-
PDF
- Split View
-
Views
-
Cite
Cite
Masashi Nagata, Shinichi Otani, Yoshihiko Kanai, Shinichi Yamamoto, Hiroyoshi Tsubochi, Shunsuke Endo, Laser-Trélat sign improved after the resection of a tiny ground-grass nodule: a case report, Journal of Surgical Case Reports, Volume 2021, Issue 6, June 2021, rjab275, https://doi.org/10.1093/jscr/rjab275
Close - Share Icon Share
Abstract
The Laser-Trélat sign refers to eruptive seborrheic keratoses accompanied by internal malignancies, mainly abdominal advanced ones. Detailed associations remain unclear, and the skin lesions do not improve with the treatment of internal malignancies in half of the patients. Herein, we report a rare case of Laser-Trélat sign that improved after resection of a 0.6-cm pulmonary ground-glass nodule: adenocarcinoma in situ. The patient requested the resection with the hopes of improving the skin lesions, though immediate resection was not indicated oncologically. With informed consent, despite possible failure in improving cutaneous diseases, thoracoscopic partial resection of the right lower lobe was performed. Fortunately, her seborrheic keratoses substantially improved after the resection, without exacerbation. To our knowledge, this is the first report describing such a clinical course. It is essential to inform patients regarding the indication of treatment for internal malignancy and its limitation in improving eruptive seborrheic keratoses.
INTRODUCTION
The Laser-Trélat sign (LTS) refers to the rapid progression of seborrheic keratoses (SK) accompanied by internal malignancies [1]. As such, the presence of eruptive SK warrants further investigation for internal malignancies. Gastrointestinal adenocarcinomas in the advanced stage are most commonly associated with LTS [2]. In half of the patients with suspected LTS, skin lesions do not change even after treatment of the malignancies [1, 3]. Herein, we report an unusual case of progressive SK, which improved after resection of a tiny lung ground-glass nodule (GGN), which was an adenocarcinoma in situ.
CASE REPORT
A never-smoker woman in her 50s with unremarkable family and medical history was referred to our department by a dermatologist to treat a lung nodule following a history of rapidly growing brown-to-black spots with mild pruritus, mainly on her trunk (Fig. 1). Histopathologic analysis was consistent with SK. To rule out the possibility of LTS, the patient was evaluated for potential internal malignancies. Computed tomography (CT) revealed a 0.6-cm pure GGN in the right lower lobe (RLL) (Fig. 2). There were no other malignant findings on CT, esophagogastroduodenoscopy, colonoscopy or ultrasonography for breasts and thyroid. All tumor markers examined were within the normal limits.

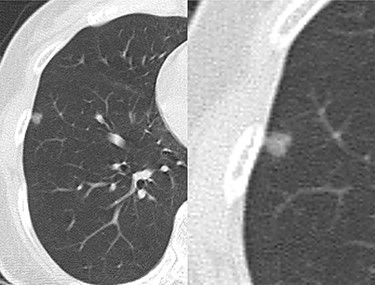
Computed tomography (CT) shows a ground-glass nodule in the right lower lobe.
We considered that the tiny GGN had low malignant potential and thus did not necessitate immediate surgical resection. However, with the hopes of improving her skin lesions, she opted for resection of the GGN. Preoperative examination detected no remarkable risks of lung resection under general anesthesia. Nevertheless, we informed her and her family about the postoperative complications and the possibility that SK would not improve even after the surgery. The patient and her family consented to the operation.
Thoracoscopic partial resection of the RLL with sufficient margins was performed. No perioperative or postoperative complications occurred. She was discharged 5 days later, and the postoperative course after discharge was uneventful. The pathologic features were identical to those of typical adenocarcinoma in situ, Noguchi type B (Fig. 3). After the resection, her SK started improving and kept substantially ameliorated in the 2nd and 4th postoperative year (Fig. 4). She was satisfied with the change in her SK. Currently, she has no re-exacerbation of SK and new malignancy.
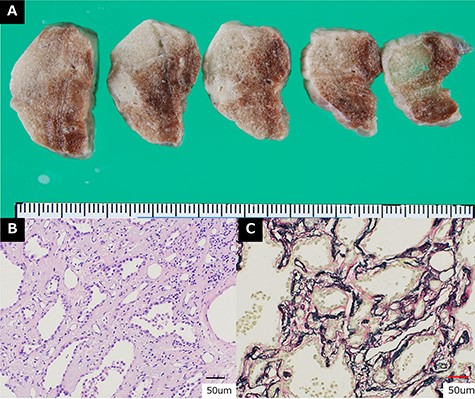
Pathological findings. (A) Macroscopic specimen of the resected tumors. (B) Hematoxylin and eosin staining (×200). (C) Elastica van Gieson staining (×200). These findings were compatible with typical adenocarcinoma in situ, Noguchi type B.
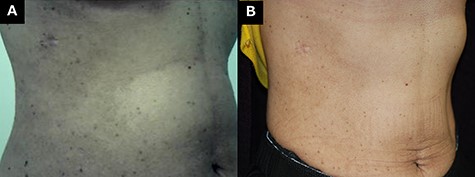
Seborrheic keratoses after resection of the lung nodule. (A) Two years after the operation. (B) Four years after the operation.
Informed consent was obtained from the patient for publication of this report and any accompanying images. A copy of the written consent was also obtained. The case report complied with the principles of the Declaration of Helsinki (as revised in 2013) and was approved by our institutional review board (approval number 2020-014).
DISCUSSION
Since the first report of LTS in the 1900s [4], many cases of eruptive SK and internal malignancies have been documented. However, eruptive SK without any malignancies [3, 5] or with non-malignant events such as human immunodeficiency virus infection, erythrodermic pityriasis rubra pilaris and adalimumab use [6–8] has been reported. Although the mechanisms between progressive SK and internal malignancies remain unclear, tumor cells that produce transforming growth factor-α have been implicated to facilitate growth of the skin lesions [9]. As described above, the improvement of the cutaneous lesions after the treatment of malignancies was seen in only half of the cases, and the reason for this is still unknown. As such, predicting the effect of treating the underlying malignancy on SK remains to be a challenge.
Both SK and malignancy are often seen in elderly patients. This makes it difficult to establish a direct causality of SK and malignancy as observed in LTS. This is why it is doubtful that eruptive SK is a paraneoplastic dermatosis [4, 10]. Nevertheless, the rapid development of SK is regarded as a cutaneous marker that alerts the existence of an underlying internal malignancy.
To the best of our knowledge, this is the first case report of progressive SK improvement after resection of a tiny GGN consistent with the histology of lung adenocarcinoma in situ. Lung cancers account for approximately 6% of internal malignancies associated with LTS. These were less frequently found than gastrointestinal cancers, as were early cancers than advanced cancers [11]. In a literature search using PubMed, we did not find any similar report. Interestingly, the eruptive SK improved after resection of the GGN. Spontaneous remission of eruptive SK has not been reported in PubMed regardless of internal malignancies. This suggests a possible association between cutaneous disease and progression or treatment of internal malignancies. Rapidly developing SK could result from complex interactions among multiple associated factors, including internal malignancy. The GGN likely had the genetic mutation of epidermal growth factor receptor. Even if the skin lesion has the abnormality regarding epidermal growth factor, we cannot explain the causality at this time. The exact roles that these factors play require further evaluation.
In this report, the GGN was resected with the hope of improving symptomatic SK. Since there was no indication for immediate surgical resection oncologically, it is controversial to perform GGN resection to improve SK. Nevertheless, surgery was still performed with the informed consent and strong request from the patient. Fortunately, no intraoperative or postoperative complications occurred, and the eruptive SK improved.
Despite these results, it is important to consider that postoperative complications cannot be completely avoided, even in patients with no perioperative risks. Additionally, it is uncertain whether lung resection cures eruptive SK. Thus, it is crucial to comprehensively inform patients and their families regarding the risk of postoperative complications, possibility of SK treatment failure after resection and treatment alternatives (e.g. repeated resections and cryotherapies) for symptomatic SK.
In conclusion, we encountered an extremely rare case of LTS that improved after resection of a tiny lung GGN consistent with the histology of adenocarcinoma in situ. This report highlights the role of treating the underlying malignancy in improving outcomes of symptomatic SK. It is essential to inform patients with LTS and their families regarding the indication of treatment for internal malignancy and its limitation in improving eruptive SK.
ACKNOWLEDGMENTS
We thank Dr. Masako Arai, a dermatologist at Okinawa Kyodo Hospital, for informing us of the patient and the Laser-Trélat sign. We also thank Dr. Kayoko Higuchi and Ryoji Uchima, pathologists at Okinawa Kyodo Hospital, for their diagnostic pathology.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



