-
PDF
- Split View
-
Views
-
Cite
Cite
Raid Alghamdi, Amer Alzahrnai, Abdulaziz Alosaimi, Ibrahim Albabtain, Infarcted wandering spleen: A case report from Saudi Arabia, Journal of Surgical Case Reports, Volume 2021, Issue 6, June 2021, rjab277, https://doi.org/10.1093/jscr/rjab277
Close - Share Icon Share
Abstract
Spleen is normally positioned in the left upper quadrant. Abnormal location where it is not found in its normal anatomical position is called wandering spleen (WS). Wandering spleen is a rare medical condition that occurs due to developmental abnormality or acquired laxity of the ligaments that hold the spleen in its normal anatomical position. It affects children and young adults, especially childbearing age women. Patients affected with this condition may present with nonspecific symptoms requiring a high index of suspicion. Here, we are presenting a 20-year-old female known to have WS ended up with infarcted WS requiring emergency splenectomy.
INTRODUCTION
Spleen is normally positioned in the left upper quadrant. Abnormal location where it is not found in its normal location is called Wandering spleen (WS). WS is a rare medical condition that occurs due to developmental abnormality or acquired laxity of the ligaments that hold the spleen in its normal anatomical position. It affects children and young adults, especially childbearing age women. Patients affected with this condition may present with nonspecific symptoms requiring a high index of suspicion. Here, we are presenting a 20-year-old female known to have WS ended up with infarcted WS.
CASE PRESENTATION
A 20-year-old female, not married, presented to the emergency department with severe left lower quadrant abdominal pain for one day. The pain is continuous described as dull in nature none radiating with history of previous similar milder attacks. The patient denies any lower urinary tract symptoms, nausea, vomiting, chills, rigors, diarrhea and trauma. She reports regular periods and her last menstrual period was three weeks ago.
The patient is known to have William syndrome with a past surgical history of atrial septal defect repair when she was 8 years of age. She is following with cardiac surgery as she was recently diagnosed to have mitral valve prolapse with severe mitral regurgitation planned for surgery.
On examination, she looked well but in pain. Heart rate 107 beats per minute and a blood pressure of 141/69 mmHg. Her temperature was 36.8°C and saturating well on RA 100%. Her abdominal examination positive only for moderate left lower quadrant tenderness and palpable tender mass in the left lower quadrant, soft abdomen with no signs of peritoneal irritation nor abdominal distention.
Her laboratory investigations were unremarkable aside from mild leukocytosis with a white cell count of 16 d/L. Computed tomography (CT) abdomen with intravenous contrast revealed twisted wandering dysmorphic spleen in the left mid abdomen with subsequent infarction (Fig. 1).
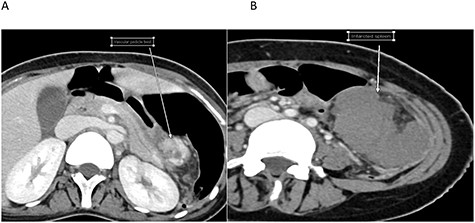
Cross-sectional images of the same patient at the time of infarction. A. Twisted pedicle. B. Infarcted WS.
Upon reviewing her file, she had a CT scan done two years prior to this presentation for an abdominal pain and it confirmed the diagnosis of WS; however, no treatment options were offered to her with no follow-ups (Fig. 2).

Cross-sectional image at the time initial diagnosis shows normal enhancement.
Patient was then pushed to the operating theater for diagnostic laparotomy and possible splenectomy. Abdomen was explored an 8-cm midline incision revealing a wondering spleen in the mid abdomen connected only with colonosplenic ligament with twisted splenic pedicle. Splenectomy performed and patient was shifted to postanesthesia care unit in stable condition (Fig. 3). Hospital course was unremarkable and patient was kept in the hospital for three days for observation then discharged home.
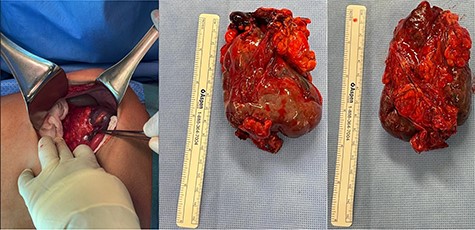
Intraoperative clinical photographs showing infarcted malformed WS.
DISCUSSION
WS is a rare condition that is characterized by laxity or sometimes absence of the ligaments that hold the spleen in its normal anatomical position [1]. The incidence of WS is estimated to be 0.2% [2]. It has a female predominance and the most common age of presentation is childhood, and in adults, if affects female of childbearing age [1, 3]. It has been hypothesized that laxity of the ligaments that hold the spleen is due to effects of estrogen [4]. Moreover, maldevelopment or absence of the suspensory ligaments is another proposed caused of this rare condition [5].
Statistically, it is 2.5 times more common in males under the age of 1 year. However, it is seven times more common in females after age 10. The most common age of clinical presentation is variable. It can be asymptomatic and discovered only on imaging or during clinical examination as a palpable mass and may never be symptomatic [6]. While another set of patients might present with recurrent attacks of abdominal pain due to torsion and spontaneous detorsion of the splenic pedicle. Acute surgical abdomen is more serious presentation secondary to splenic torsion and subsequently acute splenic infarction, a life-threatening condition [7].
Our patient has a previous presentations for a milder abdominal pain attacks; this is could be related to her malformed spleen being subjected to torsion and detorsion. Her first attack was two years prior to this presentation for which she had a CT scan confirming the presence of WS. One case report of a young married woman was published in the year 2020 with a history of recurrent abdominal pain with an US showed no spleen in the LUQ, that was suggestive of WS; however, family ignored to complete full investigations. This case presented five months later with an acute abdomen ended up with emergency laparotomy and splenectomy due to infarcted WS. This highlights the importance of family and patient education as well as planned follow-ups [2].
Diagnostic modalities include CT, magnetic resonance imaging or doppler ultrasound can help to confirm the diagnosis; however, CT scan remains the investigation of choice not only to confirm the diagnosis of WS but more importantly to rule out other causes of acute abdomen as this condition can mimic other pathologies especially in women of childbearing age where it can present as ovarian torsion or rupture ectopic pregnancy [8].
Findings on CT scan include absence of spleen in its normal position, lower pelvic mass representing the malpositioned spleen, homogenous or heterogeneous splenic parenchyma with loss of attenuation [9].
The case presented came with acute abdominal pain and CT scan out of its normal anatomical position was already evident on her previous scans and twisted pedicle with infarcted spleen warranting exploratory laparotomy and eventually splenectomy. WS can be complicated with hypersplenism, splenic infarction, portal hypertension and/or mesenteric varices. Portal hypertension and mesenteric varices is a rare complication and was already reported in the literature, which was hypothesized to be due to mechanical effect of the malpositioned spleen on the extrahepatic portal vasculature [10].
Up to date, the only recommended treatment is operative even in asymptomatic patient due to high rate of complications without removing the spleen. Surgical options can be formal splenectomy laparoscopic or open in case of infarcted spleen or splenopexy as a viable option and as a splenic preservation modality for young patients and those with high risk for overwhelming postsplenectomy sepsis [11].
CONCLUSION
WS remains a rare cause of acute abdominal pain. I acknowledge changes, diagnosis is difficult sometimes; however, when torsion and infarction happens patient will present with acute surgical abdomen requiring emergency splenectomy or splenopexy in a salvageable spleen. We recommend regular follow-ups for patient whom the diagnosis of WS is established and possible splenopexy as viable option to prevent future complications. Future studies are needed for this rare disease in order to improve identifying, monitoring and following up those patient before complication occurs.



