-
PDF
- Split View
-
Views
-
Cite
Cite
Yuta Ushida, Hiromichi Ito, Yosuke Inoue, Takafumi Sato, Yoshihiro Ono, Atsushi Oba, Yu Takahashi, Liposarcoma of gallbladder: a case report and literature review, Journal of Surgical Case Reports, Volume 2021, Issue 6, June 2021, rjab273, https://doi.org/10.1093/jscr/rjab273
Close - Share Icon Share
Abstract
A 53-year-old man with prior history of resection of liposarcoma in his leg presented with gallbladder mass. Computed tomography showed 4-cm tumor at gallbladder fundus with weak enhancement with IV contrast. Differential diagnoses included hemangioma and liposarcoma, and laparoscopic cholecystectomy was recommended. In the operating room, the tumor appeared without serosal and liver invasions and uncomplicated laparoscopic cholecystectomy was completed. Histopathological examination revealed the tumor as myxoid liposarcoma with round cells. Adjuvant chemotherapy was not given, and he was placed on imaging surveillance. At 16 months after the operation, he developed recurrence of liposarcoma in the left popliteal fossa.
INTRODUCTION
Gallbladder sarcoma is rare and the most have been the subject for case report. There were 46 cases with primary gallbladder sarcoma reported in past two decades. Among them, liposarcoma of gallbladder is extremely rare and there were only five well documented in English literatures to our knowledge [1–4]. Here, we report a case of gallbladder liposarcoma which we recently experienced, with literature review for this rare disease.
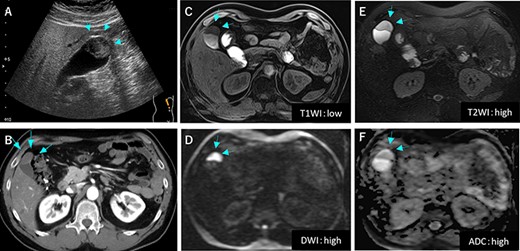
Preoperative image findings; (A) Gallbladder tumor was at gallbladder body by abdominal ultrasonography; (B) CT scan revealed slightly enhanced tumor located at gallbladder fundus; (C–F) On MRI, the tumor had high signal in both of T2 and diffusion weighed image and low signal in both of T1 and apparent diffusion coefficient.
CASE REPORT
A 53-year-old man with history of liposarcoma had gallbladder tumor detected during routine ultrasonography (Fig. 1A) and was referred to us. He was first diagnosed as leg liposarcoma 5 years before and underwent complete resection. Despite of history of liposarcoma in his leg, he never developed any abdominal symptoms. Laboratory tests were unremarkable including carcinoembryonic antigen and carbohydrate antigen 19-9 (CA19-9) within their normal limits. Computed tomography (CT) scan demonstrated slightly enhanced 4-cm tumor located at gallbladder fundus (Fig. 1B). On magnetic resonance imaging (MRI), the tumor had high signal in both of T2 and diffusion weighed image and low signal in both of T1 and apparent diffusion coefficient (Fig. 1C–F). Based on these findings in imaging studies, our working differential diagnosis included liposarcoma and hemangioma rather than adenocarcinoma, and we recommended laparoscopic cholecystectomy. In the exploration, the tumor in the fundus appeared without serosal invasion (Fig. 2). Intraoperative ultrasonography revealed the tumor was contained in the gallbladder without infiltration into the liver, and in fact there was a distance between the liver bed and the tumor. Sonazoid enhanced ultrasonography ruled out liver metastasis and thus, we proceeded to laparoscopic cholecystectomy as planned. When the gallbladder was opened, yellowish white tumor was confirmed in the submucosal layer with the overlying mucosa intact (Fig. 3A). Histopathological examination revealed, this tumor as myxoid liposarcoma consisting of lipoblasts and round cells. There was no necrosis and proliferations of spindle and round cell component were identified in the background of myxoid stroma (Fig. 3B). These histological features were similar to the ones for the sarcoma in his leg that was resected before. The patient’s postoperative course was uncomplicated and was discharged home on Day 3. The adjuvant therapy was elected not to be given and he was placed on imaging surveillance with CT scan in every 3–6 months. In 16 months after this operation, he developed disease recurrence in the left popliteal fossa. There was no recurrence to date in the abdominal cavity at 28 months after the operation, he was alive with disease.
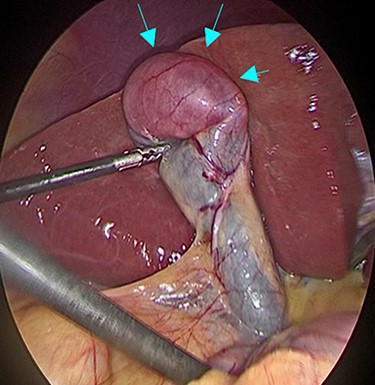
Intraoperative findings during laparoscopic cholecystectomy; The tumor was at fundus of gallbladder without serosal invasion.
DISCUSSION
Sarcoma of gallbladder is a rare clinical entity, and a PubMed search using key words of gallbladder and sarcoma identified 46 reported cases in past two decades [2, 4–7] (Table 1). The histopathological types of sarcoma were as shown in Table 1, and leiomyosarcoma and malignant fibrous histiocytoma variants were the most common subtype (35% for each) and liposarcoma represented for 11% of gallbladder sarcoma. Most patients underwent simple cholecystectomy and only one patient with angiosarcoma (2%) was reported to have lymph node metastasis.
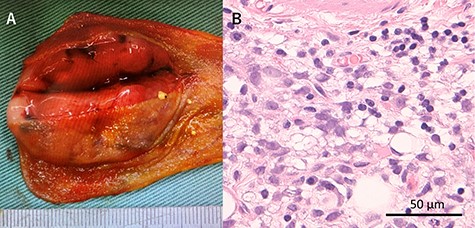
Macroscopic and microscopic findings of the resected specimen; (A) Tumor was solid and well-defined tumor mainly in the submucosa; (B) Tumor was myxoid liposarcoma consisting of solid growth of lipoblasts and round cells; There was no necrosis and proliferation of spindle and round cell component were identified in the background of myxoid stroma.
| Characteristics . | N = 46 (%) . |
|---|---|
| Age, years [range] | 66 [2–88] |
| Sex | |
| Female / Male | 33 (72) / 12 (28) |
| Classification of sarcoma type | |
| Leiomyosarcoma | 16 (35) |
| Malignant fibrous histiocytoma variants | 16 (35) |
| Angiosarcoma | 6 (13) |
| Liposarcoma | 5 (11) |
| Rhabdomyosarcoma | 3 (7) |
| Tumor size (cm) [range] | 4.8 [1–25] |
| Type of surgery | |
| Cholecystectomy [Laparoscopy] | 34 (74) [0 (0)] |
| Extended cholecystectomy | 11 (24) |
| Bile duct resection | 1 (2) |
| Unknown | 1 (2) |
| Lymphadenectomy | |
| Yes / No / Unknown | 4 (9) / 41 (89) / 1 (2) |
| Lymph node metastasis | |
| Yes / No / Unknown | 1 (2) / 7 (15) / 38 (83) |
| Margin status | |
| R0 / R1 / R2 / Unknown | 10 (22) / 0 (0) / 1 (2) / 35 (76) |
| Follow-up period (months) [range] | 12 [0.7–324] |
| Recurrence | 8 (17) |
| Liver | 5 (11) |
| Peritoneal metastasis | 3 (7) |
| Others (pancreas, colon) | 2 (4) |
| Characteristics . | N = 46 (%) . |
|---|---|
| Age, years [range] | 66 [2–88] |
| Sex | |
| Female / Male | 33 (72) / 12 (28) |
| Classification of sarcoma type | |
| Leiomyosarcoma | 16 (35) |
| Malignant fibrous histiocytoma variants | 16 (35) |
| Angiosarcoma | 6 (13) |
| Liposarcoma | 5 (11) |
| Rhabdomyosarcoma | 3 (7) |
| Tumor size (cm) [range] | 4.8 [1–25] |
| Type of surgery | |
| Cholecystectomy [Laparoscopy] | 34 (74) [0 (0)] |
| Extended cholecystectomy | 11 (24) |
| Bile duct resection | 1 (2) |
| Unknown | 1 (2) |
| Lymphadenectomy | |
| Yes / No / Unknown | 4 (9) / 41 (89) / 1 (2) |
| Lymph node metastasis | |
| Yes / No / Unknown | 1 (2) / 7 (15) / 38 (83) |
| Margin status | |
| R0 / R1 / R2 / Unknown | 10 (22) / 0 (0) / 1 (2) / 35 (76) |
| Follow-up period (months) [range] | 12 [0.7–324] |
| Recurrence | 8 (17) |
| Liver | 5 (11) |
| Peritoneal metastasis | 3 (7) |
| Others (pancreas, colon) | 2 (4) |
| Characteristics . | N = 46 (%) . |
|---|---|
| Age, years [range] | 66 [2–88] |
| Sex | |
| Female / Male | 33 (72) / 12 (28) |
| Classification of sarcoma type | |
| Leiomyosarcoma | 16 (35) |
| Malignant fibrous histiocytoma variants | 16 (35) |
| Angiosarcoma | 6 (13) |
| Liposarcoma | 5 (11) |
| Rhabdomyosarcoma | 3 (7) |
| Tumor size (cm) [range] | 4.8 [1–25] |
| Type of surgery | |
| Cholecystectomy [Laparoscopy] | 34 (74) [0 (0)] |
| Extended cholecystectomy | 11 (24) |
| Bile duct resection | 1 (2) |
| Unknown | 1 (2) |
| Lymphadenectomy | |
| Yes / No / Unknown | 4 (9) / 41 (89) / 1 (2) |
| Lymph node metastasis | |
| Yes / No / Unknown | 1 (2) / 7 (15) / 38 (83) |
| Margin status | |
| R0 / R1 / R2 / Unknown | 10 (22) / 0 (0) / 1 (2) / 35 (76) |
| Follow-up period (months) [range] | 12 [0.7–324] |
| Recurrence | 8 (17) |
| Liver | 5 (11) |
| Peritoneal metastasis | 3 (7) |
| Others (pancreas, colon) | 2 (4) |
| Characteristics . | N = 46 (%) . |
|---|---|
| Age, years [range] | 66 [2–88] |
| Sex | |
| Female / Male | 33 (72) / 12 (28) |
| Classification of sarcoma type | |
| Leiomyosarcoma | 16 (35) |
| Malignant fibrous histiocytoma variants | 16 (35) |
| Angiosarcoma | 6 (13) |
| Liposarcoma | 5 (11) |
| Rhabdomyosarcoma | 3 (7) |
| Tumor size (cm) [range] | 4.8 [1–25] |
| Type of surgery | |
| Cholecystectomy [Laparoscopy] | 34 (74) [0 (0)] |
| Extended cholecystectomy | 11 (24) |
| Bile duct resection | 1 (2) |
| Unknown | 1 (2) |
| Lymphadenectomy | |
| Yes / No / Unknown | 4 (9) / 41 (89) / 1 (2) |
| Lymph node metastasis | |
| Yes / No / Unknown | 1 (2) / 7 (15) / 38 (83) |
| Margin status | |
| R0 / R1 / R2 / Unknown | 10 (22) / 0 (0) / 1 (2) / 35 (76) |
| Follow-up period (months) [range] | 12 [0.7–324] |
| Recurrence | 8 (17) |
| Liver | 5 (11) |
| Peritoneal metastasis | 3 (7) |
| Others (pancreas, colon) | 2 (4) |
Liposarcoma commonly occurs at the proximal extremities and the retroperitoneum [8]. Liposarcoma with visceral organ origin including gastrointestinal tract, gallbladder, is extremely rare with only five relevant cases reported so far [1–4]. Liposarcoma is divided into four histological subtypes: well-differentiated liposarcoma (WDL), pleomorphic liposarcoma (PL), dedifferentiated liposarcoma (DL) and myxoid liposarcoma (ML). Among these, ML is characterized as slow-growing and low-grade tumor with low metastatic potential, like well-differentiated liposarcoma [8] (Table 2).
| Authors . | Reported year . | Age (years) /Sex . | Preoperative diagnosis . | Other lesions . | Tumor size (cm) . | Type of surgery . | Subtypes . | Lympha-denectomy . | Lymph node metastasis . | Recurrence . | Prognosis (POM) . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Hamada T | 2006 | 49 / F | Angiosarcoma | No | 25 × 23 | Cholecystectomy | PL | No | No | Liver | Alive (39) |
| Husain EA | 2009 | 64 / F | N/A | No | 1.7 | Cholecystectomy | ML | No | No | N/A | DOD (N/A) |
| Husain EA | 2009 | 70 / F | N/A | No | 3 | Cholecystectomy | ML | No | No | N/A | DOU (N/A) |
| Ma Y | 2014 | 70 / F | N/A | No | 13 × 8 | Cholecystectomy | ML | No | No | No recurrence | Alive (N/A) |
| Da Costa AC | 2018 | 71 / F | Gallbladder cancer | No | 14 × 14 | Extended cholecystectomy | DL | No | No | No recurrence | Alive (8) |
| Our case | 2020 | 53 / M | Liposarcoma | Left leg | 4 × 3.5 | Laparoscopic Cholecystectomy | ML | No | No | left popliteal fossa | Alive (28) |
| Authors . | Reported year . | Age (years) /Sex . | Preoperative diagnosis . | Other lesions . | Tumor size (cm) . | Type of surgery . | Subtypes . | Lympha-denectomy . | Lymph node metastasis . | Recurrence . | Prognosis (POM) . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Hamada T | 2006 | 49 / F | Angiosarcoma | No | 25 × 23 | Cholecystectomy | PL | No | No | Liver | Alive (39) |
| Husain EA | 2009 | 64 / F | N/A | No | 1.7 | Cholecystectomy | ML | No | No | N/A | DOD (N/A) |
| Husain EA | 2009 | 70 / F | N/A | No | 3 | Cholecystectomy | ML | No | No | N/A | DOU (N/A) |
| Ma Y | 2014 | 70 / F | N/A | No | 13 × 8 | Cholecystectomy | ML | No | No | No recurrence | Alive (N/A) |
| Da Costa AC | 2018 | 71 / F | Gallbladder cancer | No | 14 × 14 | Extended cholecystectomy | DL | No | No | No recurrence | Alive (8) |
| Our case | 2020 | 53 / M | Liposarcoma | Left leg | 4 × 3.5 | Laparoscopic Cholecystectomy | ML | No | No | left popliteal fossa | Alive (28) |
F, female; M, male; PL, pleomorphic liposarcoma; ML, myxoid liposarcoma; DL, dedifferentiated liposarcoma; DOD, died of disease; DOU, died of unrelated cause; POM, postoperative months.
| Authors . | Reported year . | Age (years) /Sex . | Preoperative diagnosis . | Other lesions . | Tumor size (cm) . | Type of surgery . | Subtypes . | Lympha-denectomy . | Lymph node metastasis . | Recurrence . | Prognosis (POM) . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Hamada T | 2006 | 49 / F | Angiosarcoma | No | 25 × 23 | Cholecystectomy | PL | No | No | Liver | Alive (39) |
| Husain EA | 2009 | 64 / F | N/A | No | 1.7 | Cholecystectomy | ML | No | No | N/A | DOD (N/A) |
| Husain EA | 2009 | 70 / F | N/A | No | 3 | Cholecystectomy | ML | No | No | N/A | DOU (N/A) |
| Ma Y | 2014 | 70 / F | N/A | No | 13 × 8 | Cholecystectomy | ML | No | No | No recurrence | Alive (N/A) |
| Da Costa AC | 2018 | 71 / F | Gallbladder cancer | No | 14 × 14 | Extended cholecystectomy | DL | No | No | No recurrence | Alive (8) |
| Our case | 2020 | 53 / M | Liposarcoma | Left leg | 4 × 3.5 | Laparoscopic Cholecystectomy | ML | No | No | left popliteal fossa | Alive (28) |
| Authors . | Reported year . | Age (years) /Sex . | Preoperative diagnosis . | Other lesions . | Tumor size (cm) . | Type of surgery . | Subtypes . | Lympha-denectomy . | Lymph node metastasis . | Recurrence . | Prognosis (POM) . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Hamada T | 2006 | 49 / F | Angiosarcoma | No | 25 × 23 | Cholecystectomy | PL | No | No | Liver | Alive (39) |
| Husain EA | 2009 | 64 / F | N/A | No | 1.7 | Cholecystectomy | ML | No | No | N/A | DOD (N/A) |
| Husain EA | 2009 | 70 / F | N/A | No | 3 | Cholecystectomy | ML | No | No | N/A | DOU (N/A) |
| Ma Y | 2014 | 70 / F | N/A | No | 13 × 8 | Cholecystectomy | ML | No | No | No recurrence | Alive (N/A) |
| Da Costa AC | 2018 | 71 / F | Gallbladder cancer | No | 14 × 14 | Extended cholecystectomy | DL | No | No | No recurrence | Alive (8) |
| Our case | 2020 | 53 / M | Liposarcoma | Left leg | 4 × 3.5 | Laparoscopic Cholecystectomy | ML | No | No | left popliteal fossa | Alive (28) |
F, female; M, male; PL, pleomorphic liposarcoma; ML, myxoid liposarcoma; DL, dedifferentiated liposarcoma; DOD, died of disease; DOU, died of unrelated cause; POM, postoperative months.
Resection with negative margins is the standard treatment for soft-tissue sarcoma and the same principle should be applied to gallbladder liposarcoma. Unlike adenocarcinoma of gallbladder, the role of extended resection with adjacent liver and portal lymphadenectomy for gallbladder sarcoma remains unclear. Given the low risk for lymphatic spread for sarcoma in general, we did not perform portal lymphadenectomy for our patient with small gallbladder mass without sign of invasion to the liver bed.
In terms of long-term outcomes, the patients with low-grade myxoid and well-differentiated subtypes have excellent outcomes with survival rate greater than 90% at 5 years after complete resection [4, 9, 10]. Chemotherapy should be reserved for unresectable disease and adjuvant therapy after complete resection is not recommended. As our patients developed recurrence in multiple sites including left popliteal fossa at 16 months after the operation and left groin and right popliteal fossa at 19 months, he received systemic chemotherapy rather than repeat resections. Although ML is known to be more sensitive to traditional cytotoxic agents including doxorubicin or ifosfamide than other types of sarcomas [11], trabectedin was elected as his chemotherapeutic regimen based on the genomic test for his recurrent tumor. Trabectedin targets FUS-CHOP oncoprotein and shown to be effective for patients with liposarcoma with FUS-CHOP fusion gene [12].
We thought his GB sarcoma as a second primary disease based on his clinical course and treated it accordingly. However, it is not easy to prove whether this lesion was truly a second primary of multifocal disease or not, and it could be an unusual form of metastasis. In fact, multifocal sarcoma is a rare and controversial entity. ‘Multifocal’ disease judged by clinical criteria reported as rare as 1% among all types of sarcoma [13] or 4.5% among liposarcoma [14]. In two studies using genomic analysis, the tumors at different site in all patients with ‘multifocal’ myxoid liposarcoma had the monoclonality in the genomic profile and they concluded clinical ‘multifocal’ disease is likely an atypical pattern of metastatic disease [14, 15]. For our patient, unfortunately, genomic test was not available for previously resected tumor.
In conclusions, we have presented a rare case of gallbladder liposarcoma. Collaborative efforts to collect and compile pieces of information for clinicopathological features and treatment outcomes for each case is essential to establish the optimized care for this extremely rare disease.
CONFLICT OF INTEREST STATEMENT
The authors have no conflicts of interest to declare and received no financial support for this report.
HUMAN AND ANIMAL RIGHTS
All procedures followed have been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.



