-
PDF
- Split View
-
Views
-
Cite
Cite
Carlos Castillo Amaya, Jose Antonio Prieto Meré, Andres Cobar Bustamante, Rudolf Mauricio Herrera Ovalle, Francisco Alonzo, Stab injury to the spine without neurological involvement: a report of a rare case, Journal of Surgical Case Reports, Volume 2021, Issue 5, May 2021, rjab163, https://doi.org/10.1093/jscr/rjab163
Close - Share Icon Share
Abstract
The annual incidence of traumatic spinal cord injury worldwide is 35 patients per million; this incidence is likely to be much higher in Latin America, where stab injuries are a common incidence. Stab injuries to the spine represent a small percentage of these cases; these are rare injuries; its management may differ compared with other penetrating injuries; these injuries are frequently complicated with neurological damage; the most common clinical manifestation is Brown–Sequard syndrome, and the most common segment involved is the thoracic region; stab injuries to the lumbar spine are rarely found in the literature. The management of patients without neurological involvement is controversial due to the risk of neurologic deterioration intraoperatively. However, failure to adequately intervene increases the risk of permanent neurological deficit, worsening functional outcomes, cerebral fluid leakage and infections. A short review of the literature and a case report are presented.
INTRODUCTION
The annual incidence of traumatic spinal cord injury is 35 patients per million. Nonmissile penetrating spinal injuries commonly occur in the thoracic region; this is explained by the defensive position the victim assumes when being attacked [1]. In 1977 Peacock et al. [2] analyzed 450 patients admitted for penetrating spinal trauma, up to 76% had neurologic deficit. There are also several reported cases with injuries to the paraspinal cord region without neurologic deficit [3]. The management of patients without neurologic deficit is controversial, due to the risk of neurologic deterioration intraoperatively. However, failure to adequately intervene increases the risk of permanent neurological deficit, functional outcomes, cerebral fluid leakage and infections [4].
CASE REPORT
A 21-year-old man arrived at the emergency room with a stab wound in the lumbar spine after alleged subjects attacked him 30 minutes prior to his arrival. Patient was alert and oriented, normotensive, in prone position with a knife projecting through his lumbar spine and a stab wound of ~3 cm (Fig. 1). Physical examination evidenced normal muscular strength, sensitivity, reflexes and pulses; rectal tone was intact. Lumbosacral radiographs were obtained (Fig. 2).

A stab wound of ~3 cm is described, at the lumbar portion of the patient’s spine, with a knife blade projecting from the wound. No active hemorrhage was seen.
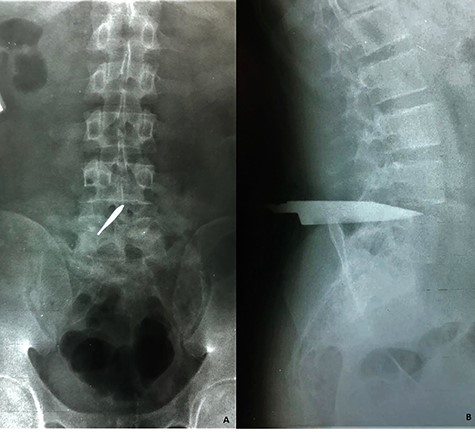
Lumbosacral radiographs were obtained revealing a foreign object compatible with a knife blade. (A) Anteroposterior view reveals the object placed within the L4–L5 intervertebral space involving the medullary canal and (B) lateral view shows the object that travels form posterior to anterior up to the L4–L5 intervertebral disc. No evidence of vertebral fractures nor free air were evidenced.

A right-sided L4–L5 laminectomy was performed for a total extraction of the knife blade. (A) Knife blade placed at the L4–L5 intervertebral space, at the right side from the spinous process and (B) shows the total extraction of the knife blade.
Prophylactic antibiotics were administered, and wound irrigation was performed at his immediate arrival; afterward, the patient underwent surgery, performing a right-sided L4–L5 laminectomy to extract a 12-cm stainless steel knife blade (Figs 3 and 4). A posterior dural tear was identified at the site of the extraction, which was repaired with a primary closure with nonabsorbable suture; the posterior ligamentous complex of the L4–L5 segment was intact (Fig. 5).


Postoperatively, neither signs of neurological dysfunction, nor drainage of cerebrospinal fluid were present. Dynamic radiographs discarded instability at the lumbar spine. A 3-day course of antibiotics was administered before discharge.
In the third month of follow-up visit, surgical wound was completely healed without signs of infection nor cerebrospinal fluid leakage; neurological examination remained normal; a standard postoperative magnetic resonance was obtained (Fig. 6).
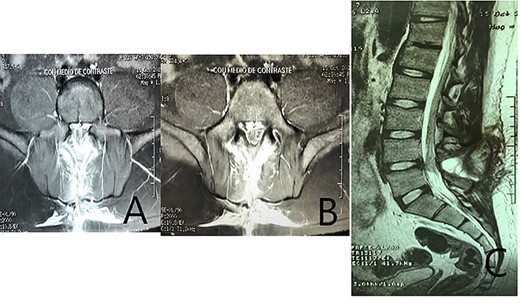
A standard postoperative magnetic resonance imaging. (A–B) coronal T2 images show a posterior cumulus of fluid that seems to connect the epidural space with the subcutaneous tissue, at the L4–L5 space, related to the laminectomized level. (C) Sagital T2 image demonstrating a posterior cumulus of fluid at the L4–L5 space; no changes in the L4–L5 disc compared with adjacent levels, and scar tissue is visible within the dural sac. The image is highly suspicious of cerebrospinal fluid leakage; the origin of the leakage whether from the anterior or posterior surface of the dural sac is not clear.
After a 1-year follow-up, the patient remained well.
DISCUSSION
Knife injuries to the spinal cord are infrequent and presented as case reports through the literature. Although relatively uncommon, several cases have been reported of penetrating thoracic trauma with extradural spinal cord involvement without neurological deficit [1–3].
It is of outmost importance to rule out associated injuries at the arrival of these patients, which would require urgent management before starting the diagnostic workup of the spinal stab wound [2, 3].
The diagnostic approach should start with plain radiographs to detect the presence of retained metal fragments. This is especially important before performing a magnetic resonance imaging. Plain radiographs can also detect fractures and presence of free air [5].
Dynamic X-rays assess spinal stability; however, its use in emergency situations is controversial. Computed tomography is the preferred study in the emergency department. It provides information about spinal stability, bone injury, wound trajectory and involvement of vital structures; it is an invaluable tool to assess the integrity of vessels, viscera or the presence of other life-threatening injuries [5, 6].
Magnetic resonance imaging can trace the path of the blade in soft tissues and bony structures, detect intraspinal hemorrhage or edema and spinal cord contusions. Initial images may detect an intradural or intraspinal hematoma with signs of compression (requiring urgent surgical evacuation) or a complete cord transection. T2-wighted fat-saturated and STIR sequences are recommended to identify dural injuries and ligament or neural disruptions [7].
In any case magnetic resonance imaging is contraindicated, the presence of progressive neurological deterioration or no response to conservative therapy mandates a myelography as the study of choice [8].
Management of penetrating spinal cord trauma depends on the mechanism and duration of injury. Penetrating traumas, such as stab wounds, present rates of significant neurologic recovery in up to 61% of patients [2]. Early and adequate surgical intervention is critical to improve neurologic outcomes. In contrast, surgical intervention for low-velocity penetrating bullet injuries does not improve long-term neurologic outcomes. However, early surgical intervention decreases the rate of infection, cerebrospinal fluid leakage and arachnoiditis in these patients [5, 6].
The essential components of management must involve careful positioning and transferring of the patient (in prone position). The technical components of surgical intervention include identifying the location and spinal level of the foreign object, surgical decompression, object removal in the line of the original trajectory and dural repair with collagen matrix or direct primary repair [6].
After knife blade removal, significant cord swelling may exist, mainly in the T7–T8 region, because of the presence of the vascular watershed area of the spine; a direct closure of the dura reduces the space available to accommodate the edema and could cause secondary injury and should not be performed in this region. Collagen Matrix Graft (Duragen Re-seal, Integra Life Sciences) may be used to seal the dural leak; recent studies have demonstrated the use the collagen matrix as an effective way to manage dural tears without sutures when necessary [9].
In our patient, we suspected the presence of a dural tear in the anterior and posterior aspect of the dura, considering the trajectory of the knife blade that involved the L4–L5 intervertebral disc. During surgical exploration we were only able to perform a direct repair of the posterior tear, and we decided to treat the anterior tear with the use of a collagen matrix substitute, due to the fact that it presented no apparent leakage after repeated Valsalva maneuvers, and we had no direct vision of it through a posterior approach. After surgery and recovery, the patient had no mechanical axial pain, and the dynamic X-rays obtained showed no instability; therefore, performing a second stabilizing surgery was ruled out. The magnetic resonance imaging after 3 months showed images compatible with cerebrospinal fluid leakage that after a 1-year follow-up resulted in no clinical deterioration.
CONCLUSIONS
In a patient with a nonmissile penetrating spinal cord injury with a retained foreign object and no neurologic deficit, the author recommends careful positioning (prone positioning), surgical decompression with laminectomy and removal of the foreign object in the original trajectory path and repair of the dural tear with or without sutures to avoid further cerebrospinal fluid leakage.
CONFLICT OF INTEREST STATEMENT
The authors declare that there is no conflict of interests.



