-
PDF
- Split View
-
Views
-
Cite
Cite
Victoria J Grille, David You, Seth Kipnis, Endoscopic sleeve gastroplasty requiring conversion to partial gastrectomy with paraesophageal hernia repair, Journal of Surgical Case Reports, Volume 2021, Issue 5, May 2021, rjab149, https://doi.org/10.1093/jscr/rjab149
Close - Share Icon Share
Abstract
Endoluminal bariatric surgery has lower costs and perceived risks compared to traditional surgery. Endoluminal procedures are a newer approach to weight loss but long-term outcomes and complications continue to emerge. This case report is an endoscopic sleeve gastroplasty that resulted in a paraesophageal hernia repair with removal of gastroplasty sutures and partial gastrectomy.
INTRODUCTION
Endoluminal bariatric surgery is an alternative treatment due to the potentially lower costs and risks. However, due to the paucity of research, it is difficult to compare the outcomes of endoluminal versus laparoscopic approaches to weight loss surgery. Outcomes for endoscopic sleeve gastroplasty (ESG) are still being studied, and complications are continuing to emerge. Our case will discuss an ESG that resulted in the patient requiring a paraesophageal hernia repair with removal of gastroplasty sutures and partial gastrectomy.
CASE
The patient is a 49-year-old female with a BMI of 31 kg/m2 that presented with worsening dysphagia, pain, heartburn, and progressively worsening nausea and vomiting since her ESG. She underwent an ESG one-year prior with intragastric plication sutures, however, did not follow up with her surgeon. Associated symptoms had inadequate relief with smaller meals and proton pump inhibitors. Of note, her symptoms did not include weight loss.
She underwent an upper gastrointestinal series that showed a normal-appearing stomach without any evidence of her prior gastroplasty, moderately sized hiatal hernia and slight delay in passage of contrast through the gastroesophageal junction (Fig. 1). On subsequent endoscopy, she was noted to have multiple loosely placed sutures within the gastric lumen along the greater curvature (Fig. 2), as well as a large-sized paraesophageal hernia.
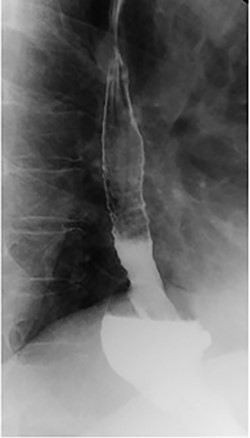
Barium swallow showing hiatal hernia postendoscopic gastroplasty.

Intraoperative endoscopy showing loose gastroplasty sutures along the greater curvature of the stomach.

Preoperative endoscopy (post gastroplasty) showing the body of the stomach without restrictive sleeve appearance.
Patient subsequently underwent a robotically assisted laparoscopic paraesophageal hernia repair with mesh, partial gastrectomy with removal of gastric foreign bodies, and flexible endoscopy. Intraoperatively via initial laparoscopic approach, there was only noted to be small dimples along the greater gastric curve without any noticeable plication (Fig. 3). The stomach was twisted up into the hiatal hernia. Multiple permanent sutures with T-fasteners were seen on endoscopy, and attempts were made to remove these endoscopically without success. These sutures were not of full thickness, so a gastrotomy was made to remove them. Partial gastrectomy was performed, including the fundus. The diaphragm was repaired with interrupted silk sutures and reinforced with a bioabsorbable mesh. The patient recovered well and was discharged home on postoperative day two tolerating a diet. She was seen at follow-up with complete resolution of her preoperative symptoms.
DISCUSSION
Bariatric surgery requires a multidisciplinary approach with an intensive preoperative and postoperative course. These patients are expected to adhere to preoperative and postoperative care, including long-term follow-up. Although ESG is considered a ‘non-surgical’ approach to weight loss, patients should still undergo the standard bariatric multidisciplinary approach.
ESG was first reported in 2013, and the other endoluminal bariatric therapies include an intragastric balloon, endoscopic bypass and endoscopic gastroplasty. These procedures may have lower costs and fewer risks compared to laparoscopic surgery. However, this is a new procedure and its complications may be under-reported in the literature. In addition, patients may not seek medical care at the same facilities or practices. This allows for flaws with currently published studies.
ESG has been described as having the advantages of maintaining anatomic structure and potential reversibility and is repeatable [1]. ESG reported total body weight loss of 14.9–15.2% at 6 months with low rates of adverse events (2–2.7%) [2, 3]. However, laparoscopic sleeve gastrectomy (LSG) demonstrates total body weight loss of 24% in 6 months. At the 1-year mark, these differences become less apparent per Novikov et al., with comparable weight loss only in the BMI < 40 kg/m2 group between ESG and LSG [4]. In terms of the reversibility of ESG, our case showed that this was not achievable and required a gastrectomy due to the inability to remove the sutures endoscopically.
Studies have also shown lower rates of adverse events with ESG. These events include perigastric leaks, perigastric inflammation, hemorrhage, pneumoperitoneum, pneumothorax and pulmonary embolism. This is compared with LSG, where major adverse events are as high as 5% [5], with perigastric leak being the most dreaded complication. However, newer advancements in technology and technique have reduced the leak rate to less than 1% [6].
Lopez-Nava et al. also describes the importance of technique and training when performing these advanced endoscopic procedures, specifically, intraoperative bleeding in 10% of their cases. They suggest the learning curve to be approximately 5–15 procedures but based on Watson et al. that the learning curve may require 50 procedures or more [7]. The rate of procedure failure for ESG has been reported to be greater than 50% with loose sutures requiring reoperation [8]. This is related to the failure of full-thickness suturing, as was depicted in our patient. Our upper gastrointestinal series failed to show the normal tubular appearance of the stomach after an ESG.
A paraesophageal hernia is contraindicated in an ESG and likely contributed to the failure. It is possible that the restriction created by the hernia made it difficult to ensure full-thickness sutures during the initial ESG. The operative report before the placement of the sutures stated that there was no hiatal hernia present; however, no other diagnostic imaging was done prior. This questions whether the hiatal hernia was present before the ESG or was a complication of the procedure. For the latter, we wanted to raise awareness of this potential complication. We recommend that ESG should be avoided in patients with a hiatal hernia due to the high likelihood of failure.
CONFLICT OF INTEREST STATEMENT
None.
FUNDING
None.
ETHICAL STATEMENT
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.



