surgery as seen as Fig. 1 of Case 2 need careful dissection to prevent splenosis. This leads to a longer duration of surgery.
LS was generally performed using a four-port technique for NS as well. We performed NS using a three-port technique. To complete our technique, several skills including the intra-operative position of the patient to manipulate the spleen easily, mastering the technique that requires the use of both hands, and extraction of the spleen after morcellation using placenta forceps so as not to extend the initial 12-mm port site are necessary. The right lateral decubitus position tilts the spleen inward to divide the lateral side of the spleen. The technique using both hands provides an operative field similar to that created using the forceps of the assistant. Morcellation of the spleen using the placenta forceps prevents perforation of the impermeable bag due to its round shape. Not extending the 12-mm port incision as seen in Fig. 4 provides a better cosmetic outcome. There were no post-operative complications and there was no need to insert the suction drain. Confirmation of secure hemostasis during the surgery can achieve those outcomes.
Table 2 [1, 2, 4–6] shows the results of previous reports of NS; there was only one report (Backus CL et al. [5]) wherein a three-port technique was used. The authors described that the use of mini-laparoscopic instruments (2–3 mm in diameter) was safe and effective even in the presence of splenomegaly, and the post-operative cosmetic appearance was excellent. However, there are no reports about NS after 2002. We suspect that no developments of NS depend on the inconvenience of needlescopic instruments compared with those of recent high-quality images, 3-D images or robotic surgery. Therefore, we hope for an improvement in existing instruments and the development of new needlescopic instruments in the future. At this time, we think that the use of 3-mm instruments including a needlescope will achieve results similar to those with conventional LS.
| Author . | Year . | Case . | Port . | Operation time (min) . | Blood loss (ml) . | POHS (day) . | Complication . |
|---|---|---|---|---|---|---|---|
| Gagner M | 1998 | 5 | 12-2-2-2 | 90 | N/A | 1 | None |
| Yuan RH | 1998 | 2 | 12-2-2-2 | N/A | N/A | N/A | N/A |
| Backus CL | 2000 | 16 | 12-2-2 | 114 | 44 | 1.4 | None |
| Mamazza L | 2001 | 10 | 12-3-3-3 | 175 | N/A | 2.2 | Urinary retension: 1 |
| Postoperative bleeding: 1 | |||||||
| Tagaya N | 2002 | 3 | 12-2-2-2 | 167 | 70 | 5 | None |
| Our case | 2021 | 3 | 12-3-3 | 176 | 70 | 4.7 | None |
| Author . | Year . | Case . | Port . | Operation time (min) . | Blood loss (ml) . | POHS (day) . | Complication . |
|---|---|---|---|---|---|---|---|
| Gagner M | 1998 | 5 | 12-2-2-2 | 90 | N/A | 1 | None |
| Yuan RH | 1998 | 2 | 12-2-2-2 | N/A | N/A | N/A | N/A |
| Backus CL | 2000 | 16 | 12-2-2 | 114 | 44 | 1.4 | None |
| Mamazza L | 2001 | 10 | 12-3-3-3 | 175 | N/A | 2.2 | Urinary retension: 1 |
| Postoperative bleeding: 1 | |||||||
| Tagaya N | 2002 | 3 | 12-2-2-2 | 167 | 70 | 5 | None |
| Our case | 2021 | 3 | 12-3-3 | 176 | 70 | 4.7 | None |
N/A: not available
| Author . | Year . | Case . | Port . | Operation time (min) . | Blood loss (ml) . | POHS (day) . | Complication . |
|---|---|---|---|---|---|---|---|
| Gagner M | 1998 | 5 | 12-2-2-2 | 90 | N/A | 1 | None |
| Yuan RH | 1998 | 2 | 12-2-2-2 | N/A | N/A | N/A | N/A |
| Backus CL | 2000 | 16 | 12-2-2 | 114 | 44 | 1.4 | None |
| Mamazza L | 2001 | 10 | 12-3-3-3 | 175 | N/A | 2.2 | Urinary retension: 1 |
| Postoperative bleeding: 1 | |||||||
| Tagaya N | 2002 | 3 | 12-2-2-2 | 167 | 70 | 5 | None |
| Our case | 2021 | 3 | 12-3-3 | 176 | 70 | 4.7 | None |
| Author . | Year . | Case . | Port . | Operation time (min) . | Blood loss (ml) . | POHS (day) . | Complication . |
|---|---|---|---|---|---|---|---|
| Gagner M | 1998 | 5 | 12-2-2-2 | 90 | N/A | 1 | None |
| Yuan RH | 1998 | 2 | 12-2-2-2 | N/A | N/A | N/A | N/A |
| Backus CL | 2000 | 16 | 12-2-2 | 114 | 44 | 1.4 | None |
| Mamazza L | 2001 | 10 | 12-3-3-3 | 175 | N/A | 2.2 | Urinary retension: 1 |
| Postoperative bleeding: 1 | |||||||
| Tagaya N | 2002 | 3 | 12-2-2-2 | 167 | 70 | 5 | None |
| Our case | 2021 | 3 | 12-3-3 | 176 | 70 | 4.7 | None |
N/A: not available
CONFLICT OF INTEREST STATEMENT
None decleared.
FUNDING
None.



