-
PDF
- Split View
-
Views
-
Cite
Cite
Krystal Dinh, Lucy Manuel, Miles Somers, Mauro Vicaretti, Vascular tracheobronchial compression syndrome secondary to contained ruptured thoracic aortic aneurysm, Journal of Surgical Case Reports, Volume 2021, Issue 5, May 2021, rjab147, https://doi.org/10.1093/jscr/rjab147
Close - Share Icon Share
Abstract
Vascular tracheobronchial compression syndrome is the compression of the trachea or pulmonary bronchus by a vascular structure. It is primarily a diagnosis in children and secondary to congenital vascular anomalies. In adults, vascular tracheobronchial compression syndrome can be either congenital or required with a vast majority of congenital conditions found incidentally on imaging. Acquired conditions are largely due to aortic arch aneurysms or kinking of the aorta. The case described herein illustrates the rare case of a saccular thoracic aneurysm causing compression of the left primary bronchus. Patients may have a history of gradual onset of symptoms involving both the airway and oesophagus. Vascular tracheobronchial compression syndrome may go undetected and asymptomatic throughout an individual’s lifespan, however as described herein this syndrome may also be life-threatening.
INTRODUCTION
Vascular tracheobronchial compression syndrome is the compression of the trachea or pulmonary bronchus by a vascular structure. It can be both acquired and congenital. Vascular tracheobronchial compression syndrome may go undetected and remain asymptomatic throughout an individual’s lifespan, however as described herein this syndrome may also be life-threatening.

Chest X-ray illustrating complete collapse of the left lung lobe.
CASE REPORT
A 40-year-old man presented to the emergency department with sudden onset dyspnoea and severe chest pain radiating to his back. He also reports a year history of intermittent haemoptysis. On presentation, the patient’s observations were stable. The patient was born and raised in Tibet, and reported having previously been treated for confirmed tuberculosis.
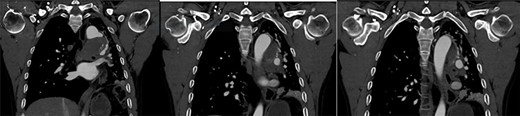
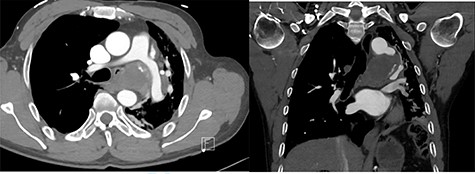
On presentation, chest X-ray illustrated a prominent proximal descending thoracic aorta contour and a completely collapsed left lung (Fig. 1). On computed tomography angiogram (CTA), the patient was found to have a large saccular aneurysm measuring 5.0 × 5.0 × 5.0 cm in size, arising from a focal location of the proximal descending thoracic aorta distal to the origin of the left subclavian artery with evidence of contained rupture (Fig. 2). The mass was found to be causing significant external compression of the left main bronchus leading to significant effacement of the left main primary bronchi leading to extensive collapse in both left upper and lower lobes and overall reduction in volume of the left hemithorax (Fig. 3).
After review by both the vascular and cardiothoracic surgeons, a decision was made to proceed to an open repair. A thoracic stent graft was considered, however this procedure would not relieve the patient’s bronchial compression. An open repair would exclude the thoracic aneurysm and also relieve compression from the bronchus. Without ventilation of the left lung, an extended posterolateral thoracotomy was performed to allow pleural entry via the fifth intercostal space. The distal aortic arch was encroached and the saccular aneurysmal portion at the inferior aspect at the distal inner curvature appreciated. The patient was placed on Cardiopulmonary Bypass (CPB), via the Common Femoral Artery and Common Femoral Vein, and the patient was cooled to 20°C. Peri-aortic tissue was dissected free of the target site; the recurrent laryngeal nerve was not observed however suspected medial to the dissection area. The saccular aneurysm was opened and old clot was evacuated and the area dissected to its neck at the inferior arch. Nil communication with the bronchus was evident. Remaining aorta appeared relatively normal. The edges of the aneurysm neck were fashioned towards health aorta and the resulting defect closed primarily with a single layer of bilaterally buttressed (bovine pericardial strips). CPB was recommenced to allow de-airing via the then closed anastomosis; with full CPB flow rewarming was begun. Sinus rhythm reverted spontaneously at 32°C; at normothermia the CPB wean was commenced, well tolerated and completed at the patient decannulated and protamine administered. Pleural packing was perused to allow haemostasis which was eventually achieved. Left lung recruitment achieve eventual satisfactory re-expansion. Drains were placed as the ribs re-approximated with double figure 8.
Post-operatively, the patient experienced intermittent episodes of desaturation secondary to mucous plugging. The patient required regular chest physiotherapy, high flow nasal prongs for humidification with intermittent bi-level positive airway pressure. He also developed a hospital-acquired pneumonia which was subsequently treated with a course of intravenous tazocin.
Repeat CTA illustrated good flow through the thoracic aneurysm, re expansion of the left lung, and decompression of the left main bronchus. Histopathology of washing and fine needle aspirates was all negative for tuberculosis and bacteria. Histopathology revealed fibroid and necrotic material with mixed acute and chronic inflammatory changes, fragments of benign bronchial epithelium and ulceration and squamous metaplasia; no granulomas were present. Further, nil malignancy was detected.
DISCUSSION
Vascular tracheobronchial compression syndrome is the compression of the trachea or pulmonary bronchus by a vascular structure. It is primarily a diagnosis in children and secondary to congenital vascular anomalies [1, 2]. In adults, vascular tracheobronchial compression syndrome can be either congenital or required with a vast majority of congenital conditions found incidentally on imaging. Acquired conditions are largely due to aortic arch aneurysms or kinking of the aorta [3]. The case described herein illustrates the rare case of a contained ruptured saccular thoracic aneurysm causing compression of the left primary bronchus. The primary cause for the contained rupture was originally thought to be from a tuberculosis mycotic aneurysm, however after extensive work and multiple tissue samples tuberculosis was not the primary cause. With no history of major trauma, hypertension or connective tissue disorders, it remains unknown to why the patient had developed a thoracic arch aneurysm. Patients may have a history of gradual onset of symptoms involving both the airway and oesophagus. Vascular tracheobronchial compression syndrome may go undetected and asymptomatic throughout an individual’s lifespan, however as described herein this syndrome may also be life-threatening.
CONFLICT OF INTEREST STATEMENT
None declared.



