-
PDF
- Split View
-
Views
-
Cite
Cite
Sabrine Derqaoui, Fouad Zouaidia, Ahmed Jahid, Zakia Bernoussi, Kaoutar Znati, Primary Hodgkin lymphoma of the ulnar nerve: the first case report with review of the literature, Journal of Surgical Case Reports, Volume 2021, Issue 5, May 2021, rjab185, https://doi.org/10.1093/jscr/rjab185
Close - Share Icon Share
Abstract
Hodgkin lymphoma is a lymphoid malignancy characterized by minority population of neoplastic cells (Reed-Sternberg cells and its variants) within a reactive inflammatory background. It encompasses two entities: classical HL (∼95% of cases) and nodular lymphocyte predominant HL (∼5% of cases). Primary lymphoma of peripheral nerves (PLPN) represent a very rare condition, since only 19 cases have been reported in the English literature to date, all of which are of a non-HL phenotype. A 20-year-old female presented an intramural mass of the ulnar nerve. Histological analysis revealed a Classical Hodgkin lymphoma. Further investigations failed to reveal nodal or extranodal involvement. PLPN is a very rare entity. There is a need for further understanding of this unusual lymphoma presentation.
INTRODUCTION
Hodgkin lymphoma is a B-cell lymphoid neoplasm characterized by minority population of neoplastic cells (Reed-Sternberg cells and its variants) within a reactive inflammatory background. It encompasses two entities: classical HL (∼95% of cases) and nodular lymphocyte predominant HL (∼5% of cases) [1]. Neurologic involvement in HL is related to either central nervous system metastasis, paraneoplastic syndrome or treatment toxicity [2]. To date, no HL was found in the 18 cases of primary peripheral nerve’s lymphoma reported previously in the literature. Herein, we describe the first case of classical HL (CHL) arising from a peripheral nerve in 20-year-old female to report on this exceptional entity and to help provide better understanding of this unusual lymphoma presentation.
CASE PRESENTATION
A 20-year-old woman with no medical history presented with a 4-month history of paresthesia in her right ulnar nerve’s sensory territory, and swelling in the cubital fossa 5 weeks before consulting. On examination, she was a healthy woman with stable vital signs; there was a painful tender mass in the cubital fossa (Fig. 1A). Magnetic resonance imaging (MRI) revealed an intraneural well demarcated tumor, measuring 4.8 × 2.7 × 2.5 cm, which was hypointense on T1- and T2-weighted images (Fig. 1B). The interpretation was that of a benign tumor more likely a schwannoma. Thus, a biopsy was performed. On histology, Hematoxylin–eosin stained sections revealed a tumor consisting of sparse large mononuclear cells, with thick nuclear membrane and large nucleoli. Typical multinucleated Reed Sternberg cells and lacunar were also observed. The inflammatory background was dense; composed of plasma cells, neutrophils, eosinophils, histiocytes and small lymphocytes. The latter arranged, in some areas, in primary lymphoid folliculs with germinatif center. On immunohistochemistry, neoplastic cells expressed CD30, CD15 and Pax5 and were negative for CD20 and CD3. The patient underwent surgical excision of the mass. On gross, it was a well demarcated spherical mass measuring 4.2 × 2.5 cm with withe to gray cut surface. The texture was firm at sectioning (Fig. 2A). Morphological and immunohistochemical studies confirmed the diagnosis (Figs 2 and 3). Examination confirmed the diagnosis of classical Hodgkin lymphoma. Physical examination and thoraco abdominal pelvic CT scan failed to show any evidence of generalized lymphoma; bone marrow biopsy was also negative. In the absence of either lymph nodes or extranodal involvement, the diagnosis of primary ulnar nerve HL was retained. The patient was referred to hematology department. Two months later the patient presented with cervical adenopathy, histological examination was consistent of HL. Chemotherapy treatment was initiated.
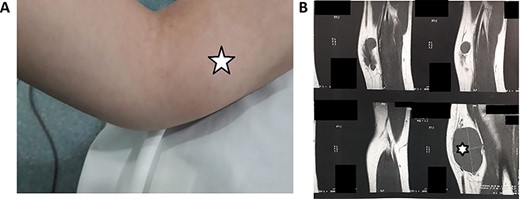
(A) Clinical findings of the mass; (B) MRI showing an intraneural well demarcated tumor, measuring 4.8 × 2.7 × 2.5 cm, which was hypointense on T1-weighted images (white star).
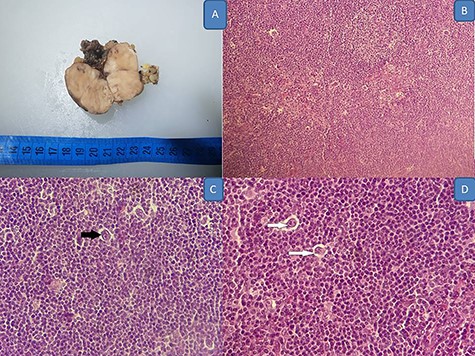
(A) Gross appearance of the mass; (B–D) Hodgkin lymphoma’s histology: neoplastic cells within a reactive inflammatory background: B (HE, x20O), C (HE X 400 black arrow showing RSB cell) and D (HE, X 400 white arrows showing Hodgkin cell).
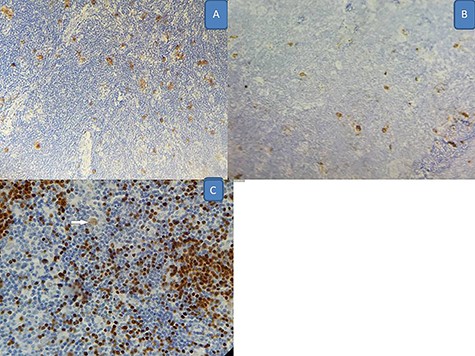
Immunohistochemistry findings (X 200); (A) positivity for CD30; (B) positivity for CD15; (C) positivity for Pax5 (white arrow for neoplastic cells).
DISCUSSION
Primary lymphoma of peripheral nerves (PLPN) represents a very rare condition, since only 19 cases have been reported in the English literature to date. All of these are B or T non-Hodgkin lymphoma, with diffuse large B cell lymphoma being the most common subtype [3], and this is the first case of primary HL arising in a peripheral nerve. Peripheral nervous system involvement in non-HL can present in multiple ways including: (i) lymphoma’s paraneoplastic effect, (ii) compression of a peripheral nerve due to soft-tissue or adjacent nodal masses; (iii) direct invasion of the nerve, (iv) neurolymphomatosis which corresponds to the infiltration of multiple peripheral nerves by lymphoma and exceptionally (v) PLPN [4]. However, none of these aspects have been previously described in HL to the best of our knowledge. Peripheral nervous system’s complications in HL are uncommon including subacute sensory neuropathy, brachial neuropathy and Guillain–Barre syndrome [5–7]. The mean age of 18 reported PLPN was 58 years (34–72 years), with a sex ratio male to female ~1 [3]. Our patient is younger than all the described cases (20 years old). The ulnar nerve location was reported in only two cases; where the sciatic nerve represented the most involved site [3]. On imaging, MRI is a useful tool for peripheral lymphoma diagnosis and follow-up [8]. However, MRI findings, including in our case, were non-specific [3]. The diagnosis remains on histology and immunohistochemistry. In extranodal forms, especially in patients with no previous history of HL, the diagnosis is based on recognition of typical ‘diagnostic’ cells and appropriate phenotypic markers. Classical HL shows isolated neoplastic cells varying in number and in form (typical Hodgkin cells, Reed-Sternberg cells and lacunar cells). These cells are found within an inflammatory background, which differs according to histological subtype (nodular sclerosing, lymphoid rich, mixed cellularity and lymphocyte depleted) [10]. On immunohistochemistry, neoplastic cells are positive for CD30 (98% of the cases), CD15 (up to 90% of the cases), Pax 5 (weak) and mum1. CD45, EMA and BCL6 are usually negative. B and T cell markers might be positive in a proportion of cases that are usually EBV negative, especially CD20 which shows weak and heterogenous expression in up to 40% of cases [9, 10]. In our case, tumoral cells showed typical HL phenotype. The differential diagnosis of CHL includes nodular lymphocyte predominant HL, diffuse large B cell lymphoma and anaplastic large T-cell lymphoma. IHC is the most reliable tool to rule out these diagnoses [10]. Treatment in previously reported cases of non-Hodgkin PLPN consisted of complete/ partial excision of the tumor, or just biopsies, followed by various protocols of chemotherapy and or radiotherapy [3]. In HL, combination chemotherapy followed by involved-field radiation is the treatment of choice in patients with extranodal disease [10]. Up to present, no standard efficient treatment protocol has been clearly identified for patient with primary HL of peripheral nerve [3, 4]. There is a need for a further understanding of its biology and for a documenting these rare cases to find efficient treatment protocols. Our patient had a surgical excision of the mass and was referred to hematology department for chemotherapy without local radiotherapy, or CNS prophylaxis. The follow-up period is too short (2 months) to evaluate the outcome and the progression of the disease.
AUTHORS’ CONTRIBUTIONS
All authors read and approved the final manuscript.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no competing interests.
FUNDING
None.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Obtained.
CONSENT FOR PUBLICATION
Obtained.



