-
PDF
- Split View
-
Views
-
Cite
Cite
Fleur C Muirhead, Hong L Lee, Rajeev Singh, Ovarian endosalpingiosis mimicking hydrosalpinges. Unexpected intraoperative findings and a diagnostic rollercoaster, Journal of Surgical Case Reports, Volume 2021, Issue 6, June 2021, rjab264, https://doi.org/10.1093/jscr/rjab264
Close - Share Icon Share
Abstract
Over 80 % of ovarian cancer diagnoses are in women aged over 50 years. Post-menopausal women are at significantly increased risk compared with other age groups. Tumour biomarkers and ultrasound assist with diagnostics. A post-menopausal woman was referred with a possible left adnexal cyst on ultrasound. A tertiary gynaecological ultrasound suggested bilateral hydrosalpinges without cysts. Tumour markers were negative. Unexpectedly, while undergoing a laparoscopy, the tubes were normal in appearance; however, multiple cystic deposits suspicious for malignancy were noted on the ovaries. A laparoscopic bilateral salpingo-oophorectomy was performed without spillage and pelvic washings obtained. On histopathology, the ovaries contained multiple, benign epithelial cysts and pelvic washings were negative. This case demonstrates an unanticipated peri-operative diagnostic dilemma. It highlights the surgical management decisions required to balance duty of care and consent compliance within the scope of general gynaecology. It emphasizes the importance of histopathological examination to confirm diagnoses.
INTRODUCTION
Post-menopausal women are at increased risk of malignancy compared with other age groups; however, the majority of adnexal masses are histologically benign [1]. After menopause, the reproductive tract is no longer influenced by the hormonal fluctuations of the menstrual cycle, hence the absence of physiological follicles [2]. Any post-menopausal, ultrasound confirmed adnexal masses should be thoroughly investigated. Certain sonologic ovarian cyst characteristics, such as solid components, complete septations, papillary projections or ascites, can suggest malignancy [3].
Tumour biomarkers and imaging can assist with adnexal pathology diagnostics, particularly ultrasound [3]. Commonly used tumour markers include cancer antigen 125 (Ca125), carcinoembryonic antigen (CEA) and lactate dehydrogenase (LD). An increase in serum Ca125 can be caused by multiple conditions, many of which are benign, and however, a rise in serum Ca125 is noted in 80% of ovarian epithelial cancers [4, 5].

The tertiary ultrasound of the right adnexa demonstrating the 33 mm × 18 mm × 34 mm serpiginous cystic structure with a 13-mm lumen consistent with a hydrosalpinx.
The likelihood that an ovarian mass is cancerous can be determined using the Risk of Malignancy Index I (RMI). The RMI-I is calculated utilizing menopausal status, a serum Ca125 result and ultrasonographic features, and is widely adopted in first world countries [6, 7]. The RMI-I has a sensitivity of 78% and a specificity of 87% for ovarian malignancy when the cutoff is 200 [7].
Evidence suggests that a referral to a multidisciplinary, gyane-oncology team should be completed for staging and further management if an RMI-I score is greater than 200 [6]. For a post-menopausal woman with suspected benign pathology, the gold standard to exclude ovarian malignancy is a laparoscopic bilateral salpingo-oophorectomy (BSO), if appropriate. The BSO should be performed utilizing a retrieval bag to avoid spillage and subsequent histopathological examination [6–8]. Surgeon visualization and judgement during laparoscopy has a sensitivity of 87.5% and a specificity of 98% for discriminating malignant from benign disease [9]. Multiple studies demonstrate that even with a low pre-operative index of suspicion, unexpected ovarian malignancy was noted on 0.9–8% histopathological examinations [4, 10, 11].
CASE REPORT
A post-menopausal woman was referred to the gynaecological outpatient clinic with an incidental finding of a possible left adnexal cyst on a renal tract ultrasound for routine chronic kidney disease surveillance. She was 16 years post-menopausal with no significant risk factors for pelvic inflammatory disease or gynaecological cancers.
The patient was referred for a pelvic ultrasound, which demonstrated a 2.5-cm left ovarian cyst with a thin, avascular septum and a possible right-sided hydrosalpinx. These findings remained stable on a repeat ultrasound 9 months later. Ca125, CEA and LD were negative.
On review in gynaecology clinic, the patient was asymptomatic and following joint discussion regarding the management options, the surgeon recommended a laparoscopic BSO. The patient opted for surveillance management and was subsequently referred for a tertiary ultrasound and repeat tumour markers.
The tertiary level gynaecological ultrasound demonstrated a right adnexal serpiginous structure with a lumen and incomplete septae and a left adnexal cystic structure (Figs 1 and 2). The ultrasonographic features were consistent with those of hydrosalpinges [12]. The Ca125 remained negative. In view of the ultrasound diagnosis of hydrosalpinges and the patient’s post-menopausal status, a laparoscopic BSO was recommended and the patient subsequently consented.
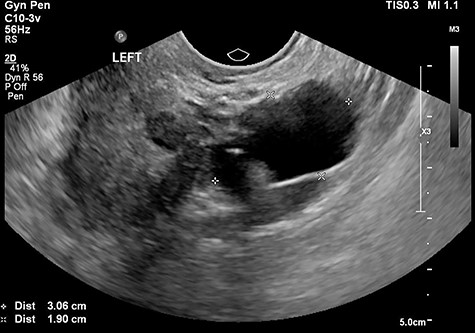
The tertiary ultrasound of the left adnexa demonstrating a 30 mm × 19 mm × 27 mm cystic structure with incomplete septae in keeping with a possible hydrosalpinx.
Intraoperative findings were inconsistent with all pre-operative ultrasound diagnoses. Both ovaries appeared suspicious for malignancy with cystic lesions covering the surface of the right, while the left appeared to contain two smaller cysts (Figs 3–5). There were no hydrosaplinges or free fluid within the pelvis. Given the abnormal features of the ovaries, the surgeon proceeded with the laparoscopic BSO without spillage. Pelvic washings were performed, though there were no atypical peritoneal or omental lesions for biopsy.
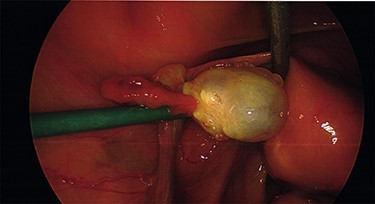
The intra-operative photos demonstrating the cystic appearance of the left ovary.
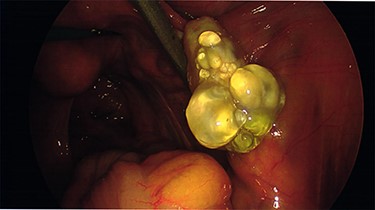
The intra-operative photos demonstrating multiple cystic structures covering the surface of the right ovary.
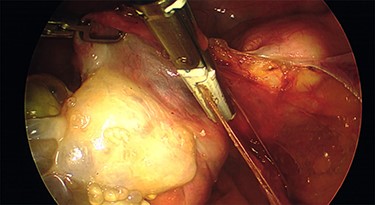
The intra-operative photographs of the posterior aspect of the right ovary.
Despite the sinister appearance macroscopically, histopathology was benign. The ovaries contained multiple, benign, ciliated and epithelial cysts. Pelvic washings were negative for malignancy and the tubes were unremarkable.
The patient had an uneventful post-operative period and was discharged after a follow-up appointment.
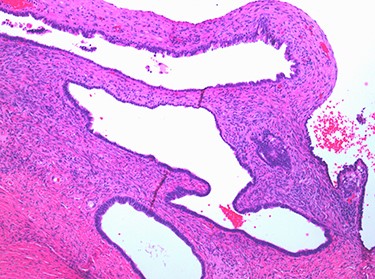
Multiple cysts of variable diameter lined by a single layer of epithelium, separated by ovarian stroma; haematoxylin and eosin stain, medium magnification, scale ×10.
DISCUSSION
This case demonstrates an unexpected, peri-operative diagnostic dilemma. Despite utilizing investigations to aid diagnoses, it remained difficult to distinguish between benign and malignant pathology for this patient [9]. Pre-operatively, the surgical team was confident that patient’s adnexal masses were tubal in origin, not ovarian, as demonstrated on the tertiary ultrasound. In addition, the pre-operative RMI-I score was low risk at 30 and remained so post-operatively.
The surgeon’s ethical challenge on observing the sinister appearance of the ovaries was determining the manner in which to proceed while balancing duty of care and consent compliance. Management of unexpected, suspicious intra-operative findings is operator dependent. There are often valid peri-operative concerns regarding risks, including intra-operative spillage [7] and seeding into post-sites [13]. Adnexectomy without intraperitoneal spillage of the cyst contents utilizing a specimen retrieval bag is the ideal management [6, 11]. Converting a laparoscopy to laparotomy depends on the extent of abnormal pathology and the operating surgeon’s skill and preference [6].
In this case, the laparoscopic BSO was performed as consented without spillage using specimen retrieval bags. Despite the intra-operative diagnosis altering from hydrosalpinges to possible ovarian malignancy, the laparoscopic BSO was still deemed the most appropriate management at the time. Obtaining pelvic washing addressed the surgeon’s suspicion of non-benign pathology. In the event that the histology returned malignant, washings may have aided in staging without compromise consent [14]. In Australia, general gynaecological surgeons do not perform formal staging; therefore, an appendicectomy or further biopsies of the omentum or peritoneum were not performed. This would also have had ethical and legal issues pertaining to consent compliance.
The case emphasizes the diagnostic importance of histopathology, particularly in the setting of unanticipated and sinister macroscopic findings. The macroscopic appearances of the ovaries suggested malignancy diagnosis; however, the histopathology identified benign epithelial cysts [15]. The cyst lining was comprised of a single layer of epithelial cells amid normal ovarian stroma (Figs 6 and 7). The cysts contained normal serous epithelium with cilia lining the cyst lumen. These histological findings are consistent with the Müllerian phenotype and are therefore endosalpingiosis, ectopic tubal cell deposits on the surface of the ovaries, not that of hydrosalpinges or malignant ovarian cysts as the diagnostic rollercoaster suggested [15].
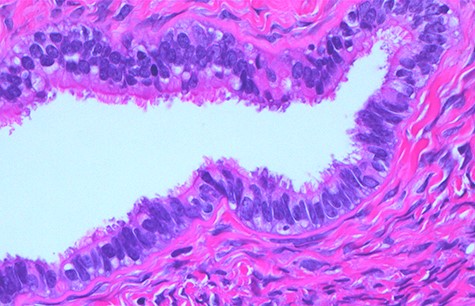
Normal serous epithelium with prominent delicate cilia lining the cyst lumen; haematoxylin and eosin stain, high magnification, scale ×40.
ACKNOWLEDGEMENTS
The authors acknowledge the support of Dr Matthew Bogle of Western Diagnostic Pathology for his expertise in anatomical pathology and histopathological images. The authors also acknowledge the team at the JHC O&G Ultrasound Clinic for the use of their images for this case report.
FUNDING AND CONFLICT OF INTEREST
The authors have sources of funding or no conflicts of interest to declare.



